Translate this page into:
Prurigo pigmentosa: A retrospective study of 11 patients
Corresponding author: Dr. Na Wang, Department of Dermatology, Hospital for Skin Diseases, Shandong First Medical University, Jinan, Shandong Province, P.R. China. kathy1112.hi@163.com
-
Received: ,
Accepted: ,
How to cite this article: Liu Y, Li J, Zhou G, Wang J, Chen X, Chen S, et al. Prurigo pigmentosa: A retrospective study of 11 patients. Indian J Dermatol Venereol Leprol. 2024;90:661-5. doi: 10.25259/IJDVL_751_2023
Dear Editor,
Prurigo pigmentosa (PP) is a rare inflammatory dermatosis predominantly affecting young women. Its pathogenesis remains unclear. In the last decade, low-carb and keto diets have gained popularity, possibly increasing the number of PP cases.1 In this study, we retrospectively analysed 11 PP patients treated at a tertiary hospital between March 2010 and September 2020. PP was diagnosed using the criteria adapted by Boer et al.2 Clinically, PP presents as pruritic urticarial papules, papulovesicles, and vesicles arranged in reticular pattern and distributed symmetrically on the back, neck, and chest. Lesions involute in a matter of days, leaving behind reticular pigmentation. Histopathologically, prurigo pigmentosa begins with a superficial perivascular infiltrate of neutrophils. Shortly after, neutrophils are scattered in dermal papillae and then sweep rapidly through the epidermis in which spongiosis, ballooning, and necrosis are accompaniments, eosinophils and lymphocytes come to predominate over neutrophils in a dermal infiltrate that assumes a patchy lichenoid pattern. Intraepidermal vesiculation follows in spongiosis and ballooning and, sometimes, subepidermal vesiculation occurs at the dermo-epidermal junction.
The etiology and pathogenesis of PP are unclear until now. The chronic and recurrent nature of PP and good therapeutic effect of doxycycline in PP means that PP is idiopathic inflammatory dermatitis. Acetyl-CoA acyltransferase 1 (ACAT1) is a key enzyme catalysing mitochondrial ketone body production. ACAT1 plays a catalytic role in ketolysis, ketogenesis, and fatty acid oxidation.3 Vasostatin-1 suppresses the inflammatory macrophage (M1) phenotype and lipopolysaccharide-induced IL-6 secretion via nuclear factor-κB in macrophages, which suppresses oxidised low-density lipoprotein-induced foam cell formation associated with ACAT-1 and CD36 down regulation in macrophages.4 IL-8 is a major chemoattractant for neutrophilic activation and regulation, and also promotes normal T cell expression.1 So, we hypothesised that ACAT1, IL-8 and IL-6 may be involved in the pathogenesis of PP. Their clinico-pathological features are presented in Table 1, and Figures 1 and 2. None of the patients had systemic diseases (e.g., diabetes). We aimed to determine whether ACAT1 is related to PP and corroborate the roles of IL-6 and IL-8 in the clinicopathological features of PP in an ethnic Chinese population.
| Pt. | Age/Sex/Race | Duration | Symptoms | Potential trigger | Clinical features | Histopathological findings | Treatment and follow-up |
|---|---|---|---|---|---|---|---|
| 1 | 16/female/Chinese | 1 month | Not mentioned | Dieting | Reticular, erythematous plaques and reticular hyperpigmented areas on the chest | Epidermal hyperkeratosis, parakeratosis, prominent acanthosis, edema in the papillary dermis, nuclear dust, one enlarged hair follicle with a neutrophil abscess and surrounding lymphocytes, neutrophils and eosinophils | Tetracycline orally 500 mg twice daily. Slight residual pigmentation on the chest after 3 months of follow-up. |
| 2 | 19/female/Chinese | 1 month | Pruritic | Ketogenic diet | Pruritic, erythematous papules, excoriations, and marked reticular hyperpigmentation on the neck, upper back, and chest | Epidermal hyperkeratosis, intercellular edema, basal cell degeneration, perivascular lymphohistiocytic and neutrophilic infiltrate, and nuclear dust | Tetracycline orally 500 mg twice daily. Recovered without residual pigmentation after 1 month of follow-up. |
| 3 | 9/male/ Chinese | 3 months | Pruritic | Low-carb diet | Pruritic, reticular, erythematous plaques and reticular hyperpigmented areas on the chest | Epidermal hyperkeratosis, mild parakeratosis, prominent acanthosis, infiltration of lymphocytes and individual eosinophils in the entire dermis | Carbohydrate diet. Residual reticular hyperpigmentation after 1 year of follow-up. |
| 4 | 18/male/ Chinese | 1.5 months | Pruritic | Ketogenic diet | Severe pruritic, erythematous macules and reticular hyperpigmentation on the chest | Epidermal focal hypokeratosis, prominent acanthosis, infiltration of mononuclear cells in the superficial dermis | Tetracycline orally 500 mg twice daily. Followed up for 8 months by phone; residual reticular hyperpigmentation on the chest. |
| 5 | 18/female/Chinese | 4 years | NG | Fasting for 15 h per day | Erythematous macules and reticulate hyperpigmentation on the forehead, neck, upper back and chest | Epidermal slight hyperkeratosis, prominent acanthosis, individual dyskeratosis, basal cell degeneration, slight mononuclear cell migration, slight perivascular infiltration of mononuclear cells, and pigmentophages | Tetracycline orally 500 mg twice daily. Followed up for >3 months. Post-inflammatory hyperpigmentation resolved without any treatment. |
| 6 | 31/male/ Chinese | 4 years | NG | Low-carb diet | Erythematous macules and reticular hyperpigmentation on the back and chest | Epidermal hyperkeratosis, parakeratosis, focal intercellular edema, basal cell degeneration, slight mononuclear cell migration, slight perivascular infiltration of mononuclear cells | Carbohydrate diet. Tetracycline orally 500 mg twice daily. Lost to follow-up. |
| 7 | 24/female/Chinese | 2 years | Pruritic | None | Severe pruritic, erythematous macules and reticular hyperpigmentation on the back and chest | Epidermal mononuclear cell migration, mild infiltrate of lymphocytes, neutrophils, and a few eosinophils in the dermal papillae and perivascular areas, scattered pigment granules | Tetracycline orally 500 mg twice daily. Lost to follow-up. |
| 8 | 31/female/Chinese | 1 year | Pruritic | Ketogenic diet | Severe pruritic, erythematous macules and reticular hyperpigmentation on the back | Epidermal hyperkeratosis, parakeratosis, irregular epidermal thickening, necrosis of superficial keratinocytes, intercellular edema, lymphocyte migration, basal cell degeneration, perivascular infiltrate of lymphohistiocytic cells and neutrophils, and nuclear dust | Diet modification. Minocycline 50 mg bid. Lost to follow-up. |
| 9 | 19/male/ Chinese | 1 month | Pruritic | Low-carb diet, protein supplement | Erythematous macules and reticular hyperpigmentation on the back and chest | Epidermal hyperkeratosis, prominent acanthosis, perivascular infiltration of lymphocytes and individual eosinophils in the superficial dermis | Doxycycline 100 mg bid. Followed up for 3 months by phone. Slight residual reticular hyperpigmentation on the chest and back. |
| 10 | 26/male/ Chinese | 10 days | Pruritic | Low-carb diet | Erythematous macules and reticular hyperpigmentation on the back and chest | Epidermal hyperkeratosis, prominent acanthosis, perivascular infiltration of lymphocytes, and individual eosinophils in the superficial dermis | Minocycline 50 mg bid and carbohydrate diet, which rapidly resolved the symptoms. The patient was followed up for 7 months and had pigmentation for 3 months. |
| 11 | 35/female/Chinese | 1 month | NG | Low-carb diet | Erythematous macules and reticular hyperpigmentation on the back and chest | Mild epidermal acanthosis, superficial perivascular infiltrate, neutrophilic exocytosis, occasional apoptotic keratinocytes, and superficial perivascular lymphocytic infiltrate in the upper dermis | Minocycline 50 mg bid. Lost to follow-up. |
NG: Not Given

- Erythematous papules and plaques with reticular hyperpigmentation on the upper chest (patient 7).
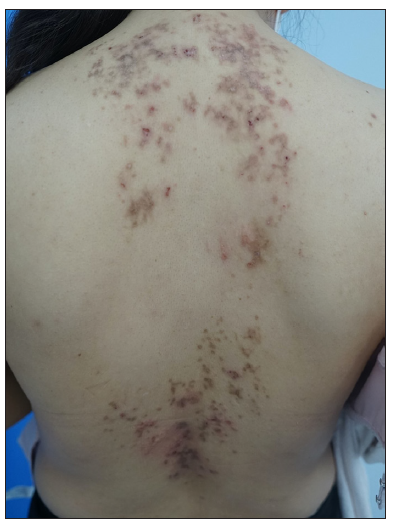
- Erythematous macules and reticular hyperpigmentation on the back (patient 8).

- Erythematous macules and reticular hyperpigmentation on the chest (patient 9).

- Erythematous papules with reticular hyperpigmentation on the chest and abdomen (patient 10).
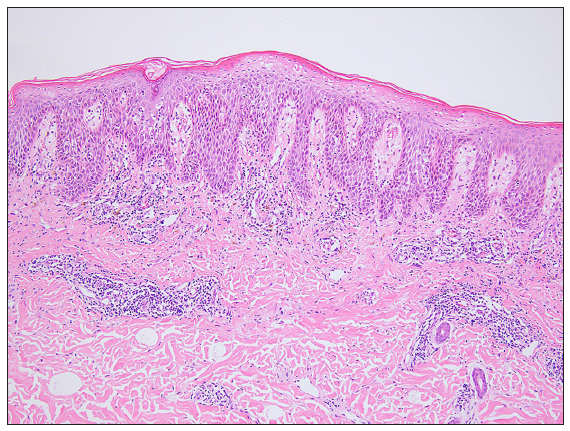
- Patient 8: Epidermal hyperkeratosis, parakeratosis, irregular epidermal thickening, necrosis of superficial keratinocytes, intercellular edema, lymphocyte migration, basal cell degeneration, perivascular infiltrate of lymphohistiocytic cells and neutrophils, and nuclear dust (Haematoxylin and Eosin, 100x).
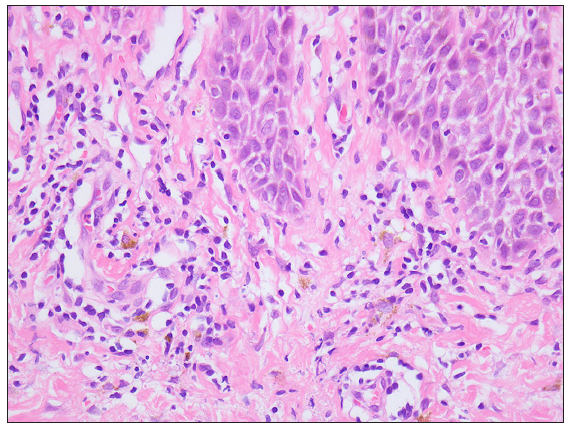
- Patient 8: Epidermal hyperkeratosis, parakeratosis, irregular epidermal thickening, necrosis of superficial keratinocytes, intercellular edema, lymphocyte migration, basal cell degeneration, perivascular infiltrate of lymphohistiocytic cells and neutrophils, and nuclear dust (Haematoxylin & Eosin, 400x).

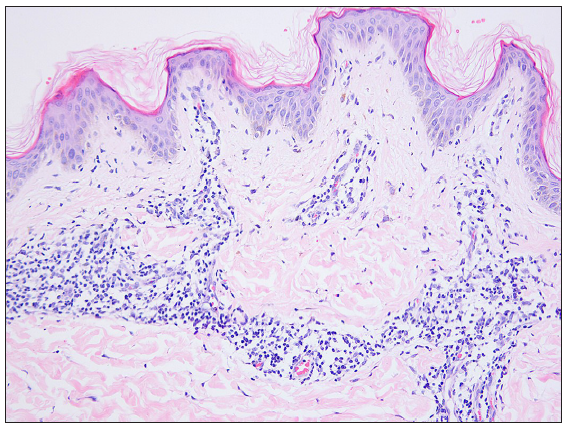
- Patient 9: Epidermal hyperkeratosis, prominent acanthosis, perivascular infiltration of lymphocytes and individual eosinophils in the superficial dermis (Haematoxylin & Eosin stain, 100x).
- Patient 9: Epidermal hyperkeratosis, prominent acanthosis, perivascular infiltration of lymphocytes and individual eosinophils in the superficial dermis (Haematoxylin & Eosin stain, 200x).
The median age at the time of PP diagnosis was 22.3 years (range: 9–35 years); the female-to-male ratio being 6:5. The diagnostic delay ranged from 10 days to 4 years. Most patients responded well to doxycycline and tetracycline, leaving residual pigmentation. Immunohistochemistry (IHC) revealed slightly elevated lesional IL-6 and IL-8 expression in PP relative to control skin samples from eczema patients (P > 0.05). The PP and control groups were matched for age, sex, and lesion site. All the slices were matched in the three groups before IHC. All PP skin samples were negative for ACAT1 compared to controls. [Supplementary Table 1 and Supplementary Figure 1].
PP was first described by Nagashima in 1978. Its precise etiology and pathogenesis remain unclear but may involve dietary modification. PP has been associated with fasting, dieting (especially ketogenic diets), diabetes mellitus, conditions that increase ketone body production, mechanical irritation, sweating, and emotional stress.5 In our series, the association with diet was striking, and a history of dietary changes prior to PP development was obtained in 80% of patients.
Resolution of PP has been reported with dietary modification (as in patients 3, 6, and 8 in our series) or with treatment for dehydration.5 Antibiotics that affect neutrophil chemotaxis, including minocycline and doxycycline, are usually effective. Colchicine may be of therapeutic benefit,6 and narrow-band ultraviolet-B therapy may be an alternative treatment.7
Ketosis may play a major role in the pathogenesis of PP.5 Urine ketone levels were measured in 4 patients in this study, all of whom had levels of 4 +. A study1 has reported that IL-6 is strongly expressed in PP skin lesions, but this could not be confirmed in our patients. ACAT1 deficient mice develop severe skin xanthomas and abnormal accumulation of subcutaneous cholesterol, which suggests the importance of ACAT in maintaining cholesterol metabolism.8 Studies on the specific roles of ACAT-1, IL-6, and IL-8 in PP are lacking. In our study, all PP lesions were negative for ACAT1, implying that the null hypothesis is probably not true.
Differential diagnoses like confluent and reticulated papillomatosis, contact dermatitis, urticaria, erythema multiforme, dermatitis herpetiformis, and medication-induced rashes should be excluded, since the progression of PP in three stages is typical and biopsy can easily diagnose PP.
More research is necessary for understanding the mechanism of PP including the role of genetics, and the causal relevance of anecdotal associations. The rarity of PP makes it difficult to perform large-scale studies, which are warranted for its deeper understanding. Owing to the small sample size, we failed to conduct a stratified analysis of the diet. Because of the retrospective study design, we could not collect data on urine ketone levels, nor could we analyse the relationship between ketones and PP.
We conclude that PP is easily misdiagnosed. IL-6 plays an important role in PP skin lesions, but ACAT1 may not be involved in its pathogenesis.
Ethical approval
This study was approved by the Ethics Committee of Shandong Provincial Institute of Dermatology and Venereology and was conducted according to the principles of the Declaration of Helsinki. The approve date was on Sep12, 2020 and the approval No. is 20200912KYKTKS003.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This work was funded by the National Natural Science Foundation of China (81903230), Shandong Provincial Medical and Health Science and Technology Development Plan (202004120262).
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Prurigo pigmentosa: A clinicopathological study and analysis of associated factors. Int J Dermatol. 2011;50:36-43.
- [CrossRef] [PubMed] [Google Scholar]
- Prurigo pigmentosa: A distinctive inflammatory disease of the skin. Am J Dermatopathol. 2003;25:117-29.
- [CrossRef] [PubMed] [Google Scholar]
- The recent insights into the function of ACAT1: A possible anti-cancer therapeutic target. Life Sci. 2019;232:116592.
- [CrossRef] [PubMed] [Google Scholar]
- Inhibitory effects of vasostatin-1 against atherogenesis. Clin Sci (Lond). 2018;132:2493-507.
- [CrossRef] [PubMed] [Google Scholar]
- Ketogenic diet-induced prurigo pigmentosa: A rising association. Int J Dermatol. 2022;61:779-82.
- [CrossRef] [PubMed] [Google Scholar]
- Crisaborole: An emerging therapy for prurigo pigmentosa. J Eur Acad Dermatol Venereol. 2022;36:e441-e443.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment with narrowband ultraviolet B phototherapy in prurigo pigmentosa. J Eur Acad Dermatol Venereol. 2021;35:e796-e798.
- [CrossRef] [PubMed] [Google Scholar]
- ACAT1 deficiency increases cholesterol synthesis in mouse peritoneal macrophages. Atherosclerosis. 2006;186:267-74.
- [CrossRef] [PubMed] [Google Scholar]





