Translate this page into:
Calciphylaxis causing skin gangrene in an old woman with end-stage renal disease
Corresponding author: Dr. Shuaihantian Luo, Department of Dermatology, The second Xiangya Hospital of Central South University, No. 139 Renmin Road, Changsha, Hunan, China. lsht5309@163.com
-
Received: ,
Accepted: ,
How to cite this article: Luo S, Feng Y, Zhou Y. Calciphylaxis causing skin gangrene in an old woman with End-stage renal disease. Indian J Dermatol Venereol Leprol, 2023;89:792
Dear Editor,
Calciphylaxis is a rare but devastating disease that is predominantly observed in patients suffering from chronic kidney failure who are treated with dialysis. Mortality rates in chronic hemodialysis patients with calciphylaxis were almost three times higher than those without calciphylaxis. In this report, we describe an old woman who presented with skin gangrene caused by calciphylaxis.
A 68-year-old woman presented with a 3-month history of ulceration in her lower extremities. The lesion started as a painful erythematous patch in her right lower leg and rapidly developed into crusted ulcers. Subsequently, the same type of lesion appeared in her left lower leg. She was diagnosed with end-stage renal disease secondary to chronic glomerulonephritis and had been on regular hemodialysis for 3 years. Physical examination showed a big ulcer, 5×5 cm in size, mostly covered by black eschar near the right ankle [Figure 1a]. Two smaller violaceous plaques with central eschar-covered ulcers were seen in the left lower limb [Figure 1b]. Peripheral pulse was normal.

- Skin ulcers and tissue necrosis on the right leg. Well-demarcated necrotic ulcer covered with black eschar

- Skin ulcers and tissue necrosis on the right leg. Well-demarcated necrotic ulcer covered with black eschar
Routine parameters showed white blood cells: 7.23 × 109/L, haemoglobin: 93 g/L, and red blood cells: 1.56 × 1012/L. Renal function tests showed serum creatinine: 687 µmol/L, parathyroid hormone (PTH): 23 pmol/L, and glomerular filtration rate (GFR): 11 mL/min. Serum electrolyte showed potassium levels to be 3.17 mmol/L and calcium levels to be 2.61 mmol/L. Human serum albumin was calculated to be 33.7 g/L, erythrocyte sedimentation rate was found to be 92 mm/h, and C-reactive protein to be 33.7 mg/l. Arteriovenous ultrasound of both lower extremities showed lower extremity dorsal pedis artery stenosis, arteriosclerosis and extensive plaque formation, suggesting the recanalization after stenosis and the insufficiency of the popliteal vein valve. The skin biopsy showed calcification, intimal fibrosis of the blood vessel wall in the subcutis [Figure 2a]. Haemorrhage and numerous neutrophils were observed around the small vessels in the dermis [Figure 2b]. Alizarin red staining was positive around the vessels [Figure 2c].
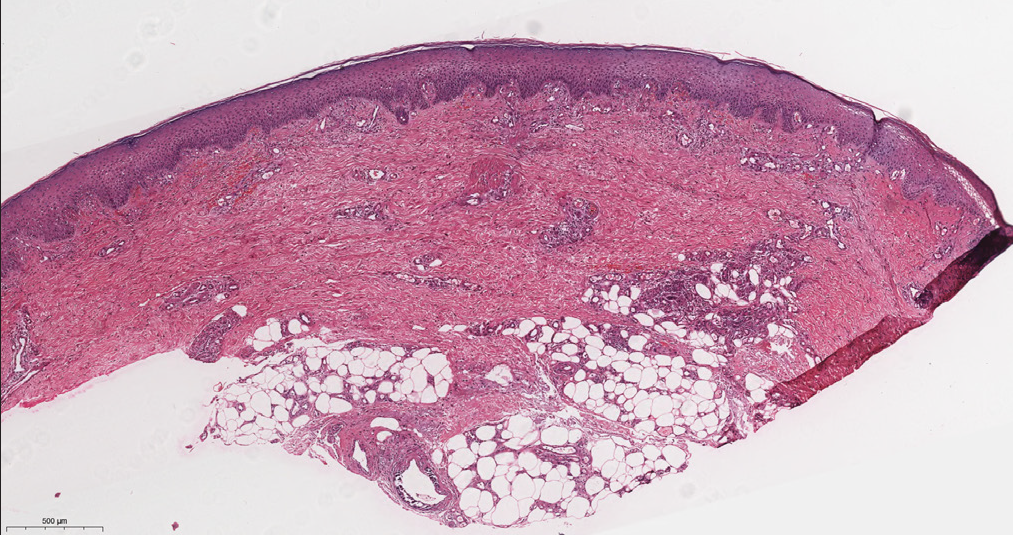
- Heamorrhage and numerous neutrophils around the small vessels in the dermis (H&E, ×100)

- Calcification and fibrosis of a vessel wall (H&E, ×400)
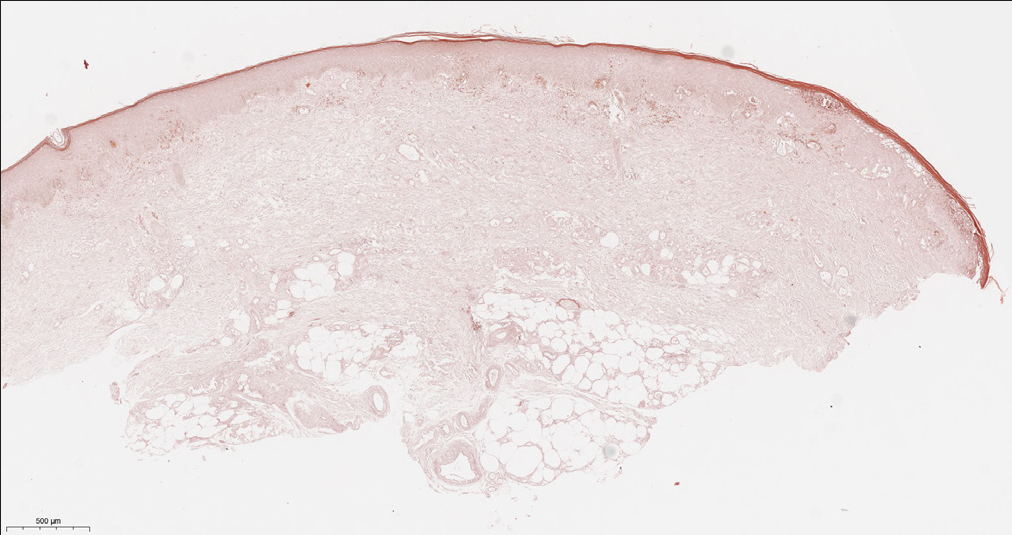
- Alizarin red staining positivity around the vessels (H &E, ×100)
Based on clinical data and histological features, the diagnosis of calciphylaxis was confirmed. During her hospital stay, the frequency and duration of heamodialysis was increased. She was treated with zinc oxide pastes to repair local wounds, sodium thiosulfate to resist calcification, lanthanum carbonate to reduce phosphate absorption, and cinacalcet to ameliorate PTH. Unfortunately, she succumbed to sepsis from a recurrent wound infection and passed away one year after diagnosis.
Calciphylaxis is a rare and fatal vascular disease that often occurs in patients with end-stage renal disease treated with heamodialysis. 1,2 Calciphylaxis mostly affects the female gender and its aetiology remains unclear. Other risk factors include diabetes, obesity, vitamin K deficiency, hypoalbuminemia, thrombophilia, medications (warfarin, vitamin D, and phosphate binders), altered mineral metabolism and hyperparathyroidism. 1,3 Calciphylaxis may be a manifestation of Koebner phenomenon, suggesting trauma is a risk factor. 4
Cutaneous calciphylaxis is caused as a result of ischemic injuries of the cutaneous blood vessels. The process involves calcification within the media layer, fibrosis underneath the intima of vessel walls, and thrombotic occlusion in the vessel lumen. 1,3,5 The typical clinical manifestations of calciphylaxis include skin lesions with severe pain, mainly livedo reticularis, violaceous plaques, or sclerotic nodules in the early stage, rapidly progressing skin ulceration and necrosis, secondary infection and poor prognosis. 6 Histologically, calciphylaxis is characterized by calcium deposition in small and medium vessels and vascular thrombosis leading to tissue ischemia, which in turn leads to skin tissue ulceration and necrosis. 1,5 Other histopathological features include extravascular tissue calcification, especially perieccrine calcification, calcium in elastic fibers, panniculitis, and epidermal necrosis. 1,3
Calciphylaxis with a painful ulceration may be mistaken for pyoderma gangrenosum. Pyoderma gangrenosum often occurs with comorbidities such as inflammatory bowel disease, connective tissue diseases, and heamatoproliferative disorders. 7 The lesion of pyoderma gangrenosum manifests initially as a papulopustule and rapidly develops into a painful deep ulcer with a raised and rolled bluish margin. Histopathological features of pyoderma gangrenosum show neutrophilic infiltration in the dermis and subcutaneous tissue. 7 Other diseases with eschar-covered ulcers, such as warfarin and heparin-induced necrosis, antiphospholipid antibody syndrome, diabetic ulcer may also imitate calciphylaxis 1,3,5 [Table 1].
| Diseases | Clinical features | Histopathological features |
|---|---|---|
| Calciphylaxis | Skin lesions with severe pain, violaceous plaques, rapidly progressing to skin ulceration and necrosis. | Calcium deposition in small and medium vessels and vascular thrombosis leading to tissue ischemia. |
| Pyoderma gangrenosum | Often occurs with comorbidity. Initially manifests as a papulopustule and rapidly develops into a painful deep ulcer with a raised and rolled bluish margin. | Neutrophilic infiltration in the dermis and subcutaneous tissue |
| Warfarin and heparin-induced necrosis | Pain and purpura, which over a few days becomes bluish-black with a red rim, followed by heamorrhagie blisters and full-thickness skin necrosis. Red netlike rash around the necrotic area. | Clotting within blood vessels in the skin without any inflammation. |
| Antiphospholipid antibody syndrome | Widespread necrosis of skin and severe in some cases. With disfiguring necrosis, these patients suffer pain and are at risk of superimposed infection. Livedo reticularis is due to thrombotic involvement of arterioles and arteries. | Thrombotic vasculopathy, vascular occlusion of arterioles and arteries with a fibrinoid plug, minimal or no inflammation of the blood vessel wall or surrounding tissue. Marked dermal necrosis. |
| Diabetic ulcer | Hypoesthesia, hyperesthesia, paresthesia, dysesthesia, and radicular pain. Vascular insufficiency has varied presentations and most patients are asymptomatic. Intermittent claudication, rest pain, and healing or non-healing ulcers. | Thickening of the walls of small blood vessels in the dermis and subcutis and some proliferation of their endothelial cells. The thickening of the walls and subsequent luminal narrowing is caused by the deposition of PAS-positive material in the basement membrane region. |
The treatment of calciphylaxis primarily requires a high-quality wound care, surgical debridement, pain relief, and other general treatments 5 [Table 2]. Therapeutic options aimed at vascular calcification and thrombosis should also be emphasised. Targeted therapy such as sodium thiosulfate and vitamin K can be administered [Table 2]. For refractory skin lesions and advanced lesions, new treatments such as human amniotic stem cell transplantation, hyperbaric oxygen therapy, and bisphosphonates can be considered. 1,2,6
| Case No. | Authors, year | Age/sex | Clinical features | Treatment | Outcome |
|---|---|---|---|---|---|
| 1 | Karmegam, et al. 2017 | 60 y/male | Indurated nodules that progressed to painful necrotic skin lesions in both his lower extremities and buttocks. | Intravenous sodium thiosulfate, elaborate wound care, increasing dialysis dose, and discontinuing vitamin D supplements and calcium containing phosphate binders. | Succumbed to sepsis from a recurrent wound infection and passed away. |
| 2 | Tangkham, et al. 2019 | 43 y/male | Thigh pain that progressed to necrotic skin lesions on the right thigh, then developed into large skin necrosis with a violaceous patch on the left thigh. | Intravenous ciprofloxacin, sodium thiosulfate, oral opioids, gabapentin, and intravenous fentanyl. | Refused for surgical debridement and died from sepsis 3 months after presenting with cutaneous lesions. |
| 3 | Zhou, et al. 2014 | 59 y/male | Painful, non-healing ulcerations on legs. The lesions developed without known trauma. | Cinacalcet, daily heamodialysis, sodium thiosulfate, and bisphosphonate. | Skin condition improved |
| 4 | Sherban, et al. 2021 | 66 y/male | A tender, ulcerated plaque on the glans penis without inguinal lymphadenopathy. | Sodium thiosulfate, wound care, and urinary diversion with a suprapubic catheter to prevent infection. | unknown |
| 5 | Hall, et al. 2015 | 53 y/female | Large symmetric breast ptosis with everted nipples without discharge. Blanching erythema and induration were noted over both breasts with underlying palpable masses. | Daily heamodialysis, intravenous sodium thiosulfate, high flow oxygen therapy, and non-calcium-containing phosphate binders. | Successful closure by secondary intention occurred within 4 weeks. |
In conclusion, we report this case to increase awareness of this rare disease, and to emphasize the importance of systemic testing in the diagnosis of ulcerative diseases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This work was supported by the National Natural Science Foundation of China (No. 81703133) and the Natural Science Foundation of Hunan Province (No. 2021JJ40856).
Conflict of interest
The authors declare no conflict of interest.
References
- Calciphylaxis in end-stage kidney disease: outcome data from the United Kingdom Calciphylaxis Study. J Nephrol. 2021;34:1537-45.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Calciphylaxis: risk factors, diagnosis, and treatment. Am J Kidney Dis. 2015;66:133-46.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The Koebner phenomenon may contribute to the development of calciphylaxis: A case series. JAAD Case Rep. 2021;13:57-61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diagnosis and treatment of calciphylaxis in patients with chronic kidney disease. J Bras Nefrol. 2021;43:665-68.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Risk factors for calciphylaxis in Chinese hemodialysis patients: a matched case-control study. Renal failure. 2021;43:406-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pyoderma gangrenosum: an update on pathophysiology, diagnosis and treatment. Am J Clin Dermatol. 2017;18:355-72.
- [CrossRef] [PubMed] [Google Scholar]





