Translate this page into:
Cutaneous argyria: A rare cause of occupational dermatoses
Corresponding author: Dr. Suresh Kumar Jain, Department of Dermatology, Venereology and Leprosy, Government Medical College, Kota, India. drsuresh253@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shrivastava H, Kushwaha R, Joshi S, Jain SK. Cutaneous argyria: A rare cause of occupational dermatoses. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1001_2023
Dear Editor,
Silver is a naturally occurring metal that has no known physiological or biological function in the human body. Its concentration in a normal healthy person is <3 mcg/L.1 For occupational exposure a recommended exposure limit of 0.01 mg/m3 in the air for both metallic and soluble compounds of silver and two separate exposure limits of 0.1 mg/m3 for metallic silver and 0.01 mg/m3 for soluble silver compounds are established by the National Institute for Occupational Safety and Health and the American Conference of Governmental Industrial Hygienists, respectively.1
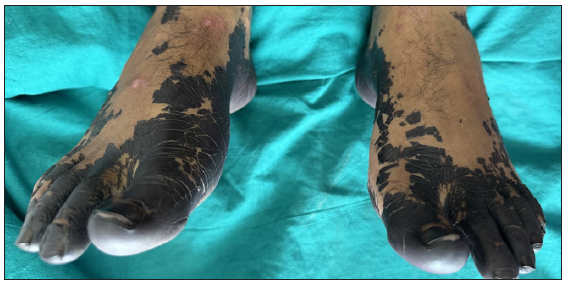
We report a case of a 34-year-old man who presented in the out-patient department, with localised, ashy-grey homogeneous pigmentation of the plantar surface of both feet with pigmentation extending on to the dorsal surface of the feet and nails. He was a worker in a gold refinery and was accidentally exposed due to a leakage of silver nitrate used in extracting pure gold from its ore. The leaked solution percolated through his shoes and came in direct contact with his feet. The worker immediately diluted the solution by adding water but the solution that had entered his shoes caused localised ashy-grey pigmentation of his feet that was noticed after three hours since no immediate symptoms were felt by the patient. On examination, there were thick crusted plaques on both feet [Figure 1] associated with burning and itching along with bluish-black discolouration of all toenails [Figure 2]. He complained of oozing of bluish-black fluid from his feet whenever he stepped in sunlight. Dermoscopy (using DermLite DL3N) showed a shiny, homogeneous network of grey-blue pigmentation with multiple fissures giving an appearance of ‘leaf-venation’ [Figure 3]. These fissures were less pigmented as compared to the surrounding areas. Multiple white dots were present on the dermoscopy over the soles. The blue-grey colour of the dermoscopy structures was most probably produced via a refringence phenomenon (Tyndall effect), which gives the appearance of a brown pigment that is located deep within the dermis.2

- Grey-black pigmentation on both feet.
- Pigmentation extending on to the the dorsum of feet and showing blue-grey pigmentation of nails.

- Dermoscopy from sole showing ‘leaf venation’ pattern (DermLite DL3N, non-polarised 10x).
Based on the history, examination and dermoscopic findings, a diagnosis of localised cutaneous argyria was made. A skin biopsy was not taken. The patient was counselled about the benign nature of his condition. He was given symptomatic with antihistaminics and emollients. On follow-up after 15 days, he presented with focal areas of peeled crusted plaque exposing raw, slightly erythematous, wrinkled and macerated skin. There was adherent grey plaques on the heels and plantar side of the great toe. He was advised not to wear shoes, air dry and use a moisturiser.
Argyria can be of two types – generalised or localised. Generalised argyria is a systemic condition which presents as blue-grey pigmentation of skin, nails and mucous membranes due to ingestion or inhalation of silver or its compounds. Silver is used in various ayurvedic preparations and ingestion of colloidal silver is thought to have medicinal properties which usually results in generalised pigmentation. It is an irreversible condition with some benefits seen in cosmetic appearance with the use of Q-switched Nd-YAG laser therapy. Silver is suggested to be deposited in the dermis in a chemically stable and inactive form. It is also believed that argyria occurs through the eccrine sweat ducts because the metal is most concentrated around the secretion site of the sweat glands.3 It remains confined to a particular site and is usually seen in silversmiths, people using silver containing earrings, hair dyes, antique pieces or as in our case as a sequelae of occupational exposure. It is a benign condition and the pathogenesis is not fully understood. Interestingly, the blue-grey skin discolouration observed in both generalised and localised cutaneous argyria is most prominent in sun-exposed areas of the skin. Skin discolouration due to silver exposure is intensified in the presence of sunlight by the reduction of silver and can be further exacerbated by the silver-induced increase in melanin.4 The condition is insidious in onset and should be differentiated from other causes of cutaneous pigmentation which can also be due to systemic disorders. Various recent case reports published on localised cutaneous argyria are listed in Table 1. However, nowadays, such case reports have declined due to advanced equipment usage in occupational settings.
| Authors | Site of lesion | Exposure source |
|---|---|---|
| Georgiadou et al5 (2021) | Hand | Silver jewellery handling |
| Regina M. Ondrasik et al.4 (2020) | Hand and feet | Topical silver nitrate |
| Sittiroj Arunkajohnsak et al.6 (2020) | Face, hands, wrists, legs, feet | Acupuncture |
| Verena Isak et al.7 (2019) | Face | Topical silver sulfadiazine |
| Seung Gi Hong et al.3 (2019) | Ear | Earrings |
Silver has various medicinal uses. As its use is now limited in healthcare practices, occurrence of conditions due to its toxicity have declined. But we should always be alert to evaluate metal toxicity in cases of cutaneous pigmentation. To the best of our knowledge, a detailed description of dermoscopic appearance in cutaneous argyria has not been extensively reported.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Argyria an unrecognized cause of cutaneous pigmentation in Indian patients: A case series and review of the literature. Indian J Dermatol Venereol Leprol. 2013;79:805-11.
- [CrossRef] [PubMed] [Google Scholar]
- Argyria mimicking a blue nevis: Dermoscopy features. Ann Bras Dermatol. 2013;88:452-5.
- [CrossRef] [PubMed] [Google Scholar]
- Localized cutaneous argyria mimicking blue nevus after wearing earrings. Ann Dermatol. 2019;31:666-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A clinical mimicker of melanoma with distinctive histopathology: Topical silver nitrate exposure. J Cutan Pathol. 2020;47:1205-10.
- [CrossRef] [PubMed] [Google Scholar]
- Occupational localized cutaneous argyria with pseudo-ochronosis in a jeweler. Am J Dermatopathol. 2021;43:822-6.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of acupuncture-induced argyria using Q-switched 1064-nm Nd:YAG laser. JAAD Case reports. 2020;10:984-7.
- [CrossRef] [PubMed] [Google Scholar]
- A rare case of localized argyria on the face. Case Rep Dermatol. 2019;11:23-7.
- [CrossRef] [PubMed] [Google Scholar]






