Translate this page into:
Intradermal vitamin C: A new paradigm in the treatment of exogenous ochronosis
Corresponding author: Dr. Abhishek R Parekh, Department of Dermatology, Venereology and Leprosy, Dr. Kiran C. Patel Medical College and Research Institute, Bharuch, India. om10abhi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gulwani PR, Parekh AR, Shah HA. Intradermal vitamin C: A new paradigm in the treatment of exogenous ochronosis. Indian J Dermatol Venereol Leprol. 2024;90:378-80. doi: 10.25259/IJDVL_890_2023
Dear Editor,
Exogenous ochronosis is caused by prolonged use of hydroquinone-containing skin-lightening creams, leading to dark brown to blue-black skin pigmentation. Although multiple treatment options are available, the outcomes are frequently erratic, unpredictable and rarely satisfying. We have attempted to utilise intradermal vitamin C (ascorbic acid) for the treatment of exogenous ochronosis.
A 45-year-old Indian man visited the dermatology department with complaints of hyperpigmentation on both cheeks. He had been using various depigmenting creams on and off for 9 years; including application of unsupervised triple combination cream (2% hydroquinone, 0.05% tretinoin and 0.1% mometasone furoate) in the past 3 years. For the last 3 months, he reported worsening of pigmentation and appearance of erythema on both cheeks.
Clinical examination revealed presence of bilaterally symmetrical blue-black macules in a speckled pattern, with erythematous backgrounds on both cheeks [Figures 1a, 1b]. The prayer sign was observed over the forehead. Rest of the physical examination was unremarkable. Dermoscopy revealed irregular, dark brown to black globular, annular and arciform structures, which obliterated some follicular openings and formed a curvilinear and worm-like pattern [Figure 1c]. Additionally, marked telangiectasia was evident in the background. The histological examination revealed a thinned-out epidermis, dense elastotic degeneration in superficial dermis and deposition of extracellular, yellowish-brown, banana-shaped, sickled or round ochronotic bodies [Figure 2].

- Bilaterally symmetrical blue-black macules in a speckled pattern, with erythematous backgrounds present on both cheeks.
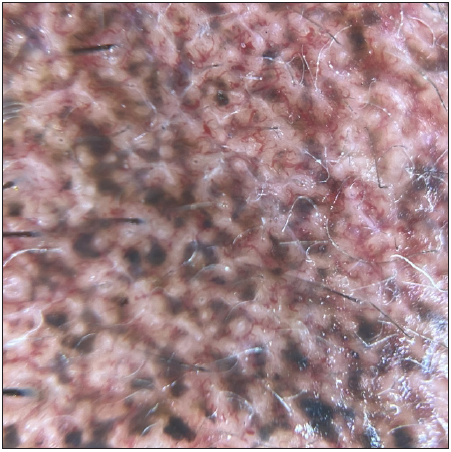
- Pre-treatment: Dermoscopy showed irregular, dark brown to black globular, annular and arciform structures forming a curvilinear and worm-like pattern on telangiectatic background (DermLite DL4, polarised mode, 20x).
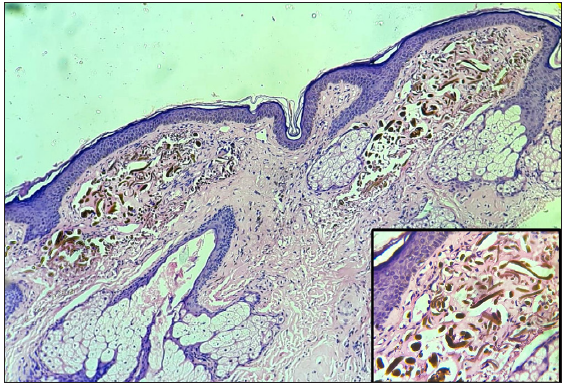
- Thinned-out epidermis, elastotic degeneration in the superficial dermis along with the deposition of extracellular, yellowish-brown, banana-shaped, sickled or round ochronotic bodies, (Haematoxylin and Eosin, 40x) better visualised in inset image (Haematoxylin and Eosin, 400x).
Based on clinical, dermoscopic and histological findings, the patient was diagnosed to have exogenous ochronosis. He was strictly advised to avoid using any depigmenting cream and was prescribed broad spectrum sunscreen against ultraviolet, infrared and visible light. In addition, a barrier repair moisturiser containing hyaluronic acid, ceramide, squalene and lecithin was prescribed for one month. To address the pigmentation, 0.05–0.1 mL of vitamin C (500 mg/5 mL) was injected at 1 cm interval intradermally up to 1 mL (100 mg) per sitting every four weeks for three cycles. The patient experienced mild-to-moderate pain during the procedure. After one month, erythema subsided completely (100%) and after three months, 80% improvement in the hyperpigmentation was observed [Figures 3a, 3b and 3c].

- Three months post-treatment: 80% improvement in blue-black macules was observed on both cheeks along with subsidence of erythema.
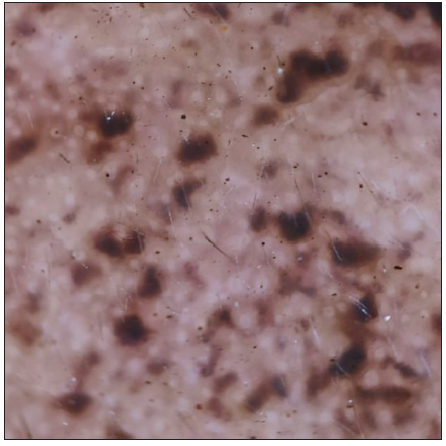
- Three months post-treatment: Dermoscopy showed few and smaller dark brown to black globular, annular and arciform structures along with subsidence of telangiectasia in the background (DermLite DL4, polarised mode, 20x).
Unsupervised and prolonged use of depigmenting creams containing hydroquinone over larger areas or in excessive amounts is the most prevalent cause of exogenous ochronosis. Various pathways contribute to understanding how hydroquinone triggers exogenous ochronosis; and vitamin C strategically targets and mitigates these mechanisms [Figure 4]. One plausible mechanism is the formation of homogentisic acid (HGA) and subsequent benzoquinone (BQ). Later it binds with connective tissue to form aberrant elastic fibres, which then give rise to ochronotic bodies.1,2 It is seen that in alkaptonuria, the effect of BQ on tissue could be prevented by inhibiting the conversion of HGA to BQ by treatment with high dose of vitamin C.3 We have speculated that the reduction of BQ back to HGA can also occur with the use of vitamin C in exogenous ochronosis. Also, vitamin C acts as a potent antioxidant.

- Flowchart showing pathogenesis of hydroquinone-induced exogenous ochronosis and multifaceted effect of vitamin C on various steps of pathogenesis.
The water solubility and charged nature of vitamin C pose a challenge in its effective delivery through the physical barrier of terminally differentiated epidermal cells. Despite the availability of various topical formulations in the market, their effectiveness in penetrating the dermis and converting to the active form of vitamin C remains limited. Even the use of lipophilic preparations increases vitamin C absorption proportionally with concentration up to a maximum of 20%.4 To overcome these limitations, we have used intradermal injection of vitamin C, which has given promising result in our patient.
Literature mentions the adjuvant role of intradermal injection of vitamin C for achieving a beneficial effect in melasma. A comparative study by Balevi A et al.5 showed improved outcomes after 6 months in melasma patients who received both Vitamin C mesotherapy and salicylic acid peeling (mean reduction of MASI score by 68.11%) compared to those who underwent salicylic acid peeling alone (mean reduction of MASI score by 13.17%). A similar observation was made by Pazyar N et al.6 who demonstrated better outcomes with intradermal injection of tranexamic acid and ascorbic acid compared to tranexamic acid alone. The copper ions on the enzyme tyrosinase are chelated by vitamin C, which inhibits the synthesis of melanin, this being the suggested explanation here. However, efficacy of intradermal injection of vitamin C alone in melasma and exogenous ochronosis remains unexplored.
To conclude, our case highlights that intradermal injection of vitamin C may be a promising modality for exogenous ochronosis. However, long-term research involving a larger number of patients with longer follow up is needed to establish its efficacy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Exogenous ochronosis and pigmented colloid milia from hydroquinone bleaching creams. Br J Dermatol. 1975;93:613-22.
- [CrossRef] [PubMed] [Google Scholar]
- Ochronosis-like pigmentation from bleaching creams. Arch Dermatol. 1985;121:1239-40.
- [Google Scholar]
- Vitamin C in dermatology. Indian Dermatol Online J. 2013;4:143-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Salicylic acid peeling combined with vitamin C mesotherapy versus salicylic acid peeling alone in the treatment of mixed type melasma: A comparative study. J Cosmet Laser Ther. 2017;19:294-9.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of intradermal injection of tranexamic acid and ascorbic acid versus tranexamic acid and placebo in the treatment of melasma: A split‐face comparative trial. Health Sci Rep. 2022;5:e537.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





