Translate this page into:
Asymptomatic solitary nodule over the left flank
Corresponding author: Dr Anupam Das, Department of Dermatology, KPC Medical College and Hospital, Kolkata, West Bengal, India. anupamdasdr@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Das PC, Kumar P, Das A. Asymptomatic solitary nodule over the left flank. Indian J Dermatol Venereol Leprol 2023;89:466-8.
A 30-year-old man presented with a solitary mass on the left flank, for the last three and a half years. Initially it was a pea-sized lesion, which gradually increased in size. Cutaneous examination revealed a solitary 2×2 cm solid non tender, non pruritic, rough surfaced hyperpigmented nodule on the left flank [Figure 1]. It was not fixed to the underlying tissue. There was no regional lymphadenopathy and no other mucocutaneous findings. Systemic examination was noncontributory. The nodule was excised and sent for histopathological examination. Biopsy showed a well-circumscribed diffuse dense and nodular proliferation of large cells with abundant pink staining cytoplasm with a small vesicular central nucleus. The cytoplasm was packed with pink staining granules of different sizes (0.5–2 microns). The neoplastic cells were packed closely in nodules and fascicles with compressed collagen in between them [Figures 2 and 3]. Overlying epidermis showed pseudocarcinomatous hyperplasia and the granules stained positive with periodic acid-Schiff [Figure 4]. Immunohistochemistry could not be performed due to logistic reasons.
Question
What is your diagnosis?

- Hyperpigmented nodule on the left flank
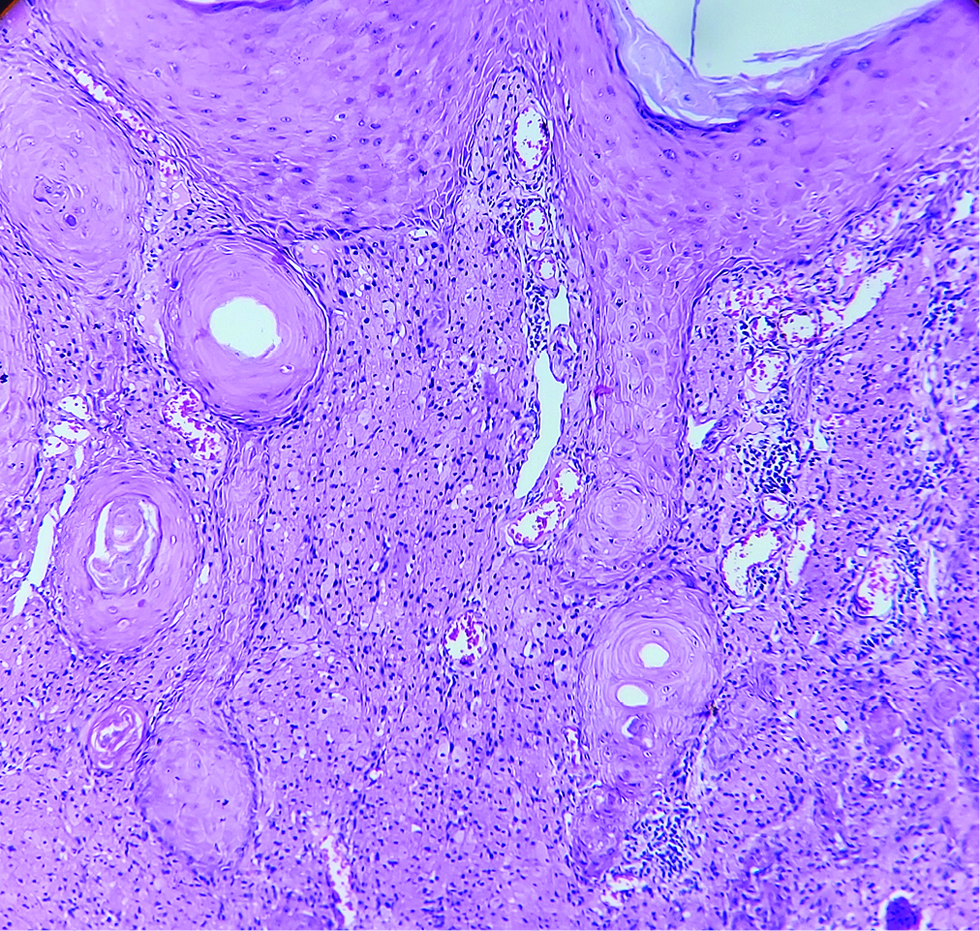
- Well-circumscribed diffuse dense and nodular proliferation of large cells (H and E, × 100)
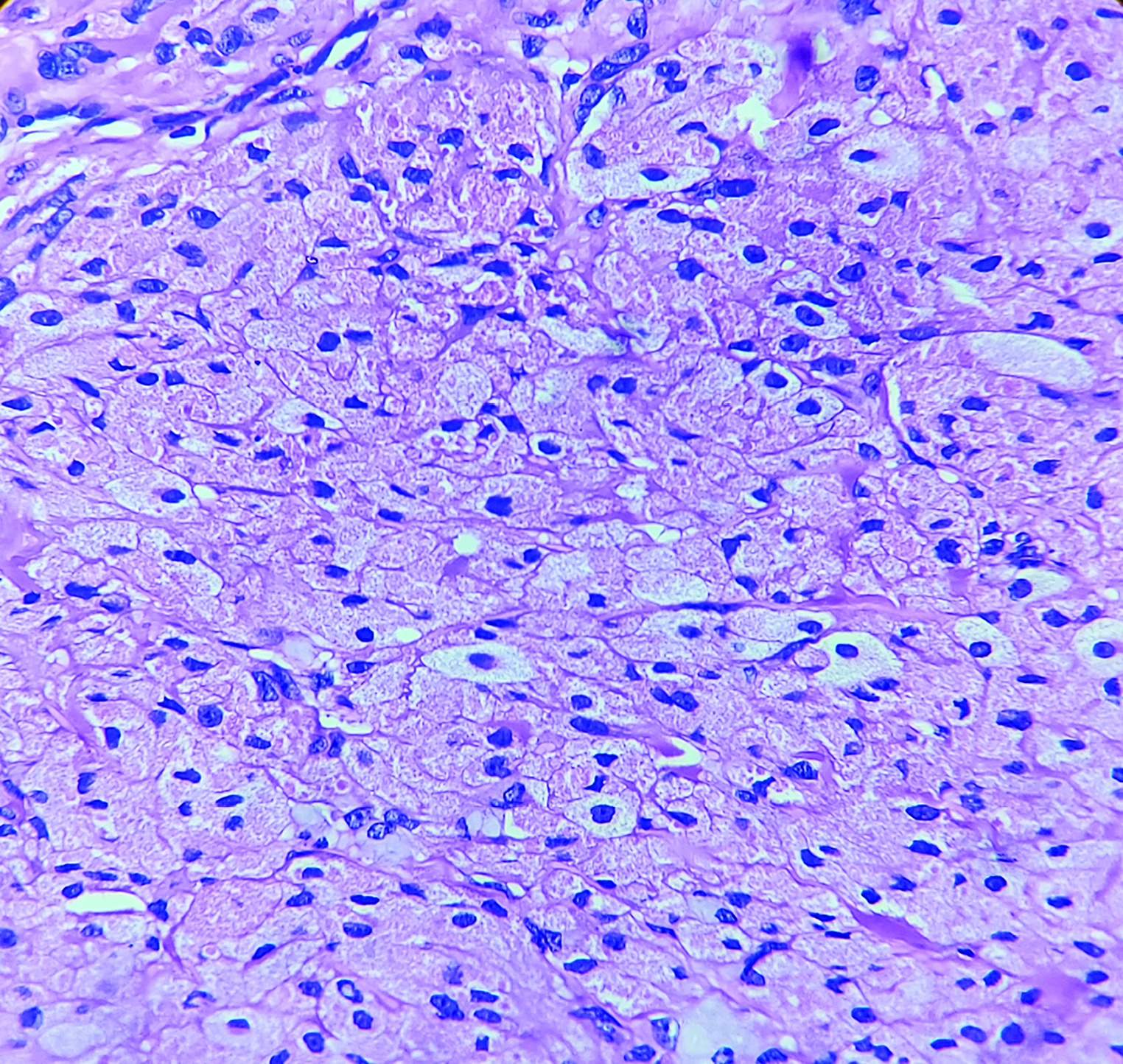
- Densely packed cells with abundant pink staining cytoplasm with a small vesicular central nucleus
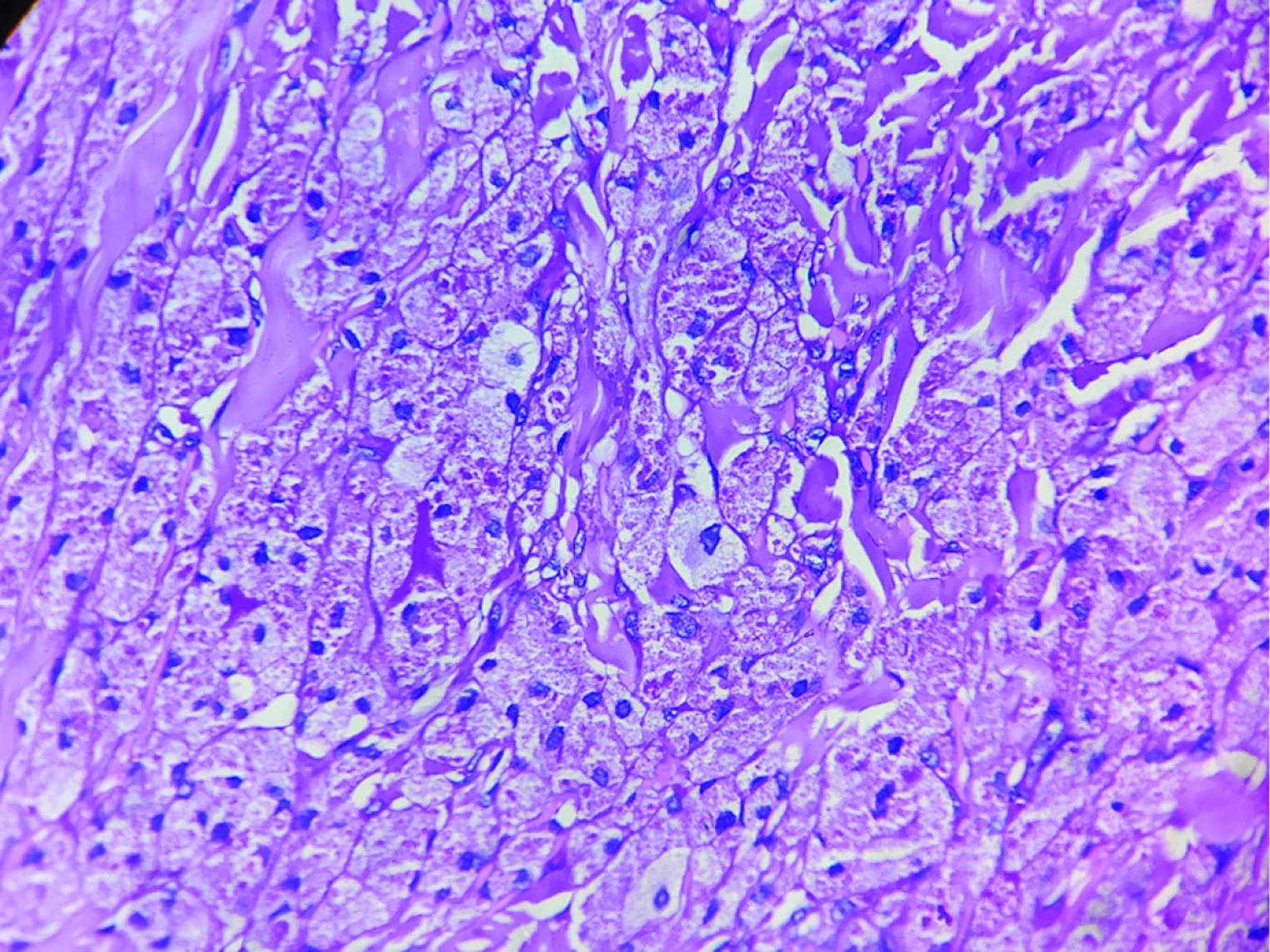
- Distinctly stained granules (PAS, × 400)
Answer
Granular cell tumour.
Discussion
A granular cell tumour is an uncommon benign neoplasm, originating from Schwann cells. The commonest site of involvement is the tongue, dermis and subcutaneous tissues. However, atypical sites of involvement have been reported like larynx, bronchus, uvea, oesophagus, stomach etc. There is no age predilection, and cases are more commonly seen in women. The lesions are usually solitary and painless, and in less than 25% of cases, multiple lesions have been noted. Rarely the tumour may be painful.1
Histopathology typically shows sheets of polygonal cells infiltrating into the dermis. The cells are typified by the presence of centrally placed small round to oval vesiculated nuclei with abundant granular eosinophilic cytoplasm. On immunohistochemistry, cells stain with vimentin, neuron-specific enolase, S-100, myelin protein, calretinin, nerve growth factor receptor five, microphthalmia-associated transcription factor, inhibin-alpha and protein gene product 9.5.2 LeBoit et al. and subsequently by others described rare subtypes: polypoid granular cell tumour and primitive non neural granular cell tumour which were S-100 negative.3 The granular appearance of the neoplastic cells is attributed to the presence of large lysosomes, which are positive for periodic acid–Schiff and diastase-resistant. Histological differentials include dermatofibroma, rhabdomyoma, Reed neuroid spindle cell tumour, xanthoma and metastatic breast carcinoma (all of them show granular cytoplasm on histology). Rarely, tumour cells in granular cell tumour may involve the overlying epidermis and distinction from melanoma may be difficult. HMB45 stain may help in differentiating the two conditions, which is usually negative in granular cell tumour.
Malignancy is uncommon (1–2%) and clinically it manifests with a rapid increase in size and locoregional lymph node enlargement. Spindling of neoplasic cells on histology is thought to be a marker of malignant transformation. Other features which suggest malignancy include an increased number of mitotic figures (>2 mitoses per 10 high-power fields), necrosis, pleomorphic nuclei, increased nucleocytoplasmic ratio and vesicular nuclei with prominent nucleoli.4 Presence of two of these criteria makes the tumour “atypical”, and granular cell tumours with three or more of these criteria are classified as malignant.5
The therapy of choice is complete excision with free surgical margins. Patients should be followed up periodically to look for recurrences.6
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Granular cell tumor: An uncommon benign neoplasm. Indian J Dermatol. 2015;60:322.
- [CrossRef] [PubMed] [Google Scholar]
- Granular cell tumor: a clinical study of 81 patients. Actas Dermosifiliogr (Engl Ed). 2021;112:441-6.
- [CrossRef] [PubMed] [Google Scholar]
- Primitive polypoid granular-cell tumor and other cutaneous granular-cell neoplasms of apparent nonneural origin. Am J Surg Pathol. 1991;15:48-58.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple asymptomatic lesions on the lips. Clin Exp Dermatol. 2019;44:316-8.
- [CrossRef] [PubMed] [Google Scholar]
- Histopathological features of granular cell tumor. Int Clin Pathol J. 2015;1:42-4.
- [CrossRef] [Google Scholar]
- A case of granular cell tumor with an interesting clinical course. Indian J Dermatol Venereol Leprol. 2012;78:193-5.
- [CrossRef] [PubMed] [Google Scholar]





