Translate this page into:
Dermoscopic and in vivo reflectance confocal microscopic features of endogenous ochronosis
Corresponding author: Dr. Fatmagul Dirican Ulusoy, Department of Dermatology, Mardin Educational and Research Hospital Dermatology Clinic, Mardin, Turkey. gdirican@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ulusoy FD, Yaman B, Ceylan C, Karaarslan I. Dermoscopic and in vivo reflectance confocal microscopic features of endogenous ochronosis. Indian J Dermatol Venereol Leprol. 2024;90:646-9. doi: 10.25259/IJDVL_935_2022
Dear Editor,
Endogenous ochronosis (EO) is a rare hereditary metabolic disease caused by the decreased activity of the enzyme, homogentisate 1,2 dioxygenase. Bluish-grey discoloration of the skin and mucosa is typically seen in this disorder. 1 The features of ochronosis by in vivo reflectance confocal microscopy (RCM) have scarcely been reported and that too, in only the exogenous type. The present case demonstrates the clinical features, dermoscopic findings, RCM findings and the response to the treatment in a case of EO. We were unable to find any previous reports of RCM features of EO.
A 49-year-old male presented with pigmented skin lesions on his ears and pain and limitation of movement in both knees since five years. There was no history of intake of systemic drugs or topical medications. There were bluish-grey nodules seen on both the auricles [Figures 1a and 1b] and yellowish-brown discoloration of the conjunctivae [Figures 1c and 1d]. The left knee was swollen and had a limited range of motion [Figure 1e]. The magnetic resonance imaging and X-ray of the knee revealed osteophytic degenerative changes [Figure 1f]. Liver and kidney function tests, complete blood count, and rheumatoid factor were within normal limits. ANA was positive at a titer of 1/160. The patient’s urine darkened after two hours of exposure to the air. The level of homogentisic acid detected in urine or blood could not be evaluated for technical reasons. The homozygous mutation was detected in the HGD gene (exon 10, c.731_749del p.Thr244ArgfsTer30). Renal or cardiovascular involvement was not detected.

- Bluish-grey nodular lesions on the left auricle.

- Bluish-grey nodular lesions on the right auricle.

- Yellow-brown discoloration in left conjunctiva.

- Yellow-brown discoloration in right conjunctiva.
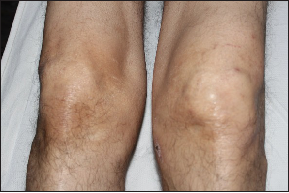
- Swelling of the left knee joint.

- Osteophytic degenerative changes on direct radiography.
Dermoscopic examination of the ear lesions revealed a homogeneous brown to grey-blue pigmentation and linear vessels on a pinkish background [Figure 2a and 2b]. On reflectance confocal microscopy (Vivascope 3000; CALIBER ID, Rochester, NY, USA), the epidermis exhibited a normal honeycombed pattern with inflammatory and dendritic cells. The dermo-epidermal junction had a normal ridged pattern with normal-edged papillae. The dermis had hypo-refractile irregular, disorganised dark areas of different shapes and sizes [Figures 3a and 3b]. There were thin irregular collagen fibres with increased inflammatory cells and vessels between these dark areas. There were no atypical cells.

- Homogeneous brown to grey-blue pigmentation (red arrow) (Dermlite DL4, polarised light)
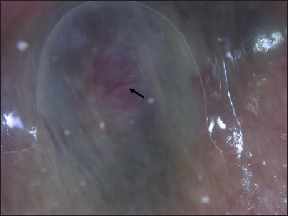
- Linear vessels on the pinkish background (black arrow) (Dermlite DL4, polarised light).
Histopathological examination revealed both small and large, numerous, yellowish brown, oval to round amorphous acellular substances (ochre pigment) in the reticular dermis along with increased vascularization and inflammatory cell infiltrates. Small amorphous deposits were seen very close to the flattened epidermis in some areas [Figures 3c and 3d]. A-low protein diet and nitisinone treatment (30 mg/day) were given. No progression was seen during the ensuing six-month period.
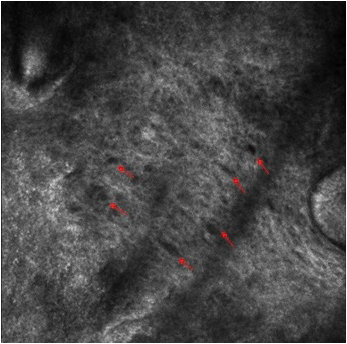
- Oval dark spaces between irregular collagen fibers at lower magnification (red arrow).
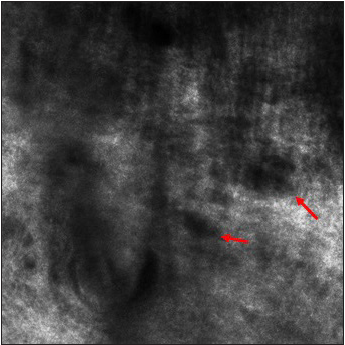
- Oval dark spaces between irregular collagen fibers at higher magnification (red arrow).
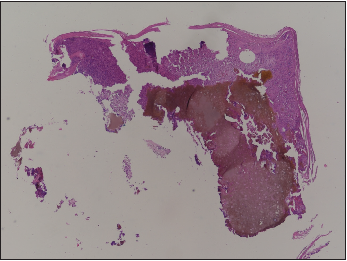
- Yellowish brown amorphous material in the dermis; increased vascularity and inflammatory cell infiltrates (H&E, 40x).
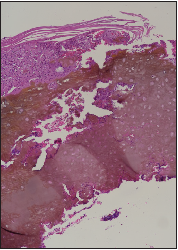
- Yellowish brown amorphous material in the dermis; increased vascularity and inflammatory cell infiltrates (H&E, 100x).
Dermoscopic findings of EO have been reported in only two cases, which included pseudo-network and partial occlusion of the follicular openings on the face and bluish-grey and white globular areas on the acral region. 1,2 In the present case, homogeneous brown to blue-grey pigmentation and linear vessels on a pinkish background were the dermoscopic features on the ears.
Evaluating only the superficial layers of the skin including the superficial dermis may be a major limitation of RCM in cases of EO with deep deposits. However, it may be possible to demonstrate deposits close to the surface. This possibility has been shown clearly in the present case; ochre pigment was observed as hypo-refractile, irregular, disorganized dark areas with different shapes and sizes at the dermal level on RCM. In the literature, available data on RCM findings of ochronosis are based on observations in some cases of exogenous ochronosis. In exogenous ochronosis, brown-grey reticulated macules with grey-black coarse spots are seen on the skin, most commonly on the malar regions of the patients treated for melasma with topical hydroquinone. 3 In these cases, the accumulation is expected to be small and superficial. 4–7 Dark, well-defined, round-to-oval and banana-shaped spaces in the papillary and middle dermis were the reported features on RCM. 4–6
Dermoscopy and RCM are particularly important in considering the clinical differential diagnoses of bluish-grey nodular lesions. In this case, the multiple symmetrical lesions on the ears suggest a possible diagnosis of EO. The differential diagnosis of a single bluish-grey nodule may include, besides EO, nodular melanoma, melanoma metastasis, blue nevus, pigmented basal cell carcinoma, and skin appendageal tumors. With the typical dermoscopic findings, it may be possible to differentiate between these entities. However, in a solitary lesion of EO, the diagnosis of ochronosis could be more convincing by demonstrating the deposits in the dermis and excluding the differentials demonstrating atypical cells.
In conclusion, RCM may be helpful in the diagnosis of EO with very superficial deposits, as seen in the present case. However, it must be noted that RCM findings should be taken in tandem with the suggestive clinical features and the diagnosis still needs to be confirmed by histopathology.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Endogenous ochronosis: A dermoscopic view. Int J Dermatol. 2019;58:e175-e178.
- [CrossRef] [PubMed] [Google Scholar]
- Endogenous ochronosis: When clinical suspicion prevails over histopathology. Dermatol Online J. 2019;25:13030/qt5q2763pj.
- [PubMed] [Google Scholar]
- Exogenous ochronosis. Indian J Dermatol. 2015;60:537-43.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermoscopic and reflectance confocal microscopic features of exogenous ochronosis. Arch Dermatol. 2010;146:1021-5.
- [CrossRef] [PubMed] [Google Scholar]
- Apport de la dermoscopie et de la microscopie confocale par réflectance dans le diagnostic d’ochronose exogène [Role of dermoscopy and reflectance confocal microscopy as an aid in the diagnosis of exogenous ochronosis] Ann Dermatol Venereol. 2016;143:318-20.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic and laser confocal features of an exogenous ochronosis case. G Ital Dermatol Venereol. 2020;155:367-8.
- [CrossRef] [PubMed] [Google Scholar]
- Exogenous ochronosis in melasma: A study from South India. Pigment International. 2014;1:17-22.
- [Google Scholar]





