Translate this page into:
Non-cultured epidermal cell suspension and laser resurfacing to improve the appearance of thick post-burn skin graft
Corresponding author: Dr. Somesh Gupta, Department of Dermatology and Venereology, All India Institute of Medical Sciences, Delhi, India. someshgupta@aiims.edu
-
Received: ,
Accepted: ,
How to cite this article: Mehta N, Taneja N, Gupta S. Non-cultured epidermal cell suspension and laser resurfacing to improve the appearance of thick post-burn skin graft. Indian J Dermatol Venereol Leprol. 2024;90:376-8. doi: 10.25259/IJDVL_402_2023
Dear Editor,
Non-cultured epidermal cell suspension (NCES) has a variety of indications in pigmentary disorders apart from vitiligo, including post-burn depigmentation, post-herpetic depigmentation, chemical leukoderma and depigmentation in discoid lupus erythematosus patients.1 In addition to depigmentation, non-cultured epidermal cell suspension has also been found to be useful to treat colour mismatch, variegation and textural changes that occur after surgery in vitiligo patients.2 Non-cultured epidermal cell suspension is potentially useful to replace any uneven texture formed as a sequela of a disease or its intervention with a more uniform homogenous epidermis. Here, we present a novel use of non-cultured epidermal cell suspension to improve the appearance of post-burn skin graft over the face.
An 18-year-old female presented to us seeking improvement in the appearance of a skin graft. She had severe burns on the left side of the face 10 years ago, for which a large, full-thickness skin graft using the thigh as the donor site was done 6 years ago by a plastic surgeon. At presentation, the thick graft was distinctly noticeable, being hyperpigmented and raised compared to the rest of the face [Figure 1a]. It also had prominent follicles and covered almost the whole of the left side of the face. The graft had a ‘stuck-on’ appearance on the face. The patient was highly dissatisfied with the appearance. She had not shown any significant improvement with the use of modified Kligman’s regimen for 3 months prior to taking up for surgery.
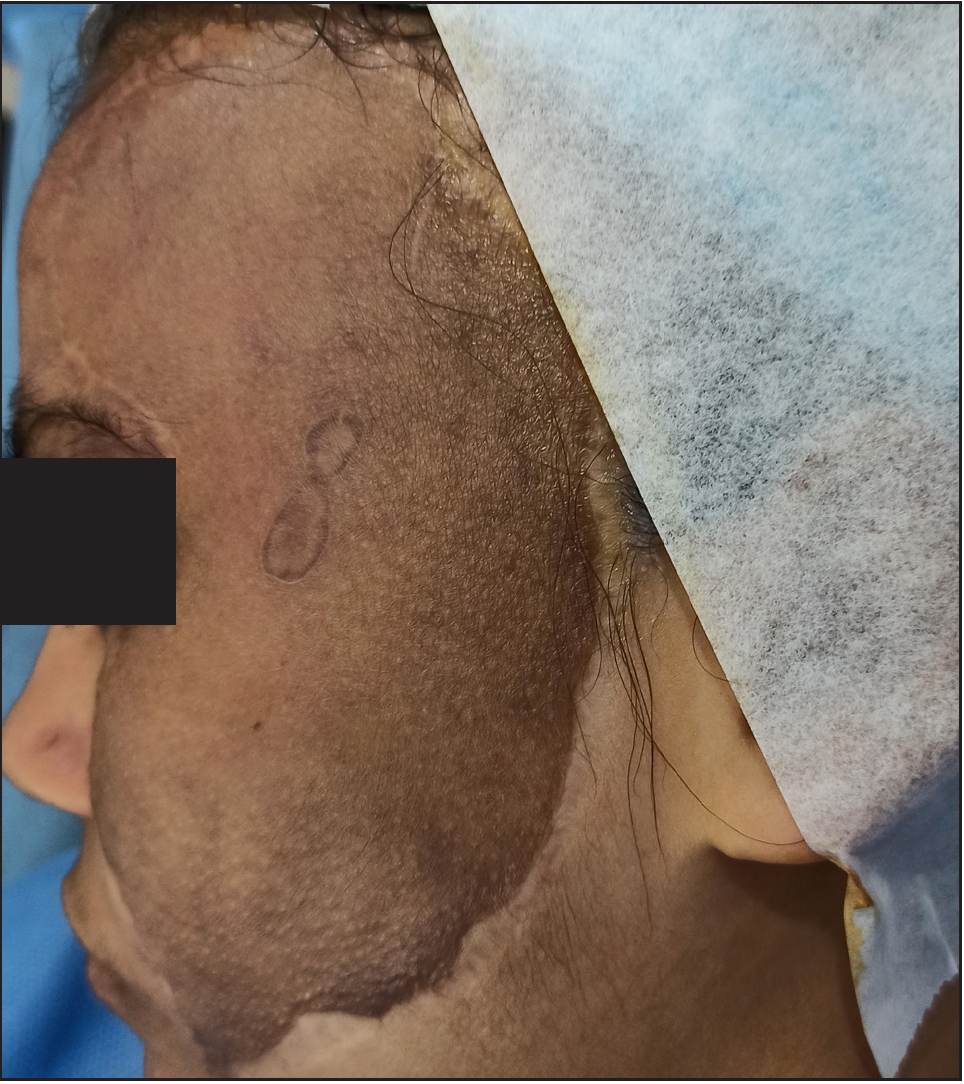
- A patient with a distinctly noticeable hyperpigmented thick post-burn graft on the face. The graft was elevated compared to the rest of the facial skin, appeared stuck-on and had prominent follicles. A small linear scarred area was present within the graft over the zygomatic ridge.

- Non-cultured epidermal cell suspension (NCES) for thick post-burn graft. The graft epidermis has been dermabraded.

- One month after the non-cultured epidermal cell suspension session. There was significant improvement in the colour match and skin texture. The elevation was reduced and the follicular openings became less prominent. The linear scarred area over the zygomatic ridge healed slowly compared to the surrounding skin.
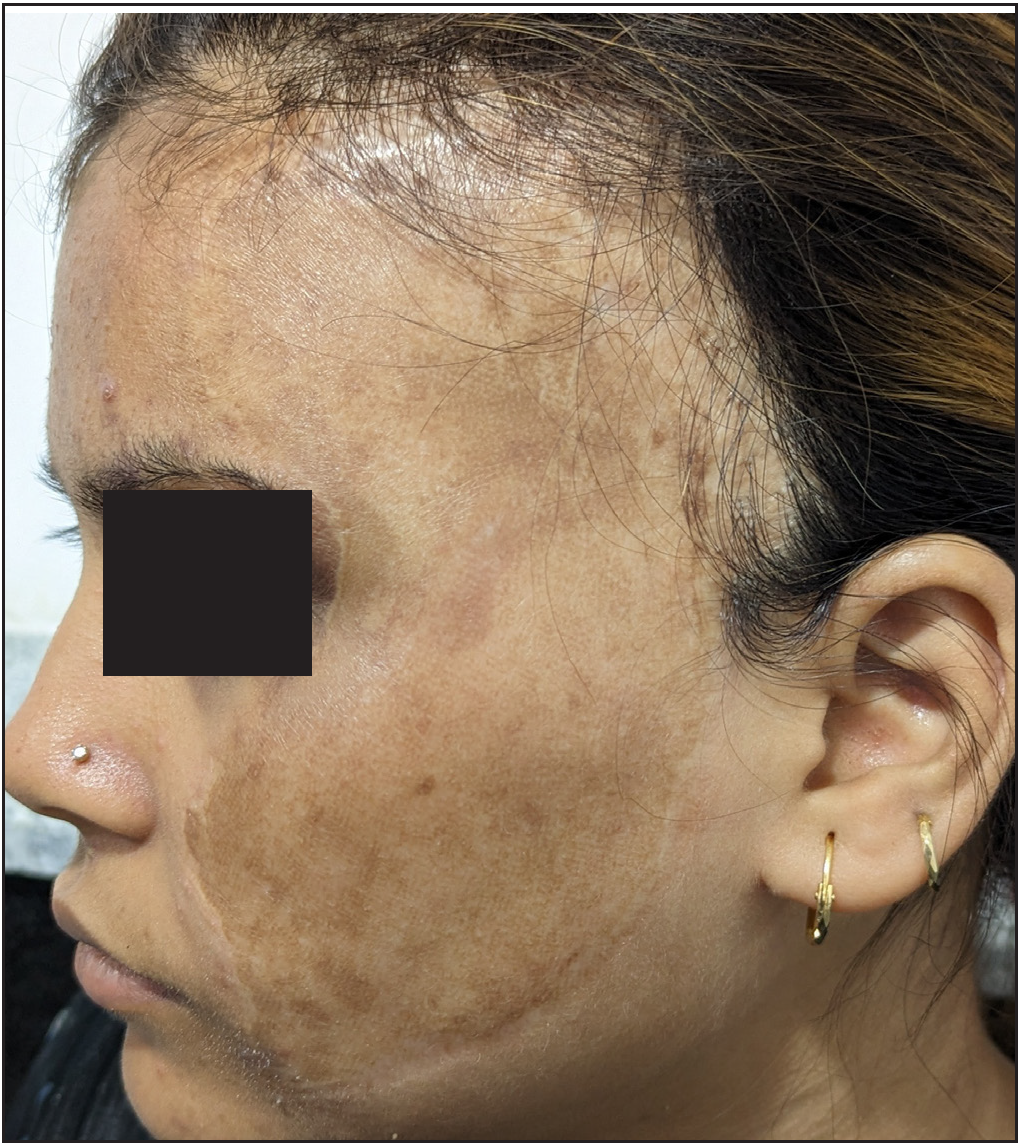
- Ten months after a single session of non-cultured epidermal cell suspension and four sessions of CO2 laser. Further homogenisation of colour, flattening, merging of margins and improvement in texture, but there was hyperpigmentation on the skin of the graft. The patient was moderately satisfied with the resultant appearance.
For non-cultured epidermal cell suspension, the cellular suspension was prepared using the standard technique.2 The skin of the post-burn graft was superficially dermabraded till the level of papillary dermis (indicated by the development of pin-point bleeding) [Figure 1b]. The cell suspension was applied over the dermabraded area and then covered with dry collagen sheet, a transparent film dressing and an adhesive plaster. The dressing was removed after 1 week and the eroded area was allowed to heal spontaneously without any medications. One month after non-cultured epidermal cell suspension, the color of the grafted site matched well with the rest of the face and there was also moderate flattening of the tissue, getting rid of the stuck-on appearance [Figure 1c]. Subsequently, four sessions of fractional CO2 laser ablation of the raised graft were done, at monthly intervals starting 2 months after the non-cultured epidermal cell suspension. This resulted in homogenisation of colour, further flattening of the graft, merging of the graft margins with the periphery, significant reduction of the follicular prominences and significant improvement in texture. However with time increased pigmentation was noticed in the grafted skin compared to the surrounding skin despite photo protection and sunscreen use [Figure 1d]. Overall, the graft was significantly less noticeable and the patient was moderately satisfied. The resultant graft had a much better aesthetic appearance, rated as 5 out of 10 on an investigator global assessment scale by us. The patient rated the overall improvement in appearance as 7 out of 10 on a visual analogue scale.
There were no immediate post-procedural complications and the patient tolerated the procedure well. A small previously scarred area over the zygomatic arch healed slowly with superficial erosions persisting till a month after procedure. Subsequently, it healed with mild dyspigmentation.
Epidermal cell suspension has been used for the management of burns and non-healing ulcers and wounds as it leads to faster re-epithelialization.3,4 Dermabrasion or ablative CO2 laser alone without transplanting the non-cultured epidermal cell suspension would have resulted in a longer time to reepithelization for such a large surface area. Non-cultured epidermal cell suspension promoted faster healing and lesser inflammation. Non-cultured epidermal cell suspension combined with dermabrasion is also reported to improve dyspigmentation caused by vitiligo treatments and colour of scars.2,5 Therefore, we hypothesise that non-cultured epidermal cell suspension helped in achieving relatively homogenous lightening of the graft in this patient.
In conclusion, non-cultured epidermal cell suspension can be useful in alleviating the colour, texture and skin thickness mismatch between the thick skin grafts and the surrounding skin with good patient satisfaction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Treatment of post-burn leucoderma with non-cultured melanocyte-keratinocyte transplantation (MKTP) Burns. 2011;37:448-52.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous noncultured epidermal cell suspension for treatment of iatrogenic variegate repigmentation, textural changes and color mismatch in vitiligo. Dermatol Ther. 2020;33:e14399.
- [CrossRef] [PubMed] [Google Scholar]
- The use of a non cultured autologous cell suspension to repair chronic ulcers. Int Wound J. 2013;12:32-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Autologous epidermal cell suspension: A promising treatment for chronic wounds. J Tissue Viability. 2016;25:50-6.
- [CrossRef] [PubMed] [Google Scholar]
- The use of noncultured regenerative epithelial suspension for improving skin color and scars: A report of 8 cases and review of the literature. J Cosmet Dermatol. 2019;18:1487-94.
- [CrossRef] [PubMed] [Google Scholar]





