Translate this page into:
Botryomycosis with compressive brachial plexus neuropathy: A rare tropical disease with dermato-neurological association
Corresponding author: Dr. Vijaikumar M, Department of Skin and STD, Indira Gandhi Government General Hospital and Post Graduate Institute, Puducherry, India. vijaiderm@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mohanan S, Vijaikumar M., Carounanidy U, Banushree C. S. Botryomycosis with compressive brachial plexus neuropathy: A rare tropical disease with dermato-neurological association. Indian J Dermatol Venereol Leprol. 2023;90:99-102. doi: 10.25259/IJDVL_1005_2022
Dear Editor,
Botryomycosis is a rare chronic granulomatous bacterial skin infection characterised by nodules, abscesses and ulcers on the hands, feet, genitals and head.1 It usually results from the inoculation and subsequent persistent infection of injured skin by bacteria such as Staphylococcus aureus, Pseudomonas aeruginosa or Escherchia Coli.1 It is also known as granular bacteriosis, actinobacillosis or bacterial pseudomycosis.2 We report a patient with cutaneous botryomycosis who had compressive brachial plexus neuropathy as a result of the nodules in her axilla. We highlight this case due to its rarity and to stress upon this rarely reported complication that can result from untreated botryomycosis.
A 50-year-old female patient, who was an agricultural labourer, presented to the dermatology out-patient department with multiple painful lesions on the back exuding serous discharge since 6 months. The condition started as a single lesion on the back, which ruptured with serous discharge. Later, she developed multiple lesions extending into the bilateral axillae. The lesions were associated with pain, which exacerbated in the past one month. She also developed severe radiating pain over the left upper limb. There was no history of evening rise in temperature or weight loss. General examination revealed pallor; there was no generalised lymphadenopathy. There was mild ulnar clawing of the left upper limb and impaired touch sensation on the medial aspect of the forearm. Cutaneous examination revealed diffuse soft tissue swelling over the upper back studded with numerous sinuses, exuding serous discharge [Figure 1]. There were sinuses in the bilateral axillae too, with puckering of the skin [Figure 2]. The complete haemogram was within normal limits except for a haemoglobin of 4.8 g/dL. Peripheral smear showed microcytic hypochromic anaemia. The erythrocyte sedimentation rate was 80 mm/hour. Mantoux test was negative. Gram stain and Ziehl Nielsen stain revealed only pus cells and no organisms were seen. Pus and tissue culture sensitivity showed Staphylococcus aureus sensitive to cloxacillin and co-trimoxazole. Culture for acid-fast bacilli and fungus showed no growth. Serology for human immunodeficiency virus was negative. Skin biopsy revealed epidermal hyperplasia with dermis showing fibrocollagenous stroma densely infiltrated by neutrophils forming abscesses at places [Figure 3]. Periodic acid Schiff, Grocott’s methenamine silver and gram stains were non-contributory. Magnetic resonance imaging showed multiple linear hyperintense inflammatory sinuses and edema of the subcutaneous and muscle plane of the nape of the neck and upper back. It also showed multiple discrete enlarged upper and lower cervical lymph nodes, causing a mass effect on the brachial plexus bilaterally [Figure 4]. A neurology opinion was sought and it was opined that the patient had left brachial preganglionic plexopathy. Nerve conduction studies showed that the compound motor action potential (CMAP) of the left axillary, left suprascapular, left musculocutaneous and left radial nerve were reduced by more than 50% compared to the healthy right side. The CMAP amplitude of the left median and ulnar nerve was reduced with normal latency and conduction velocity. The CMAP of the right median and ulnar nerves and the sensory nerve action potential of bilateral median and ulnar nerves had normal amplitude, latency and conduction velocity, confirming the plexopathy. The patient was started on intravenous cloxacillin 2 gm 6 hourly for 10 days. The sinuses started healing and the pain over the left upper limb started improving [Figure 5]. After discharge, the patient was asked to continue taking the tablet co-trimoxazole (Trimethoprim 160 mg/sulphamethoxazole 800 mg) twice a day. The pain completely disappeared in 3 weeks and all the sinuses started healing. The patient was later lost to follow-up during the coronavirus disease 2019 pandemic.

- Multiple puckered sinuses on the back, few discharging serous liquid.

- Left axilla showing discharging sinuses.
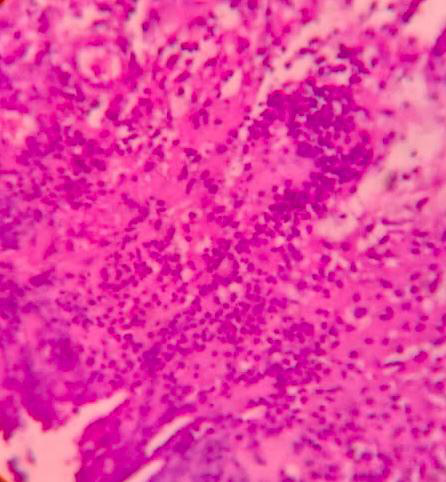
- Histopathology showing the neutrophil collection in the dermis (H&E,100x).

- Short tau inversion recovery coronal images of the neck and thorax multiple enlarged ovoid hyperintense lymph nodes, (yellow arrow) with some of them showing matting and abscess formation in the bilateral axillary region compressing the brachial plexus (yellow arrow).

- Short tau inversion recovery coronal images of the neck and thorax multiple enlarged ovoid hyperintense lymph nodes, with some of them showing matting and abscess formation in the bilateral axillary region.

- Magnetic resonance imaging: Multiple linear serpiginous hyperintense sinus tracts (yellow arrow) and abscess formation noted in the posterior upper back, involving the subcutaneous and superficial muscle plane.

- Healed sinuses forming puckered scars on the back.
The first case of botryomycosis was reported by Bollinger in 1870.3 In 1884, Rivolta proposed the term ‘botryomycosis’, from the Greek term ‘botrys’, meaning bunch of grapes, because of the characteristic groups of granules that resemble grapes and mycosis, because he thought the disease was caused by a fungus.3 The major associated predisposing factors are skin trauma, postoperative complications, diabetes mellitus, liver disorders, treatment with steroids, alcoholism and cystic fibrosis.3 Less common factors are malnutrition, glomerulonephritis, acquired immune deficiency syndrome, bronchial asthma and follicular mucinosis.3 Our patient probably had malnutrition in view of her microcytic hypochromic anemia. Botryomycosis can be cutaneous or visceral. Cutaneous botryomycosis occurs in the exposed parts of the body. Our patient developed cutaneous botryomycosis on her back. She also had swelling of soft tissues and enlarged axillary lymph nodes, causing compressive neuropathy of the brachial plexus. There are multiple reports of actinomycosis and mycetoma causing cord compression;4,5 however, we could not find a previous report of such a complication caused by botryomycosis. The differences in the differential diagnoses of soft tissue swelling with sinuses are summarised in Table 1. Usually, botryomycosis is caused by staphylococcus aureus, but Escherichia coli and Pseudomonas aeruginosa have been described as causative organisms.2 In our patient, too, materials from the pus swab grew staphylococcus aureus. Diagnosis usually depends on histopathological demonstration of bacteria. In our patient, since other cultures did not grow acid-fast bacterium or fungus, we narrowed our diagnosis to botryomycosis. In a 2018 review of 43 cases by Bailey et al.,6 they observed that most patients responded to cephalosporins or co-trimoxazole; however, 15 patients required surgical debridement. Our patient, too, responded to co-trimoxazole. There seem to be quite a few reports from India6, most probably due to increased reporting of these rare conditions. To conclude, botryomycosis continues to be reported from India and can be rarely complicated by compressive neuropathy, as in our patient. Early diagnosis and treatment can reduce the need for surgical debridement.
| Feature | Botryomycosis | Actinomycosis | Actinomycetoma | Eumycetoma | Nocardiosis |
|---|---|---|---|---|---|
| Agent | Staph aureus (commonly) | Actinomyces israelii | Actinomadura Nocardia species | Madurella mycetomatis | Nocardia species |
| Site | Extremity | Jaw, lungs, pelvis, gastrointestinal tract | Extremities | Extremities | Extremities, chest wall |
| Duration of evolution | Chronic | Chronic | Faster progress, more destruction, Early bone invasion8 | Slower progress, less destruction, late bone invasion8 | Acute to chronic |
| Histology | Grains with bacteria, cells, debris | Sulfur grainsgram-positive filaments; nonacid fast | Grains with thin filaments | Grains with thicker filaments | Gram-positive partially acid-fast filaments |
| Culture media | Ordinary culture media | Anaerobic, brain heart infusion agar | Subculture: Half-strength cornmeal agar. Brain heart infusion agar | Subculture: Half-strength cornmeal agar. Saboroaud’s agar | Ordinary media takes 2 weeks7 Saborauds glucose agar without antibiotics |
| Treatment | Surgery with antibiotics | Penicillin GAmpicillin | Streptomycin or amikacin with co-trimoxazole | Surgical excision with antifungals | Sulfonamide |
Acknowledgements
We gratefully acknowledge the contribution of Dr. S. Shrinuvasan, Associate Professor, dept of Radiology, SLIMS, Puducherry, for his contribution of MRI images of the patient
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cutaneous botryomycosis diagnosed long after an arm injury. J Am Acad Dermatol. 2014;71:e155-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous and pulmonary botryomycosis. Lancet Infect Dis. 2019;19:670.
- [CrossRef] [PubMed] [Google Scholar]
- Cervical actinomycosis causing spinal cord compression and multisegmental root failure: case report and review of the literature. Neurosurgery. 1998;43:937-40.
- [CrossRef] [PubMed] [Google Scholar]
- Cervical cord compression secondary to mycetoma infection. Sudan J Public Health. 2007;2:112-5.
- [Google Scholar]
- Cutaneous botryomycosis and staphylococcus aureus: diagnosis, management, and a systemic literature review. Curr Treat Options Infect Dis. 2018;10:347-61.
- [Google Scholar]
- Bacterial diseases. In: Bolognia JL, Schaffer JV, Cerroni L., eds. Dermatology (4th ed). China: Elsevier; 2018. p. :1259-93.
- [Google Scholar]
- Mycetoma: an update. Indian J Dermatol. 2017;62:332-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





