Translate this page into:
Acantholytic dyskeratotic acanthoma: A rare and underappreciated entity
Corresponding author: Prof. Chul Hwan Bang, Department of Dermatology, College of Medicine, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, South Korea, mrbangga@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Doh JY, Lee JH, Bang CH. Acantholytic dyskeratotic acanthoma: A rare and underappreciated entity. Indian J Dermatol Venereol Leprol 2023;89:904-7.
A 64-year-old man presented with a slightly painful plaque on the neck for 6–7 months [Figure 1a]. He had no other underlying disease except osteoarthritis and denied any family history of skin disease. Clinical examination revealed a 1.4 cm-sized erythematous-to-brownish crusted plaque on the neck. Dermoscopy findings showed a central mass of keratin surrounded by linear-irregular vessels [Figure 1b].

- A solitary, 1.4 cm-sized, erythematous to brownish plaque with crusts on the neck
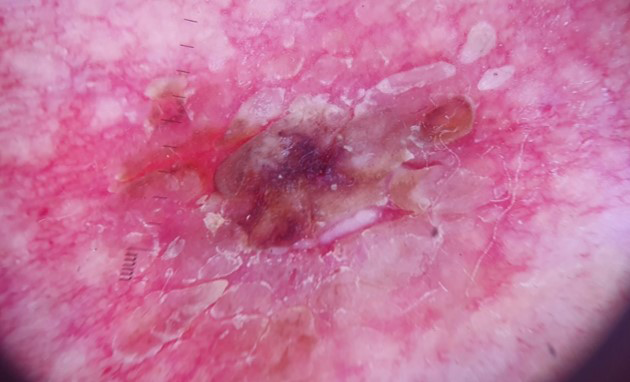
- Dermoscopy showed a central mass of keratin surrounded by linear-irregular vessels
An excisional biopsy was performed for treatment and diagnosis under suspicion of inflamed seborrheic keratosis, squamous cell carcinoma and basal cell carcinoma. Histopathological findings showed acanthosis, parakeratosis, dyskeratosis and acantholysis involving a full epidermal layer. Superficial perivascular lymphocytic infiltration in the dermis was present without follicular involvement [Figures 2a and 2b]. After excision, the lesion healed without a sign of recurrence.
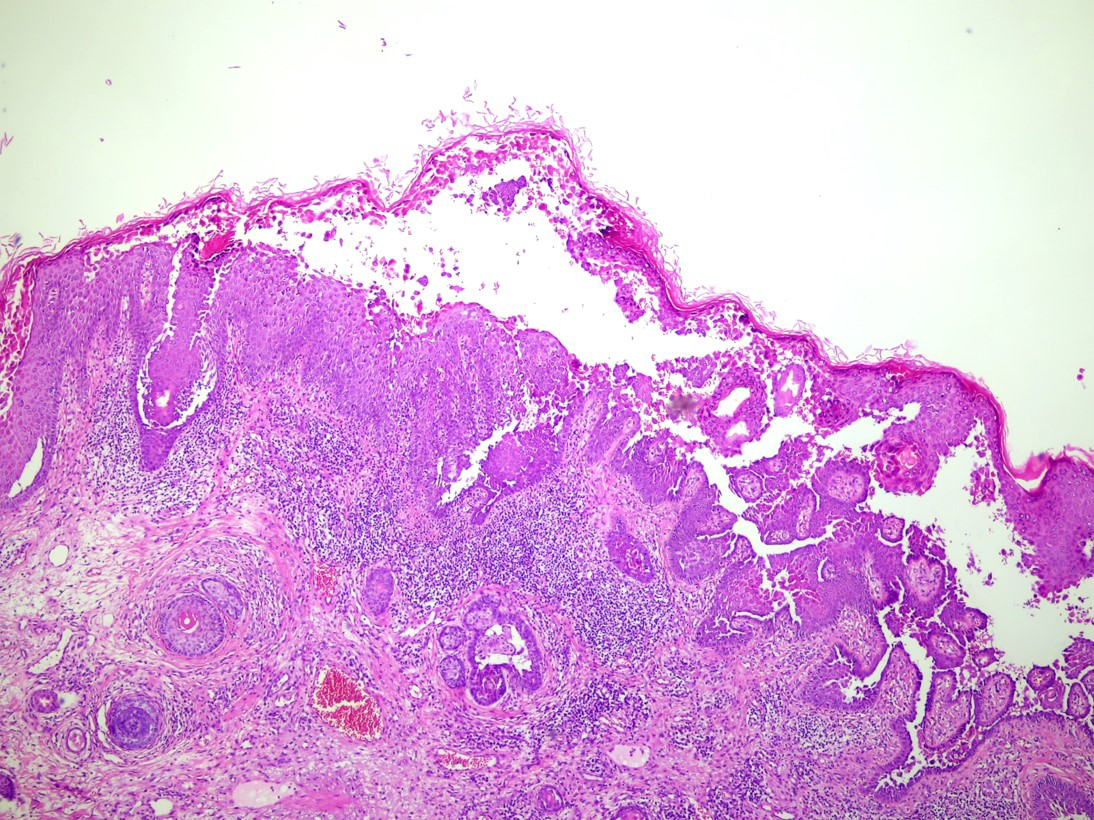
- Histopathological findings showed acanthosis and dyskeratosis with full epidermal acantholysis in the epidermis. Superficial perivascular lymphocytic infiltration in the dermis is also observed (H & E, original magnification x40)
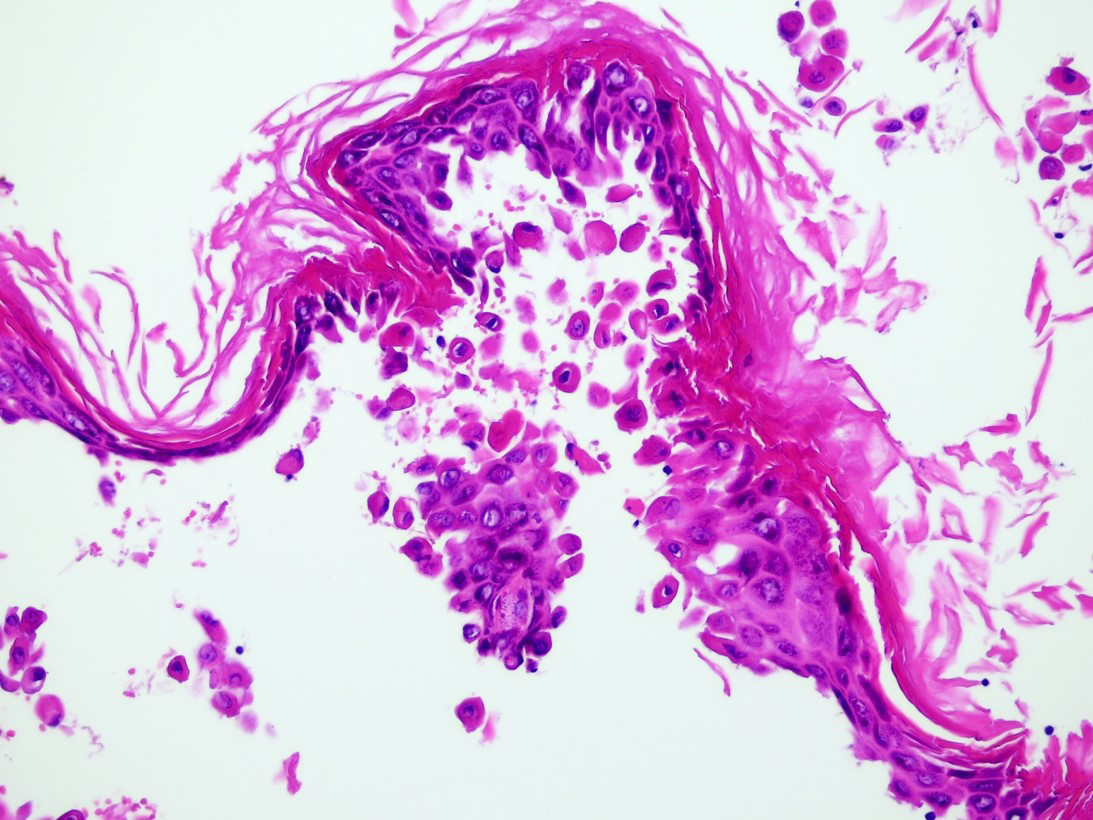
- Rounded eosinophilic dyskeratotic cells (corps ronds) and hyperkeratotic and flattened parakeratotic cells (grains) in the cornified layer are also observed (H & E, x200)
Question
What is your Diagnosis?
Answer
Diagnosis: Acantholytic dyskeratotic acanthoma
Discussion
Acanthoma is a benign tumor of epidermal keratinocytes, showing a broad range of histological patterns.1 Acantholytic dyskeratotic acanthoma is a relatively uncommon variant of acanthoma, classified within the past decade. The term ‘focal acantholytic dyskeratosis’ was first used by Ackerman to describe incidental lesions showing acantholysis and dyskeratosis.2 In contrast, genital lesions with similar characteristics had been described as ‘papular acantholytic dyskeratoma’ or ‘papular acantholytic dyskeratosis’.3,4 However, non-genital lesions showing acantholysis and dyskeratosis were not adequately identified until Omulecki et al. defined acantholytic dyskeratotic acanthoma for the first time in 2007.1 Acantholytic dyskeratotic acanthoma refers to a solitary, non-genital lesion with prominent acantholysis and dyskeratosis without cup-shaped architecture or follicular involvement.4,6,7 However, whether it is an actual distinct diagnostic entity is debatable. There is no statement from the World Health Organization, and the description of acantholytic dyskeratotic acanthoma differs even within textbooks. Lever’s histopathology and McKee’s pathology textbooks describe acantholytic dyskeratotic acanthoma as a phenomenon rather than a separate entity,8,9 while Weedon’s textbook considers acantholytic dyskeratotic acanthoma a separate entity.10
About 43 cases of acantholytic dyskeratotic acanthoma have been reported in the English literature to date [Table 1]. Patient ages ranged from 12 to 97 years, with 38 (88.4%) older than 40 years. The patients were often clinically suspected of having basal cell carcinoma, squamous cell carcinoma, and/or actinic keratosis. Most lesions were located on the trunk and often presented as a small papule of <1 cm. Among the 43 reported cases, three were in subungual areas,13–15 three occurred in a transplant setting5,12,13 and one after vemurafenib treatment.14 Among the three patients with a history of transplants, two presented with multiple lesions. However, the association between immunosuppression and acantholytic dyskeratotic acanthoma remains inconclusive.
a): Not available, b): exact duration, not given, AK: actinic keratosis, BCC: basal cell carcinoma, BD: Bowen’s disease, DLE: discoid lupus erythematosus, DM: diabetes mellitus, SCC: squamous cell carcinoma, SK: seborrheic keratosis
Year
Author
Age
Gender
Number/size (mm)
Site
Clinical diagnosis
Duration
Medical history
2007
Omulecki et al.1
64
Male
1/20 x 50
Back
(a)
7 years
DM
2008
Ko et al.4
48
Female
1/7
Ankle
BCC
(b)
(a)
40
Female
1/5
Forearm
AK/SCC
(b)
(a)
45
Female
1/4
Back
(a)
(b)
(a)
64
Female
1/4
Back
BCC
(b)
(a)
48
Female
1/5
Abdomen
BCC/SCC
(b)
(a)
49
Female
1/6
Chest
BCC/SCC
(b)
(a)
43
Female
1/3
Chest
BCC
(b)
(a)
63
Male
1/7
Back
BCC/BD
(b)
(a)
50
Female
1/4
Chest
SK
(b)
(a)
39
Female
1/7
Back
Wart
(b)
(a)
52
Female
1/6
Back
SCC
(b)
(a)
43
Male
1/5
Abdomen
BCC
(b)
(a)
45
Female
1/4
Abdomen
SK/AK
(b)
(a)
49
Female
1/5
Nevus
BCC
(b)
(a)
57
Male
1/2
Chest
BCC/AK
(b)
(a)
63
Male
1/5
Clavicle
AK/BCC/SCC
(b)
(a)
84
Male
1/9
Thigh
BD
(b)
(a)
48
Female
1/4
Flank
SK/AK
(b)
(a)
58
Male
1/7
Sternum
BCC
(b)
(a)
60
Male
1/3
Back
BCC
(b)
(a)
68
Male
1/6
Flank
SCC
(b)
(a)
57
Female
1/6
Chest
Papilloma
(b)
(a)
51
Female
1/5
Shoulder
BCC
(b)
(a)
64
Male
1/3
Chest
Nevus
(b)
(a)
75
Male
1/5
Lower leg
BCC
(b)
(a)
76
Female
1/5
Neck
SCC
(b)
(a)
47
Male
1/7
Back
Nevus
(b)
(a)
56
Female
1/5
Chest
BCC
(b)
(a)
2009
Sass et al.15
53
Male
1/5
Right thumbnail
(a)
(b)
(a)
15
Male
1/3
Right thumbnail
Onychopapilloma
6 months
(a)
12
Female
(a)
Right thumbnail
Onychopapilloma
9 months
(a)
2013
Park et al.16
42
Female
Multiple/2-3
Face
(a)
Several years(b)
Associated with rosacea
2013
Pezzolo et al.12
49
Male
1/4 x 4
Lower leg
BCC/AK
3 years
Kidney allograft patient on immunosuppression
2014
Goldenberg et al.3
72
Female
1/10 x 4
Chest
(a)
3 months
No other illness
2017
Kim et al.17
38
Female
1/(a)
Face
(a)
1 month
Associated with DLE
2018
Burgler et al.13
60
Male
Multiple/(a)
Back and lateral chest wall
(a)
1 week
Heart transplant patient on immunosuppression
2019
Kanitakis et al.5
74
Male
Multiple/(a)
Back
(a)
(b)
Liver transplant patient on immunosuppression
2020
Nandakumar et al.6
75
Female
2/13 x 15,10 x 12
Thigh
Chromoblastomycosis, SCC, tuberculosis verrucosa cutis, viral wart, lupus vulgaris
60 years
No other illness
2017
Komori et al.14
62
Female
1/(a)
Right shoulder
SCC
(b)
Metastatic melanoma on vemurafenib
2017
Ng et al.18
25
Male
1/(a)
Right thumbnail
Onychopapilloma, onychomatricoma or a verruca
1 year
No other illness
2021
Tanaka et al.19
97
Female
1/10
Right thigh
Verruca vulgaris
(b)
(a)
2022
Current case
64
Male
1/14
Neck
Inflamed SK, SCC, BCC
6–7 months
No other illness
Pathogenesis of acantholytic dyskeratotic acanthoma is still elusive. However, genetic and immunological factors along with viral infections, physical stimuli, and sunlight exposure, might play a role.3,10 Histopathologically, acantholytic dyskeratotic acanthoma is characterised by acantholysis and dyskeratosis.3,6 Therefore, it should be differentiated from other acantholytic disorders such as keratosis follicularis (Darier’s disease), transient acantholytic dermatosis (Grover’s disease), Hailey-Hailey disease, and warty dyskeratoma. As Darier’s, Grover’s and Hailey-Hailey’s diseases show distinct clinical features and immunofluorescence findings, they could be easily differentiated from acantholytic dyskeratotic acanthoma.9 On the contrary, it could be challenging to distinguish acantholytic dyskeratotic acanthoma from warty dyskeratoma as they share many histological features. However, unlike acantholytic dyskeratotic acanthoma, warty dyskeratoma is associated with a cup-shaped invagination or follicular involvement.1,3,4,6,11 Last, acantholytic dyskeratotic acanthoma can also be easily differentiated from acantholytic acnathoma by the presence of prominent dyskeratosis.
Clinically, patients with acantholytic dyskeratotic acanthoma typically present with an asymptomatic solitary keratotic papule or plaque showing predilection to the trunk,4,5 and resemble non-melanotic skin cancers such as squamous cell carcinoma, basal cell carcinoma or actinic keratosis.4,5 However, acantholytic dyskeratotic acanthoma is a benign disease that can be easily treated through excision. Therefore, it is necessary to rule out acantholytic dyskeratotic acanthoma from other conditions to avoid unnecessary procedures and treatments. It can be relatively easily differentiated from other non-melanotic skin cancers histopathologically as it lacks cellular atypia and specific morphological features of those conditions.1,3
Our case reinforces the necessity of classifying acantholytic dyskeratotic acanthoma as a distinct clinical entity. Examining and ruling out acantholytic dyskeratotic acanthoma as a clinical entity will assist in avoiding unnecessary or invasive procedures and treatments associated with another malignant disease with similar characteristics.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil
Conflict of interest
There is no conflict of interest
References
- Plaque form of warty dyskeratoma–acantholytic dyskeratotic acanthoma. J Cutan Pathol. 2007;34:494-6.
- [CrossRef] [PubMed] [Google Scholar]
- Acantholytic dyskeratotic acanthoma: Case report and review of the literature. Dermatol Pract Concept. 2014;4:25-30.
- [CrossRef] [PubMed] [Google Scholar]
- Acantholytic dyskeratotic acanthoma: A variant of a benign keratosis. J Cutan Pathol. 2008;35:298-1.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple acantholytic dyskeratotic acanthomas in a liver-transplant recipient. Dermatol Online J. 2019;25:4.
- [PubMed] [Google Scholar]
- Acantholytic dyskeratotic acanthoma: A rare clinicopathological entity–a case report and review of literature. J Skin Sex Transmit Dis. 2020;2:115-8.
- [CrossRef] [Google Scholar]
- Lever’s histopathology of the skin (11th ed). Wolters Kluwer; 2015.
- McKee’s pathology of the skin: With clinical correlations. Elsevier/Saunders; 2012.
- Weedon's skin pathology (5th ed). Elsevier; 2021.
- Dermoscopy of subungual acantholytic dyskeratotic acanthoma. Clin Exp Dermatol. 2020;45:355-6.
- [CrossRef] [PubMed] [Google Scholar]
- Acantholytic dyskeratotic acanthoma in an immunosuppressed patient: A case report with review of the literature. Clin Dermatol. 2013;1:149-52.
- [Google Scholar]
- Multiple acantholytic dyskeratotic acanthomas in an organ transplant recipient. JAAD Case Rep. 2018;4:695-7.
- [CrossRef] [PubMed] [Google Scholar]
- Acantholytic dyskeratotic acanthoma: A possible skin adverse event of vemurafenib treatment. J Eur Acad Dermatol Venereol. 2017;31:e474-5.
- [CrossRef] [PubMed] [Google Scholar]
- Acantholytic tumor of the nail: Acantholytic dyskeratotic acanthoma. J Cutan Pathol. 2009;36:1308-11.
- [CrossRef] [PubMed] [Google Scholar]
- Incidental focal acantholytic dyskeratosis. J Am Acad Dermatol. 1998;38:243-7.
- [CrossRef] [PubMed] [Google Scholar]
- Incidental Focal Acantholytic Dyskeratosis in a Patient with Discoid Lupus Erythematosus: A Possible Role for SPCA1 in the Pathogenesis of the Disease. Ann Dermatol. 2017;29:655-7.
- [CrossRef] [PubMed] [Google Scholar]
- Subungual acantholytic dyskeratotic acanthoma: An unusual cause of longitudinal erythronychia. Pathology. 2018;50:482-4.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous acantholytic dyskeratotic acanthoma accompanying syringofibroadenomatous hyperplasia with proliferation of mature sebocytes: A case report. J Cutan Pathol. 2021;48:451-4.
- [CrossRef] [PubMed] [Google Scholar]






