Translate this page into:
Uncommon variants of fixed drug eruption
Corresponding author: Dr. Anupam Das, Department of Dermatology, KPC Medical College and Hospital, Kolkata, West Bengal, India. anupamdasdr@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agarwal A, Das A, Panda M, Kumar P. Uncommon variants of fixed drug eruption. Indian J Dermatol Venereol Leprol 2023;89:475-81.
Fixed drug eruption is a fairly common dermatological condition, presenting to us. It is a distinct cutaneous allergic reaction, presenting as single or multiple hyperpigmented patches with an erythematous border appearing after exposure to the culprit drug. However, in many situations, the presentation is not classical and the diagnosis is often missed by clinicians. Herein, we provide a comprehensive list of uncommon variants of a fixed drug eruption. The drugs implicated are listed in [Table 1].
| 1. Psoriasiform fixed drug eruption | Nimesulide,1,2 ibuprofen3 |
| 2. Cellulitis-like fixed drug eruption | Topotecan,4 paracetamol5,6 |
| 3. Erythema dyschromicum perstans like fixed drug eruption | Theophylline7,8 |
| 4. Papular fixed drug eruption | Paracetamol9 |
| 5. Non-pigmenting fixed drug eruption | Cotrimoxazole,10 pseudoephedrine, tetrahydrozoline, piroxicam, thiopental, radio-opaque contrast media (iothalamate), diflunisal, ephedrine, prazinone, sorafenib, tadalafil, esomeprazole, triclofos sodium, betahistine, ibuprofen,11 acelofenac and fluoroquinolones12 |
| 6. Localised bullous fixed drug eruption | Nonsteroidal anti-inflammatory drugs (ibuprofen and mefenamic acid), antibiotics (doxycylline and cotrimoxazole),13 loxoprofen, mesalazine, levofloxacin, azithromycin, celecoxib, chlorthalidone, etoricoxib, etc. Human papilloma virus vaccine14 |
| 7. Generalised bullous fixed drug eruption | Antibiotics15,16 (metronidazole, trimethoprim sulfamethoxazole, rifampicin, ciprofloxacin,17 doxycycline and cefotaxime), analgesics (ibuprofen and naproxen), fluconazole, phenytoin, cetirizine, hydroxyzine, trazodone,18 radio-contrast dye19 and influenza vaccine20 |
| 8. Annular fixed drug eruption | Phenobarbitol21 |
| 9. Transitory giant fixed drug eruption | Allopurinol22 |
| 10. Erythema multiforme-like fixed drug eruption | Mefenamic acid23 |
| 11. Linear fixed drug eruption | Cephazolin, trimethoprim, levofloxacin,24 naproxen, azithromycin25 and carbamazepine26 |
| Based on location | |
| 1. Subungual fixed drug eruption | Sparfloxacin and amoxicillin27 |
| 2. Vulvar fixed drug eruption | Fluconazole, paracetamol and ibuprofen28,29 |
| 3. Wandering fixed drug eruption | Paracetamol30 and cotrimoxazole31 |
| 4. Oral mucosal fixed drug eruption | Cotrimoxazole (most commonly on dorsum of tongue), naproxen, mefenamic acid and ornidazole32,33 |
| Histopathological variants | |
| 1. Vasculitis-like fixed drug eruption | Paracetamol34 and ornidazole35 |
| 2. Neutrophilic fixed drug eruption | Amoxicillin-clavulinic acid, naproxen, cotrimoxazole, fluconazole, metronidazole,36 gabapentin37 and etoricoxib38 |
| Special variants | |
| 1. Chronic fixed drug eruption | Paracetamol39 |
| 2. Post-coital fixed drug eruption | Cotrimoxazole40,41,42,43 and paracetamol44 |
| 3. Fixed alcohol eruption | Ethanol and annexing agents of spirits such as aliphatic and aromatic hydrocarbons45 |
| 4. Fixed food eruption | Cashew nuts, almonds, walnut, pistachio, strawberry, kiwi and cheese crisps46 |
| 5. Fixed sunlight eruption | Ultraviolet rays |
The Uncommon Variants
Based on morphology
Psoriasiform fixed drug eruption: It presents as erythematous indurated slightly pruritic plaques with silvery-white scales with a definitive temporal correlation with drug intake.1-3 The pathomechanism postulated is triggering psoriasis through the Koebner phenomenon. Histology depicts features consistent with both psoriasis and drug eruption. The recurrence of similar morphology of lesion at same site following drug re-challenge helps in reaching a diagnosis [Figure 1].
Cellulitis-like fixed drug eruption: It presents as recurrent sudden onset ill-defined erythematous and oedematous plaques that develop following ingestion of culprit drug. The clinical picture resembles cellulitis but the lesions do not respond to conventional antibiotic therapy.4-6 The diagnosis requires a high degree of suspicion and usually, a similar eruption on re-administration of the drug raises suspicion of fixed drug eruption. Differential diagnoses include cellulitis, Wells syndrome and inflammatory metastatic carcinoma.
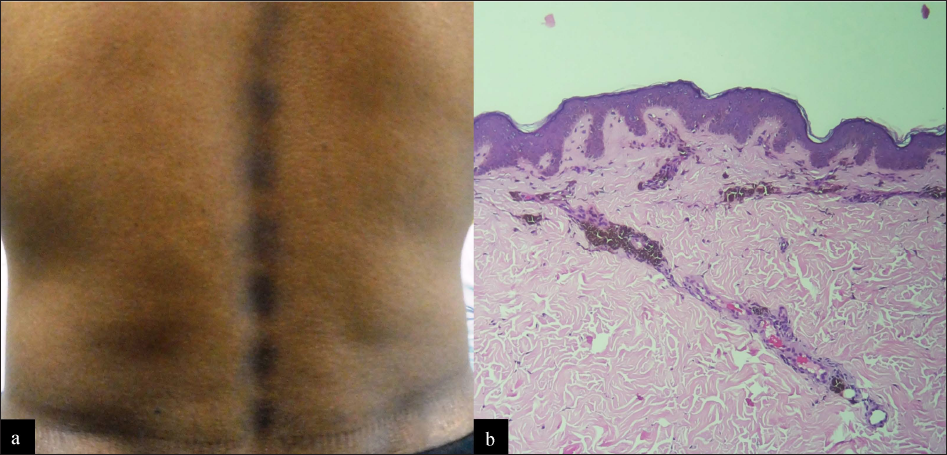
Erythema dyschromicum perstans-like fixed drug eruption: The patient presents with multiple violaceous plaques with erythematous borders which clinically resemble erythema dyschromicum perstans [Figure 2] but on careful questioning a history of the culprit drug is elicitable.7,8 Histopathological findings are suggestive of both erythema dyschromicum perstans and fixed drug eruption. Identification of intraepidermal T cells in basal and suprabasal keratinocytes of lesional skin on immunohistochemmistry are also a clue towards a diagnosis of fixed drug eruption in such cases.
Papular fixed drug eruption: The patient presents with recurrent episodes of erythematous papules affecting an area after ingestion of culprit drug. Histopathology and a strong index of suspicion are required to make a diagnosis.9
Non-pigmenting fixed drug eruption: The term was introduced by Shelly and Shelly. In this variant, large, symmetric erythematous lesions are seen on the axilla, buttock and inguinal regions which lack the post-inflammatory residual hyperpigmentation seen commonly after classical fixed drug eruption. Histopathologically, there is minimal lymphocytic infiltration in the epidermis, no epidermal necrosis and no pigment incontinence in contrast to classical fixed drug eruption.10-12
Localised bullous fixed drug eruption: A rare variant of fixed drug eruption that is characterised by red-brown patches with overlying bullae and/or erosion [Figure 3] and surrounding diffuse hyperpigmentation.13 Histopathology shows an intraepidermal split along with other classical features of a fixed drug eruption. Recently, a case of human papillomavirus vaccine-induced bullous drug eruption has also been described.14
Generalised bullous fixed drug eruption: It is a type of bullous fixed drug eruption presenting with widespread bullae and erosions [Figure 4] that are often confused with Steven-Johnson syndrome and toxic epidermal necrolysis.15-18 Differentiating features are tabulated in [Table 2]. Other differential diagnoses to be considered are pseudoporphyria, staphylococcal scalded skin syndrome and drug-induced autoimmune bullous dermatoses. Generalised bullous fixed drug eruption after the use of intravenous contrast and following influenza vaccination has also been described.19,20
Annular fixed drug eruption: Fixed drug eruption may rarely present as areas of annular erythema with violaceous hue and central clearing. History of preceding drug intake and recurrent episodes can help clinch the diagnosis21
Transitory giant fixed drug eruption: It presents as a single transient edematous plaque after ingestion of culprit drug unlike commonly occurring fixed drug eruption in multiple locations.22
Erythema multiforme-like fixed drug eruption: Multiple cases have been described wherein multifocal fixed drug eruption have masqueraded as erythema multiforme.23 The absence of residual pigmentation may also add to the confusion.
-
Linear fixed drug eruption: As the name suggests, in this unique variant of fixed drug eruption, lesions appear along a linear distribution.24-26 The linearity could be attributed to a dermatomal distribution, along lines of Blaschko, skin tension lines, or due to Wolf’s isotopic response after either herpes zoster, insect bites, or cellulitis.
Dermatomal or zosteriform fixed drug eruption: The commonly implicated drugs are cephazolin, trimethoprim, carbamazepine and levofloxacin24
Blaschkoid fixed drug eruption: most commonly caused by naproxen and trimethoprim
Non-dermatomal non-blaschkoid pattern of linear fixed drug eruption: reported with azithromycin [Figure 5]25
Linear bullous fixed drug eruption: caused by carbamezepine26
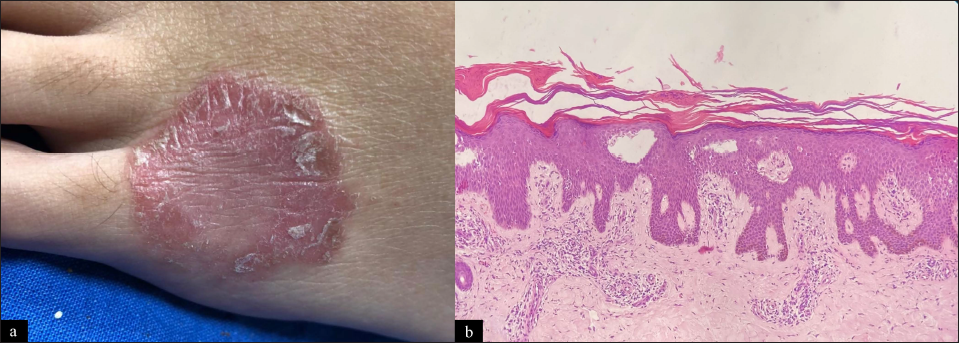
- Psoriasiform fixed drug eruption: (a) Single well-defined erythematous scaly plaque over dorsum of the left foot 12 days after ingestion of diclofenac tablet for tooth ache. Patch test carried out at same site four weeks after resolution was positive confirming diagnosis. (b) Hyperkeratosis with parakeratosis with acanthosis and regular elongation of rete ridges. Suprapapillary thinning and dilated capillaries in the papillary dermis (H and E, ×100)

- Erythema dyschromicum perstans-like fixed drug eruption: (a and b) Multiple violaceous plaques with erythematous borders present over trunk and back. History of recurrent episodes of eruption after ingestion of ofloxacin-ornidazole combination for loose stools was elicited. (c) Photomicrograph shows interface dermatitis with basal cell layer vacuolization. Marked pigmentary incontinence in the papillary dermis also present with mild inflammatory infiltrate (H and E, 100×)

- Bullous fixed drug eruption: Multiple bullae with surrounding erythema present over palm, dorsum of hand and trunk in a 35-year-old, two days after ingestion of azithromycin. The previous history of violaceous eruption after ingestion of azithromycin was present. Current episode led to bullous lesions

- Generalised bullous fixed drug eruption within 1 day after ingestion of ibuprofen tablet: (a) Areas of post inflammatory hyperpigmentation and erosions over the perineum, thighs and genitalia, (b) blisters and hyperpigmentation over genitalia and hands, (c) erosions, scaling and pigmentation over the back and buttocks and (d) blisters and pigmentation over the legs
| Generalised bullous fixed drug eruption | Stevens-Johnson syndrome-toxic epidermal necrolysis | |
|---|---|---|
| Onset from drug exposure | • Within hours | • 1-4 weeks |
| History of previous episodes | • Multiple episodes | • Absent |
| Mucosa | • Minimally involved | • Major involvement |
| Systemic involvement | • Minimal | • Definite |
| Mortality | • Low | • High |
| Serum granulysin | • Low | • High |
| Histopathology | • Necrotic keratinocytes with numerous macrophages and eosinophils and lowered granulysin positive cells | • More necrotic keratinocytes with minimal macrophages and eosinophils and increased granulysin positive cells |
- Linear fixed drug eruption: (a) Multiple hyperpigmented patches arranged in a linear distribution on the back of a patient. History of consumption of azithromycin tablet 20 days ago for sore throat was present. History of similar lesions after intake of azithromycin for acne vulgaris one year ago. (b) Photomicrograph depicts basal layer hyperpigmentation, mild interface dermatitis, pigment incontinence and perivascular infiltrate (H and E, ×100)
Based on location
Subungual fixed drug eruption: Nail pigmentation affecting few nails appearing on a recurrent basis after intake of a culprit drug should raise suspicion of subungual fixed drug eruption. Many drugs are known to cause nail pigmentation but, in that case, all nails are affected simultaneously.27
Vulvar fixed drug eruption: Fixed drug eruption involving the vulva may present as chronic erosive vulvitis or primarily as pruritus vulvae.28,29 Concomitant lesions in the skin and oral ulcers may give hint toward a diagnosis of fixed drug eruption along with the history of ingestion of culprit drug.
Wandering fixed drug eruption: As the name suggests, this variant of fixed drug eruption has lesions which tend to vary from one location to another with successive episodes. Classically only some lesions tend to be inflamed and many lesions turn refractory due to multiple episodes of drug re challenge.30,31 Pathogenesis implicated is increased frequency of drug administration due to patient being unaware of culprit drug and daily consumption for prolonged periods.
-
Oral mucosal fixed drug eruption:
Based on histopathology
Vasculitis-like fixed drug eruption: refers to fixed drug reaction presenting as purpuric lesions having a history of recurrent episodes and histopathologic finding of leukocytoclastic vasculitis.34,35 The differential diagnosis to be considered is urticarial vasculitis.
Neutrophilic fixed drug eruption: A recently described variant wherein the morphological presentation is that of fixed drug eruption with histopathological features of classical fixed drug eruption along with a perivascular and intestitial neutrophilic infiltrate in the dermis.36 There is still discordance concerning whether this represents an early phase in the histopathological progression of all fixed drug eruptions or it is a separate entity in itself. Histopathological differentials to be considered are Sweet’s syndrome, autoinflammatory urticaria and acute generalised exanthematous pustulosis. Generalised neutrophilic fixed drug eruption has been described due to gabapentin37 and etoricoxib.38
Special types
Chronic fixed drug eruption: Persistent stable lesions resembling parapsoriasis have been described in one report.39 The diagnosis was reached after seven months in the case after stoppage of culprit drug, which led to eventual clearance of the lesions with oral challenge test being positive.
Post-coital fixed drug eruption: A unique form of fixed drug eruption occurs in the male partner after sexual contact with a female on the culprit drug either orally or in local application. The male partner always has a known allergy to the culprit drug. Mode of contact with culprit drug occurs through vaginal fluid. Lesions can occur anywhere but typically involve the oral and genital mucosa. Drugs implicated are co-trimoxazole (oral40-42 and local application43 ) and paracetamol.44
Fixed alcohol eruption: History of recurrent fixed drug eruption at a similar site after consumption of a large bout of alcohol. No history of medications and allergies is elicitable. Implicated chemicals can be ethanol and annexing agents of spirits such as aliphatic and aromatic hydrocarbons.45
Fixed food eruption: presents as recurrent erythematous patches, bullae, vesicles or pustules at the same site after ingestion of the same or related food products. Pathomechanism is similar to that of fixed drug eruption. Residual antibiotics in food have also been reported to cause fixed drug eruption.46,47
Fixed sunlight eruption: Presenting as recurrent erythematous plaques appearing after sun exposure leaving behind hyperpigmentation. No other history of drugs, food is elicited.48,49
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Psoriasis koebnerization in a patient with fixed drug eruption. J Am Acad Dermatol. 2008;58:AB132.
- [CrossRef] [Google Scholar]
- Psoriasiform fixed drug caused by nimesulide. Clin Exp Dermatol. 2009;34:360-1.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasiform fixed-drug eruption to ibuprofen: A rare variant of fixed-drug eruption in a child. Indian J Paediatr Dermatol. 2021;22:96-8.
- [CrossRef] [Google Scholar]
- Topotecan-induced cellulitis-like fixed drug eruption. J Eur Acad Dermatol Venereol. 2002;16:414-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cellulitis-like fixed drug eruption attributed to paracetamol (acetaminophen) Dermatol Online J. 2005;11:24.
- [PubMed] [Google Scholar]
- Acetaminophen-induced cellulitis-like fixed drug eruption. Indian J Dermatol. 2011;56:206-8.
- [CrossRef] [PubMed] [Google Scholar]
- Periorbital hyperpigmentation mimicking fixed drug eruption: A rare presentation of erythema dyschromicumperstans in a paediatric patient. J Eur Acad Dermatol Venereol. 2006;20:1381-3.
- [CrossRef] [PubMed] [Google Scholar]
- Fixed drug eruption presenting as erythema dyschromicum perstans: A flare without taking any medications. Dermatology. 1998;197:383-5.
- [CrossRef] [PubMed] [Google Scholar]
- Papular fixed drug eruption mimicking folliculitis due to acetominophen. Clin Exp Dermatol. 2000;25:96-7.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral non-pigmenting fixed drug eruption associated with cotrimoxazole. Dermatol Online J. 2006;12:12.
- [PubMed] [Google Scholar]
- Non-pigmented fixed drug eruption caused by ibuprofen. Indian Dermatol Online J. 2019;10:341-3.
- [CrossRef] [PubMed] [Google Scholar]
- Non-pigmenting fixed drug eruption due to fluoroquinolones. Indian J Dermatol Venereol Leprol. 2017;83:108-12.
- [CrossRef] [PubMed] [Google Scholar]
- Azithromycin induced bullous fixed drug eruption. Indian J Pharmacol. 2016;48:83-5.
- [CrossRef] [PubMed] [Google Scholar]
- Bullous fixed drug eruption following human papilloma virus vaccination. J Eur Acad Dermatol Venereol. 2020;34:e697-8.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized bullous fixed drug eruption is distinct from Stevens-Johnson syndrome/toxic epidermal necrolysis by immunohistopathological features. J Am Acad Dermatol. 2014;70:539-48.
- [CrossRef] [PubMed] [Google Scholar]
- Fixed drug eruptions: An update, emphasizing the potentially lethal generalized bullous fixed drug eruption. Am J Clin Dermatol. 2020;21:393-9.
- [CrossRef] [PubMed] [Google Scholar]
- Doxycycline induced generalized bullous fixed drug eruption. Indian J Dermatol. 2016;61:128.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized bullous fixed drug eruption: Trazodone as a new culprit. Contact Dermatitis. 2020;82:192-3.
- [CrossRef] [PubMed] [Google Scholar]
- Contrast-induced generalized bullous fixed drug eruption resembling Stevens-Johnson syndrome. Proc (Bayl Univ Med Cent). 2019;32:601-2.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized bullous fixed-drug eruption secondary to the influenza vaccine. JAAD Case Rep. 2018;4:953-5.
- [CrossRef] [PubMed] [Google Scholar]
- Annular fixed drug eruption. J Dtsch Dermatol Ges. 2010;8:823-4.
- [CrossRef] [PubMed] [Google Scholar]
- Allopurinol induced transitory giant fixed drug eruption: An atypical expression. J Dermatol. 1999;26:198-9.
- [PubMed] [Google Scholar]
- Multifocal fixed drug eruption mimicking erythema multiforme. Clin Exp Dermatol. 1990;15:387-8.
- [CrossRef] [PubMed] [Google Scholar]
- Zosteriform fixed drug eruption to levofloxacin. Indian J Dermatol. 2012;57:327-8.
- [CrossRef] [PubMed] [Google Scholar]
- Azithromycin-induced linear fixed drug eruption: A rare instance. Indian Dermatol Online J. 2021;12:353-4.
- [CrossRef] [PubMed] [Google Scholar]
- Carbamazepine-induced linear and bullous fixed drug eruption representing Wolf’s isotopic phenomenon. Indian J Dermatol Venereol Leprol. 2021;87:402-4.
- [CrossRef] [PubMed] [Google Scholar]
- Sparfloxacin-induced nail pigmentation: A case of fixed drug eruption? Ann Afr Med. 2018;17:40-2.
- [CrossRef] [PubMed] [Google Scholar]
- Vulvar fixed drug eruption. A report of 13 cases. J Reprod Med. 2007;52:81-6.
- [PubMed] [Google Scholar]
- Vulval fixed drug eruption due to paracetamol. Australas J Dermatol. 2009;50:118-20.
- [CrossRef] [PubMed] [Google Scholar]
- Wandering fixed drug eruption: A mucocutaneous reaction to acetaminophen. J Am Acad Dermatol. 1987;17:399-402.
- [CrossRef] [PubMed] [Google Scholar]
- Drug related clinical pattern in fixed drug eruption. Eur J Dermatol. 2000;10:288-91.
- [PubMed] [Google Scholar]
- Oral mucosal fixed drug eruption: Characteristics and differential diagnosis. J Am Acad Dermatol. 2013;69:e51-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mucosal fixed drug eruption in a patient treated with ornidazole. J Dermatol Case Rep. 2012;6:21-4.
- [CrossRef] [PubMed] [Google Scholar]
- Vasculitis in a fixed drug eruption due to paracetamol. Br J Dermatol. 1995;133:790-1.
- [CrossRef] [PubMed] [Google Scholar]
- Image gallery: Purpuric fixed drug eruption from ornidazole showing leukocytoclastic vasculitis. Br J Dermatol. 2017;177:e164.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophilic fixed drug eruption: A mimic of neutrophilic dermatoses. Clin Exp Dermatol. 2019;44:236-8.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized neutrophilic fixed drug eruption induced by gabapentin. Turk J Phys Med Rehabil. 2021;67:122-4.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophilic generalized fixed drug eruption induced by etoricoxib. J Investig Allergol Clin Immunol. 2021;1:1.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic fixed drug eruption caused by acetaminophen. Cutis. 1988;41:106-8.
- [PubMed] [Google Scholar]
- Postcoital fixed drug eruption in a man sensitive to trimethoprim-sulphamethoxazole. Clin Exp Dermatol. 1997;22:144-5.
- [PubMed] [Google Scholar]
- Recurrent postcoital fixed drug eruption caused by co-trimoxazole mimicking a sexually induced disease. Our Dermatol Online. 2013;4:196-8.
- [CrossRef] [Google Scholar]
- Fixed drug eruption—a sexually inducible reaction? Int J STD AIDS. 2004;15:560-3.
- [CrossRef] [PubMed] [Google Scholar]
- Postcoital penile drug eruption in a co-trimoxazole-sensitive patient following vaginal use of triple sulfa vaginal cream by his partner. J Sex Med. 2012;9:758-60.
- [CrossRef] [PubMed] [Google Scholar]
- Postcoital fixed drug eruption: A rare pattern of fixed drug eruption. Indian J Drugs Dermatol. 2020;6:35-7.
- [CrossRef] [Google Scholar]
- Fixed drug eruption caused by drinking alcohol. Clin Exp Dermatol. 2019;44:68-70.
- [CrossRef] [PubMed] [Google Scholar]
- A cross-sectional observational study of clinical spectrum and prevalence of fixed food eruption in a tertiary care hospital. Indian Dermatol Online J. 2020;11:361-6.
- [CrossRef] [PubMed] [Google Scholar]
- Fixed drug eruption caused by antibiotics contained in food? Clin Exp Dermatol. 2019;44:944.
- [CrossRef] [PubMed] [Google Scholar]
- Fixed sunlight eruption: A case report. J Eur Acad Dermatol Venereol. 2016;30:894-5.
- [CrossRef] [PubMed] [Google Scholar]
- It is not a fixed drug eruption, it is a fixed “sunlight” eruption. Int J Dermatol. 2010;49:1421-3.
- [CrossRef] [PubMed] [Google Scholar]





