Translate this page into:
Cholesterol-embolisation syndrome presenting as retiform rash and purplish toes
Corresponding author: Dr. Dipankar De, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research (PIGMER), Chandigarh, India. dr_dipankar_de@yahoo.in
-
Received: ,
Accepted: ,
How to cite this article: Meena A, Dev A, Chatterjee D, De D. Cholesterol-embolisation syndrome presenting as retiform rash and purplish toes. Indian J Dermatol Venereol Leprol. 2024;90:849. doi: 10.25259/IJDVL_696_2023
Dear Editor,
Cholesterol-embolisation syndrome (CES) is a systemic disease due to dislodgement of atherosclerotic plaque materials, such as cholesterol crystals, from the aorta and its major branches to the distal circulation, causing ischaemic and inflammatory injury to multiple organs.1
A 57-year-old man, a chronic smoker with the history of hypertension, diabetes mellitus, coronary artery disease and dyslipidaemia presented with acute chest pain for 24 hours without any associated palpitation or shortness of breath. He had experienced two episodes of non-ST-elevation myocardial infarction (NSTEMI) in the past 6 months. He had undergone angioplasty followed by coronary stenting 15 days back. Subsequently, he developed multiple reddish to purple painful lesions on both lower limbs and buttocks along with painful ulcers on his penis. He also complained of bluish discoloration of his toes. On examination, purpuric macules distributed in a lacy pattern (retiform) were observed on the dorsal aspect of right forearm, buttocks, both thighs and lower legs [Figure 1a]. Some of these lesions showed central necrosis and crusting. There was bluish-purplish discolouration of all the toes in a mottled pattern, which also extended to the forefoot [Figure 1b]. Genital examination revealed two well-defined shallow ulcers on the shaft of the penis, with yellowish slough [Figure 1c].

- Retiform purpuric patches on knee with overlying erosions.

- Blue-purple discolouration of toes along with extension of mottling to forefoot.

- Shallow ulcers on shaft of penis with yellowish slough.
Laboratory evaluation revealed raised c-reactive protein (CRP) and eosinophilia with normal leucocyte count, sterile blood culture, and normal serum procalcitonin, D-dimer and coagulation profile. Computed tomography (CT)–guided angiography of both lower limbs showed diffuse atherosclerotic changes with significant bilateral common iliac artery disease and significant left renal artery stenosis. Histopathological examination revealed diffuse epidermal necrosis [Figure 2a and 2b]. Ischaemic changes were seen in the upper dermis along with scattered eosinophils, neutrophils and collagen degeneration. Dermal vessels showed nuclear debris, fibrin thrombi and cholesterol clefts within the lumen. Based on the clinical and histopathological findings, a diagnosis of CES was confirmed. In view of stabilizing the aortic plaque and attenuating the risk factors [Table 1], the treatment was optimised. Cessation of smoking was advised. The patient was started on rosuvastatin 20 mg, telmisartan 40 mg, amlodipine 10 mg and nitroglycerin 2.6 mg twice daily, along with a combination of aspirin and clopidogrel with dosing of 75 mg each. He was also started on oral prednisolone at a dose of 30 mg which was tapered rapidly. Purpura fulminans can also be considered as a differential diagnosis but the lesions are larger with retiform purpura in the setting of sepsis or disseminated intravascular coagulation which was not present in this patient.
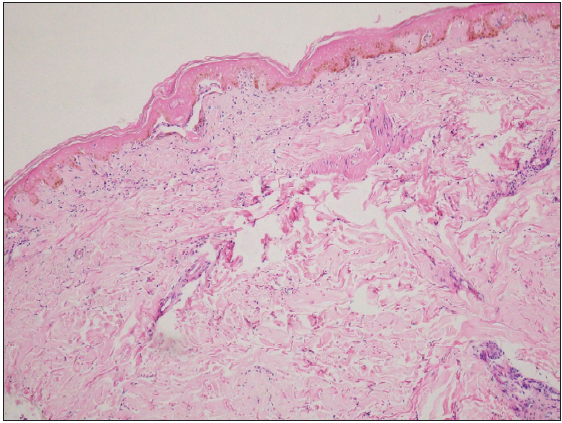
- Histopathological examination of skin biopsy specimen revealed epidermal necrosis and ischaemic changes in upper dermis. (Haematoxylin and eosin staining, 100×)
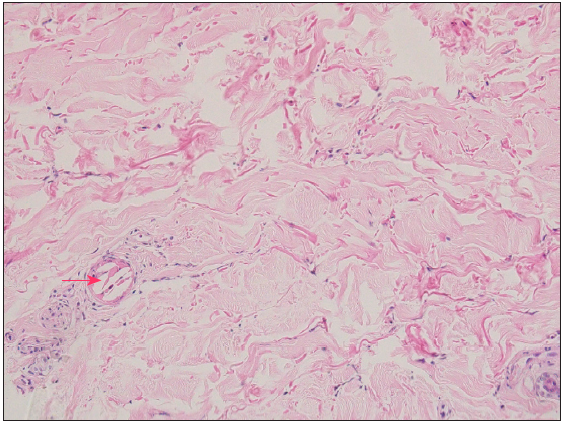
- Nuclear debris, fibrin thrombi, along with cholesterol clefts (red arrow) seen within the lumen of dermal vessels. Mixed inflammatory infiltrate comprising of scattered eosinophils and neutrophils are also seen along with collagen degeneration. (Haematoxylin and eosin staining, 400×)
| Interventional vascular procedure | Cardiovascular surgery |
|---|---|
| Hypertension | Old age |
| Smoking | Diabetes mellitus |
| Male sex | Aortic aneurysm |
| Anticoagulation | Increased inflammation |
| Thrombolytic treatment | Hyperlipidaemia |
CES is becoming common with the advent of endovascular treatments and thrombolytic therapies.2 Among angiographic procedures, coronary angiography is the most common intervention causing CES, with incidence of 0.06%–1.8%, especially by the femoral approach.3
Clinical manifestations include constitutional symptoms (fever, anorexia, weight loss, fatigue and myalgias), signs of systemic inflammation (anaemia, thrombocytopenia, leucocytosis, elevated erythrocyte sedimentation rate and c-reactive protein levels, hypocomplementemia), hypereosinophilia, acute-onset diffuse neurologic deficit, acute renal failure, gut ischaemia, livedo reticularis and blue-toe syndrome. Reported incidence of cutaneous manifestations ranges from 35% to 96% of patients with CES.4 The most frequent dermatological manifestations are livedo reticularis (49% of patients with skin manifestations), gangrene (35%), cyanosis (28%), ulceration (17%), nodules (10%) and purpura (9%). In the lower extremities, it may lead to sudden development of purple or blue toes (hence the term blue toe syndrome).5 End organ damage can occur, with acute renal failure having the worst prognosis.
Secondary preventive measures include aspirin, statins, smoking cessation, weight control, blood pressure, and glycaemia [Figure 3]. Invasive interventional studies should be avoided in patients with CES. However, if cardiac intervention becomes necessary, a radial approach has shown to have lower risk of cholesterol embolism as compared to a femoral approach.6 Treatment options are limited and supportive measures to prevent organ failure is the mainstay. Statins have been reported to be beneficial, with improved cutaneous manifestations and renal outcomes.7 Beneficial effects with anti-inflammatory drugs, such as corticosteroids, cyclophosphamide and colchicine have also been observed. Overall, prognosis is poor, with mortality rates as high as 80%.6
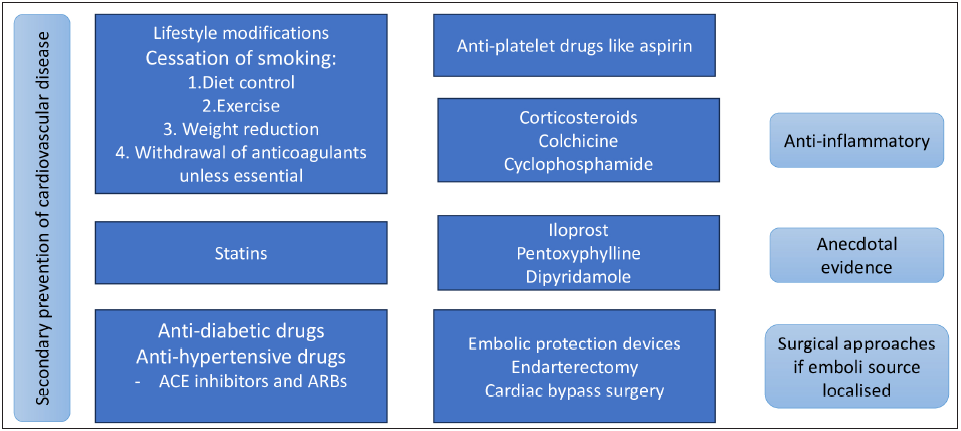
- Flow chart on treatment guidelines of cholesterol emobolisation syndrome.
Due to the high risk of end organ damage, especially renal failure, a high index of suspicion must be maintained in patients with the above-mentioned constellation of cutaneous and systemic symptoms in patients of large vessel disease who have recently undergone an invasive endovascular procedure. As treatment options are limited, early diagnosis forms the crux of management. CES syndrome is a rare complication of common procedures; such patients may be referred to a dermatologist in view of skin lesions. We must be aware of this condition for early diagnosis and timely management of such patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Cholesterol embolization syndrome. Circulation. 2010;122:631-41.
- [CrossRef] [PubMed] [Google Scholar]
- Fatal course of cutaneous cholesterol embolization syndrome: A case report. Int J Low Extrem Wounds. 2023;22:753-8.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of atheroembolic renal failure after coronary angiography. A prospective study. Angiology. 1997;48:609-13.
- [Google Scholar]
- Cholesterol crystal embolization: An atherosclerotic disease with frequent and varied cutaneous manifestations. J Eur Acad Dermatol Venereol. 2003;17:504-11.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation and management of cholesterol embolization and the blue toe syndrome. Curr Opin Cardiol. 1996;11:533-42.
- [CrossRef] [PubMed] [Google Scholar]
- Cholesterol-embolization syndrome: Current perspectives. Vasc Health Risk Manag. 2019;15:209-20.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Potential therapeutic effect of simvastatin on progressive renal failure and nephrotic-range proteinuria caused by renal cholesterol embolism. Am J Med Sci. 2001;322:50-2.
- [CrossRef] [PubMed] [Google Scholar]





