Translate this page into:
A case of erythema elevatum diutinum associated with peripheral ulcerative keratitis
Corresponding author: Dr. Tao Qu, Department of Dermatology, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, National Clinical Research Center for Dermatologic and Immunologic Diseases, Beijing, China. qutao2011@126.com
-
Received: ,
Accepted: ,
How to cite this article: Qiao J, Jia Q-N, Qu T. A case of erythema elevatum diutinum associated with peripheral ulcerative keratitis. Indian J Dermatol Venereol Leprol. 2024;90:364-6. doi: 10.25259/IJDVL_780_2022
Dear Editor,
A 61-year-old Chinese man presented with a 15-year history of painful skin lesions on the face, back, hands, elbows, buttocks and knees [Figure 1]. Lesions became exacerbated in cold weather. Several lesions had resolved spontaneously with subsequent intermittent recurrence at the same sites. He complained of recurrent ocular hyperemia and progressively blurred vision. Dermatologic examination showed purple-red, firm papules and plaques on the palms and dorsal aspects of hands, elbows, buttocks, knees and feet. In the right eye, slit-lamp examination showed corneal conjunctivalisation with conjunctival and episcleral hyperemia. There was a broad-based pseudopterygium that inserted onto the peripheral cornea from conjunctiva of lower right eyelid and conjunctival scar formation, leading to trichiasis and symblepharon [Figure 2]. Laboratory findings showed an elevated serum IgA level (monoclonal IgA λ-type). The histopathology of the lesions on the thigh revealed diffuse neutrophils, nuclear dust, leukocytoclastic vasculitis of the superficial and mid-dermal vessels [Figure 3]. Therefore, a diagnosis of erythema elevatum diutinum (EED) with peripheral ulcerative keratitis (PUK) was established based on the clinical and histopathological features.

- Purple-red, firm papules and plaques on the dorsal aspects of hands

- Purple-red, firm papules and plaques on the dorsal aspects of elbow
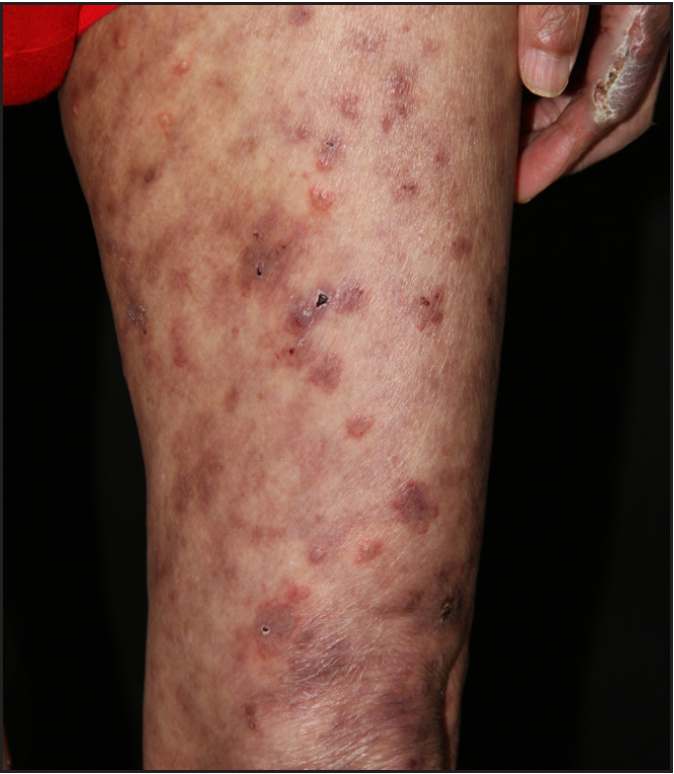
- Purple-red, firm papules and plaques on the dorsal aspects of thigh
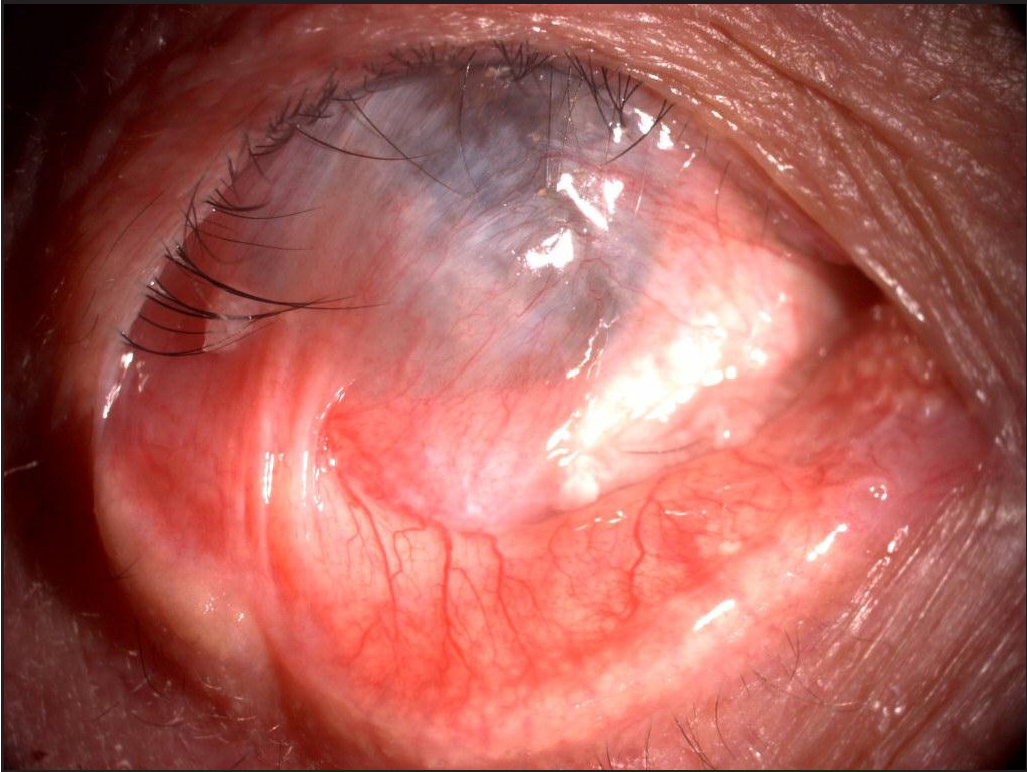
- Slit-lamp examination of the right eye
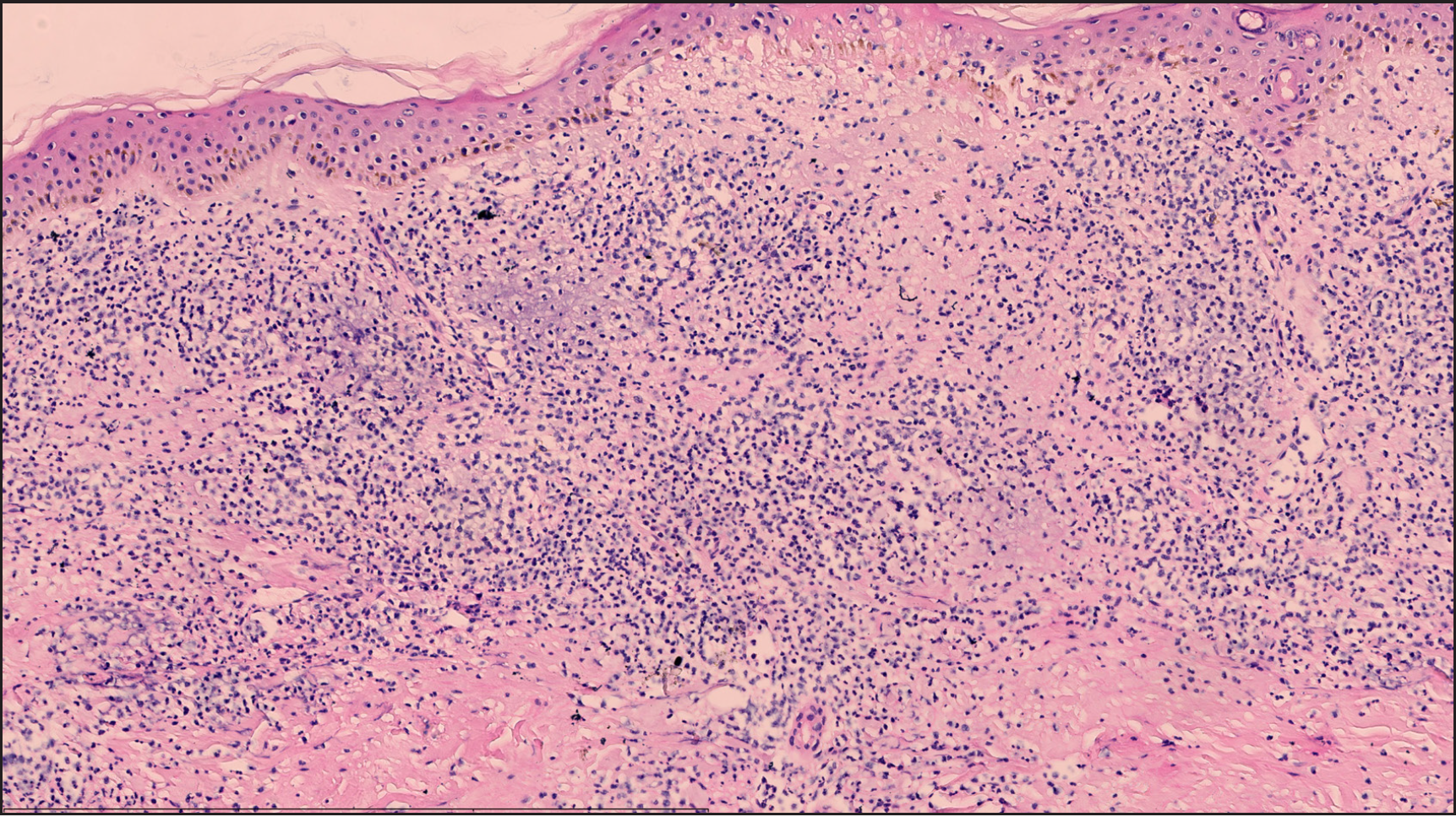
- Diffused neutrophils, nuclear dust and leukocytoclastic vasculitis of the superficial and dermal vessels (H&E staining; scale bar: 600 um; magnification x100)
Erythema elevatum diutinum is a rare form of neutrophilic dermatoses which is characterised by the presence of mature neutrophilic infiltration in the skin and other organs, with possibly associated systemic diseases. Erythema elevatum diutinum initially presents as leukocytoclastic vasculitis of the skin and later resolves with fibrosis. It is characterized by violaceous papules, nodules and plaques symmetrically distributed over extensor surfaces of the extremities.1,2 Erythema elevatum diutinum has been reported to be connected with a variety of diseases, including haematological conditions, autoimmune disorders, certain malignancies and bacterial and viral infections. Cases of erythema elevatum diutinum associated with ocular damage are rare with only a few described in the literature. Here, we describe a rare case of erythema elevatum diutinum associated with peripheral ulcerative keratitis and IgA paraproteinemia. Triamcinolone 12 mg daily and glucosidorum tripterygll totorum 60 mg daily were administrated resulting in good improvement 2 months later. The patient had been given a diagnosis of pulmonary interstitial fibrosis based on lung computed tomography findings in the 2-year follow-up.
Erythema elevatum diutinum shows a heterogeneous clinical and histopathological manifestation largely depending on the clinical stage and thus has various differential diagnoses. Clinically, early stage of erythema elevatum diutinum should be differentiated from other neutrophilic dermatoses, including neutrophilic dermatosis of the dorsal hands and Sweet’s syndrome. Later stage of erythema elevatum diutinum may resemble granuloma annulare, tuberous xanthomas, kaposi’s sarcoma, rheumatoid nodules, dermatofibroma and multicentric reticulohistiocytosis. However, histopathological presentation of erythema elevatum diutinum may aid in the differential diagnoses. Early features of erythema elevatum diutinum are leukocytoclastic vasculitis, polymorphonuclear cell infiltrate and fibrin deposition in the dermis. Later stage of erythema elevatum diutinum is characterised by further fibrosis with intravascular and perivascular fibrin deposits and more granulation tissue, which are assumed to be the result of chronic dermal injury of leukocytoclastic vasculitis.
This case of recurrent and persistent lesions associated with ocular damage should also be distinguished from Behcet disease and sweet’s syndrome. Behcet disease is an autoinflammatory systemic vasculitis characterised by recurrent oral and genital ulcers, ocular involvement, cutaneous erythema and nodosum-like and papulopustular lesions. The diagnostic criteria of Behcet disease is the concurrence of oral aphthae and two of the following features: genital ulceration, ocular manifestations, skin lesions and positive pathergy test. Sweet’s syndrome is characterised by the abrupt onset of painful erythematous skin lesions and a dense dermal neutrophilic infiltrate histopathologically and may also be associated with fever, leukocytosis and neutrophilia which are distinguishable from the present case.
Extracutaneous manifestations have been reported sporadically, including IgA paraproteinemia, ocular damage and oral and penile ulcers. Ocular damage in erythema elevatum diutinum include scleritis and panuveitis, but cases of erythema elevatum diutinum associated with peripheral ulcerative keratitis are extremely rare. We found only six cases of erythema elevatum diutinum associated with peripheral ulcerative keratitis reported in the literature. Peripheral ulcerative keratitis is considered as a sight-threatening condition which involves the outer portions of the cornea. Peripheral ulcerative keratitis may appear prior to or after the eruption of erythema elevatum diutinum. In our case, clinical presentation of peripheral ulcerative keratitis occurred 5 years later than erythema elevatum diutinum.
Although the exact pathogenesis remains unknown, a general principle is suggested by the pathophysiology features of erythema elevatum diutinum, including multi-organ involvement with skin and mucosa, neutrophil-driven inflammation and elevated serum IgA level. Intravascular immune complex deposition has been considered as a pathogenic factor for erythema elevatum diutinum which is also assumed to be associated with the pathogenesis of peripheral ulcerative keratitis. A retrospective review of associations of erythema elevatum diutinum demonstrated IgA paraproteinemia to be the most common in 57.45% among all the reported paraproteinemias, followed by IgG, IgM and IgD.3 IgA antineutrophil cytoplasmic antibody is suggested to be associated with immune dysregulation which initiates the neutrophil activation and ultimately leads to clinical manifestation.4
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Erythema elevatum diutinum: A review of presentation and treatment. J Eur Acad Dermatol Venereol. 2014;281:594-602.
- [Google Scholar]
- Erythema elevatum diutinum. Indian J Dermatol Venereol Leprol. 2013;79:238-9.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema elevatum diutinum: A case report and review of literature. Int J Dermatol. 2019;58:408-15.
- [CrossRef] [PubMed] [Google Scholar]
- Is IgA antineutrophil cytoplasmic antibody a marker for patients with erythema elevatum diutinum? A further three cases demonstrating this association. Br J Dermatol. 2011;164:675-7.
- [CrossRef] [PubMed] [Google Scholar]





