Translate this page into:
Pregnancy-associated neutrophilic figurate erythema
Corresponding author: Dr. Jau-Yu Liau, Department of Pathology, National Taiwan University Hospital and National Taiwan University College of Medicine, and Graduate Institute of Pathology, National Taiwan University College of Medicine, Taipei, Taiwan. 019188@ntuh.gov.tw
-
Received: ,
Accepted: ,
How to cite this article: Kuo YW, Liau JY. Pregnancy-associated neutrophilic figurate erythema. Indian J Dermatol Venereol Leprol 2022;88:99-101.
Sir,
Neutrophilic figurate erythema is a rare inflammatory dermatosis of unknown etiology. It usually presents as annular or polycyclic erythematous lesions with histopathological feature of predominant neutrophilic infiltrate.1 Herein, we report a case of neutrophilic figurate erythema in a pregnant woman with onset of symptoms in the third trimester and spontaneous resolution after delivery.
A 46-year-old primigravida of 32 weeks gestation presented with a two-week history of itchy skin eruptions on her lower limbs. She was otherwise healthy without fever, chills, malaise or arthralgia. There was no history of insect bite, systemic diseases or new medication usage. She had been treated with topical corticosteroid and oral antihistamine without clinical improvement. Physical examination revealed multiple erythematous and purpuric arciform plaques with peripheral scales on her lower limbs [Figure 1a]. Some of the rashes on her left calf became indurated and tender which later developed pustules [Figure 1b]. Laboratory studies revealed a normal complete blood count, electrolytes, liver and renal function and complements levels (C3 and C4). Antinuclear antibody and anti-extractable nuclear antigen antibodies (Ro/ SS-A, La/SS-B, Scl-70 and Jo-1) were negative.

- Erythematous arciform plaques with peripheral scales on the left thigh
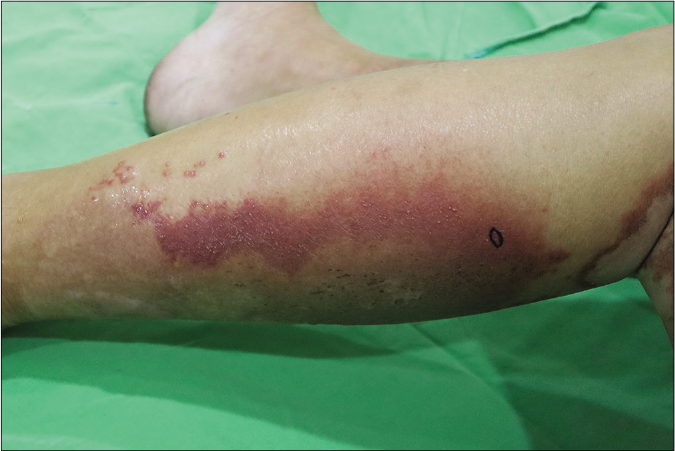
- Plaques with pustules on the left calf. Biopsy site is marked.
Histopathological examination revealed superficial perivascular and interstitial infiltration of lymphocytes and numerous neutrophils. Papillary dermal edema and erythrocyte extravasation were present without any evidence of vasculitis. Mild epidermal spongiosis and subcorneal pustules were also visible with a negative periodic acid-Schiff stain [Figures 2a and 2b]. Direct immunofluorescence was negative for immunoglobulin G, immunoglobulin A, immunoglobulin M, complement three and fibrinogen deposition. Based on the clinical and histopathological findings, neutrophilic figurate erythema was diagnosed. The patient received oral prednisolone (15 mg/day) and topical fluocinonide cream (0.05%) for two weeks and showed a significant clinical improvement. At 38 weeks of gestation, she gave birth to a healthy baby by cesarean section. The rashes gradually resolved postpartum without further treatment [Figure 3]. No recurrence was observed during one year after delivery.
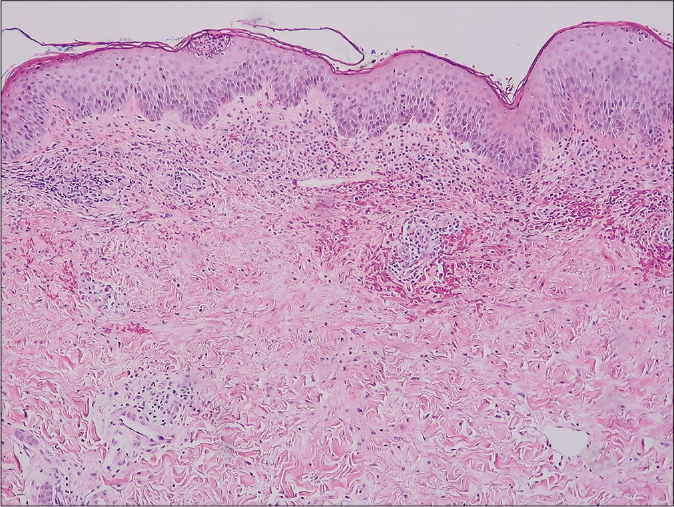
- Subcorneal pustule, perivascular and interstitial infiltrate in the upper dermis with erythrocyte extravasation and mild papillary dermal edema. (hematoxylin and eosin, ×100)
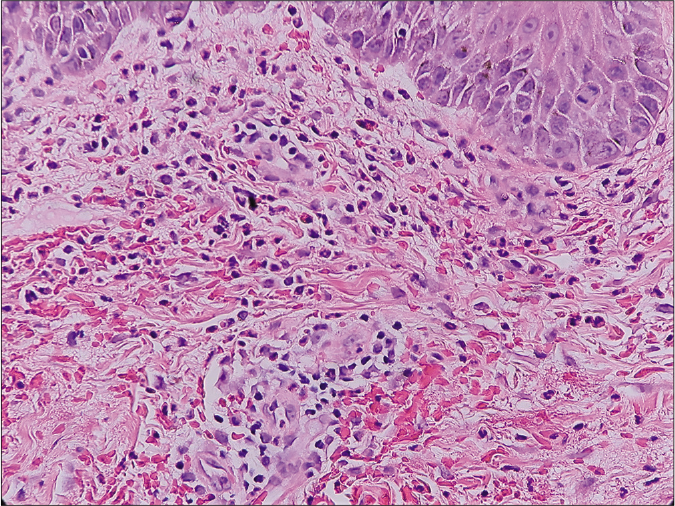
- The dermal infiltrate composed predominantly of neutrophils. (hematoxylin and eosin, ×400)
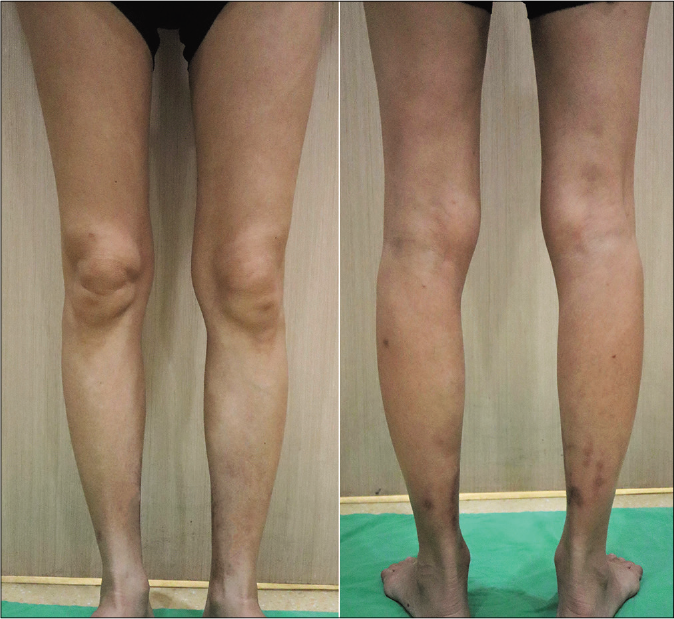
- Complete resolution of the rash postpartum
Neutrophilic figurate erythema is a rarely reported benign annular erythema with a clinical presentation similar to erythema annulare centrifugum. Histopathologically, predominant neutrophilic perivascular and interstitial infiltrate in the upper dermis, lack of vasculitis, and exclusion of other specific entities are crucial for diagnosis.2 There are no distinct triggers or direct association with major systemic disorders. We found two case reports of this entity associated with hematologic malignancies3,4 and another two cases induced by medication.2 Our patient appears to be the first reported case of pregnancy-associated neutrophilic figurate erythema, the pathogenesis of which is presently unclear.
Clinically, various inflammatory and infectious disorders presenting with annular erythema should be differentiated from neutrophilic figurate erythema, including subacute cutaneous lupus erythematosus, annular erythema of Sjögren’s syndrome, erythema annulare centrifugum, granuloma annulare, erythema chronicum migrans and tinea corporis. A correct diagnosis relies on a thorough history taking, laboratory studies and clinico-pathological correlation. Blister formation, purpuric changes and ring-shaped scales were observed in some patients in addition to annular erythema.2 However, none of the reported cases demonstrated arciform plaques with pustules, as seen in our patient. Impetigo herpetiformis or annular pustular psoriasis may also be considered in this case. Histopathologically, no typical features of psoriasis such as parakeratosis, Munro microabscess, spongiform pustule or dilated capillaries within the dermal papillae were found in our case.
The histological findings of neutrophilic figurate erythema need to be distinguished from other neutrophilic dermatoses. In particular, Sweet syndrome is characterized by more diffuse, deeper and denser neutrophilic infiltrate and prominent papillary dermal edema. Bullous systemic lupus erythematosus is marked by dermal neutrophilic infiltrate with leukocytoclasia, interface dermatitis and mucin deposition. Urticarial lesions of dermatitis herpetiformis or linear immunoglobulin A dermatosis usually show dermal papillary neutrophilic microabscesses.
A few cases of pregnancy-associated neutrophilic dermatoses have been documented in the literature. An alteration in the immune system during gestation might be a common factor. Pregnant women show a progressive neutrophilia due to increased levels of pro-inflammatory factors (e.g., granulocyte colony-stimulating factor and T helper-17), which may lead to neutrophil hyper-reactivity.5
We present a peculiar case of pregnancy-associated neutrophilic figurate erythema with a unique clinical feature of tender arciform erythematous plaques with pustules. While dealing with similar cases, extensive laboratory studies and skin biopsy are required to exclude other serious autoimmune and infectious disorders or associated malignancies. The treatment regimen for neutrophilic dermatoses may be followed to control the symptoms. Since this disease tends to run a benign course, clinicians should weigh benefits and risks before treating pregnant patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Neutrophilic figurate erythema recurring on the same site in a middle-aged healthy woman. Indian J Dermatol Venereol Leprol. 2012;78:505-8.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophilic figurate erythema. Am J Dermatopathol. 2017;39:344-50.
- [CrossRef] [PubMed] [Google Scholar]
- Paraneoplastic neutrophilic figurate erythema. Br J Dermatol. 2007;156:396-8.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophilic figurate erythema of infancy associated with juvenile myelomonocytic leukemia. Actas Dermosifiliogr. 2015;106:431-3.
- [CrossRef] [PubMed] [Google Scholar]
- Pyoderma gangrenosum and pregnancy: An example of abnormal inflammation and challenging treatment. Br J Dermatol. 2016;174:77-87.
- [CrossRef] [PubMed] [Google Scholar]





