Translate this page into:
Collision of basal cell carcinoma and atypical fibroxanthoma
Corresponding author: Dr. Héctor Perandones González, Department of Dermatology, Complejo Asistencial universitario de León, C/Altos de Nava S/N, León-24071, Spain (Hospital Universitario de León). hectorperan@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Perandones González H, Valladares Narganes LM, González Morán MA, Rodríguez prieto MÁ. Collision of basal cell carcinoma and atypical fibroxanthoma. Indian J Dermatol Venereol Leprol. 2024;90:500-3. doi: 10.25259/IJDVL_220_2021
Dear Editor,
A collision tumor is composed of two or more different cellular populations within the same lesion. Although this phenomenon is uncommon, a wide variety of either benign or malignant collisions have been described. We report a collision of a basal cell carcinoma (BCC) and an atypical fibroxanthoma (AFX) in an octogenarian woman.
BCC is the most common malignant tumour in humans while AFX represents a rarer neoplasm.1,2 Occurrence of both these neoplasms at one site was first reported by Alves et al. in 2010.3 Since then, only two other cases have been reported.4,5 In this paper, we describe the clinical presentation, dermoscopy as well as pathological findings. We also discuss the different theories proposed in collision development.
An 84-year-old woman presented to our dermatology department for a slow growing tumor located at her temple, with episodes of spontaneous bleeding. Close inspection revealed a 3-cm diameter centrally ulcerated tumor [Figure 1a]. Polarized light dermoscopy demonstrated an amelanotic pinkish tumour with white structureless areas, irregular vessels, and a central serohaemorrhagic crust. We were able to identify a unique area with a large blue-grey ovoid nest [Figure 1b].
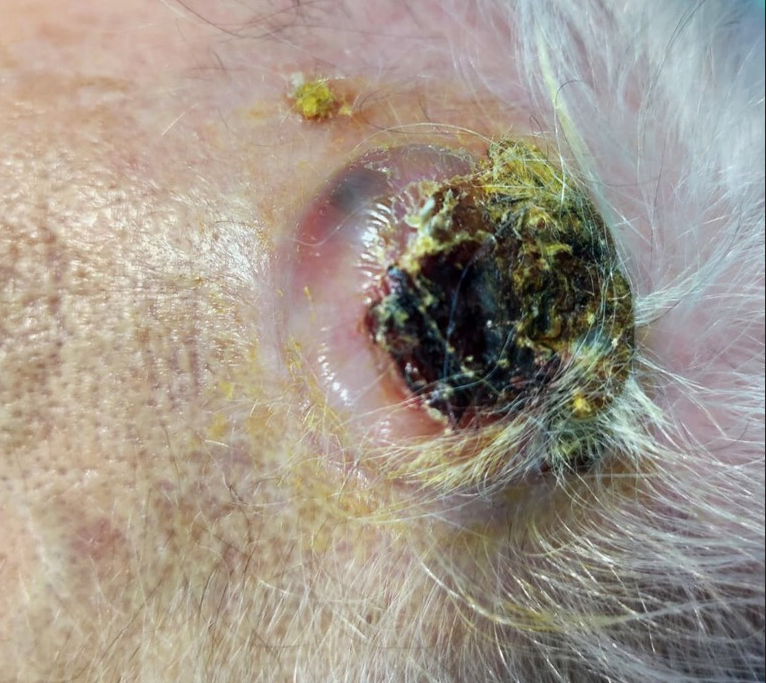
- A pink tumor with a central serohemorrhagic crust at the temple.
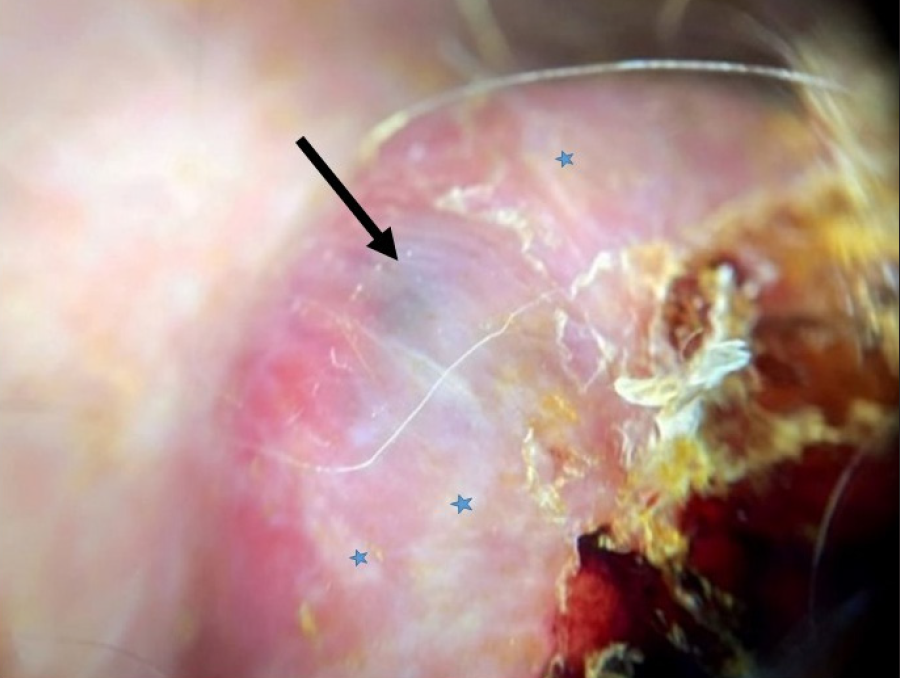
- Large blue-grey ovoid nest (black arrow) and structureless white areas (blue asterisk) on dermoscopy (Dermlite DL200 polarised).
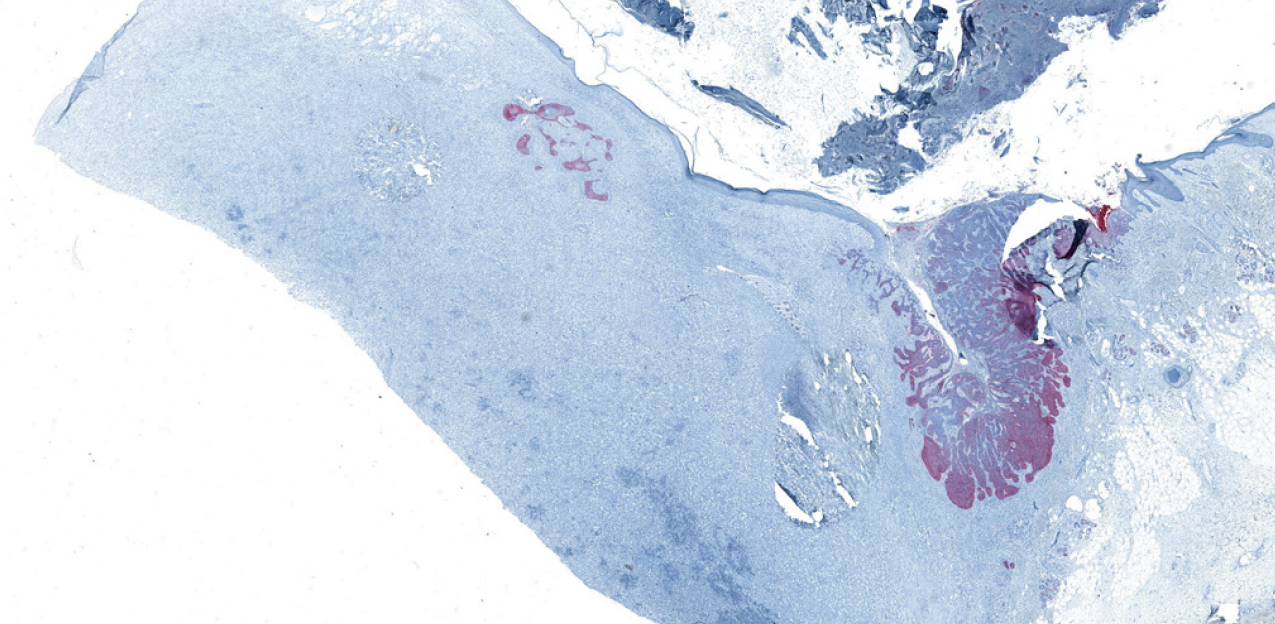
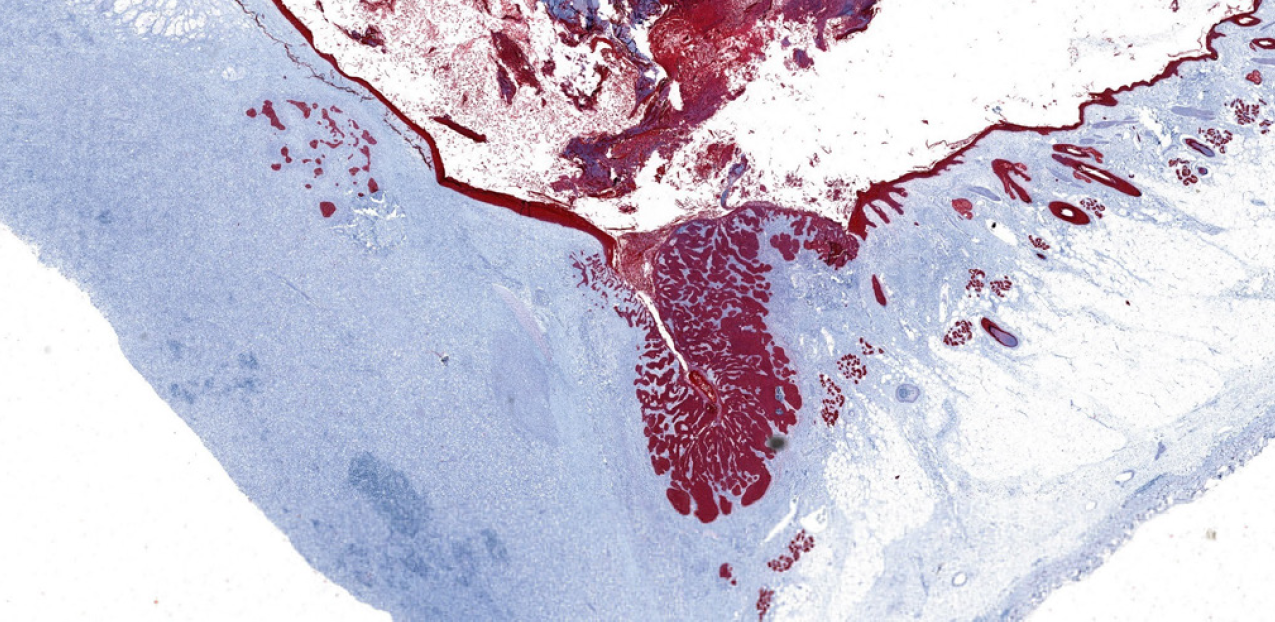
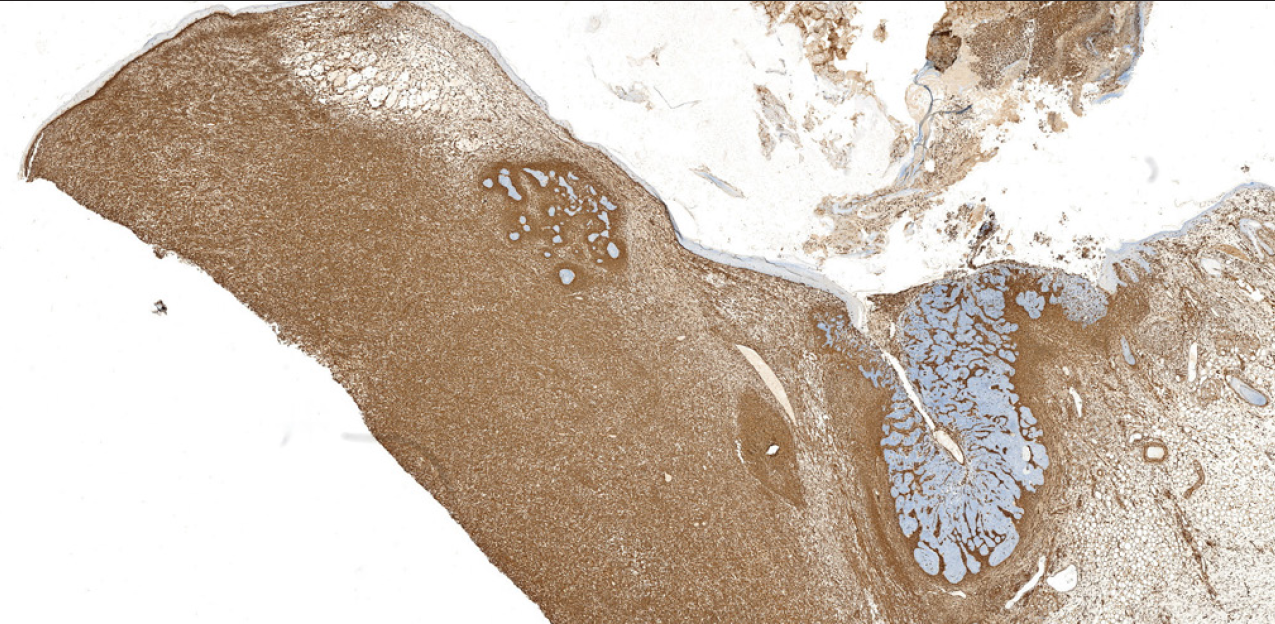
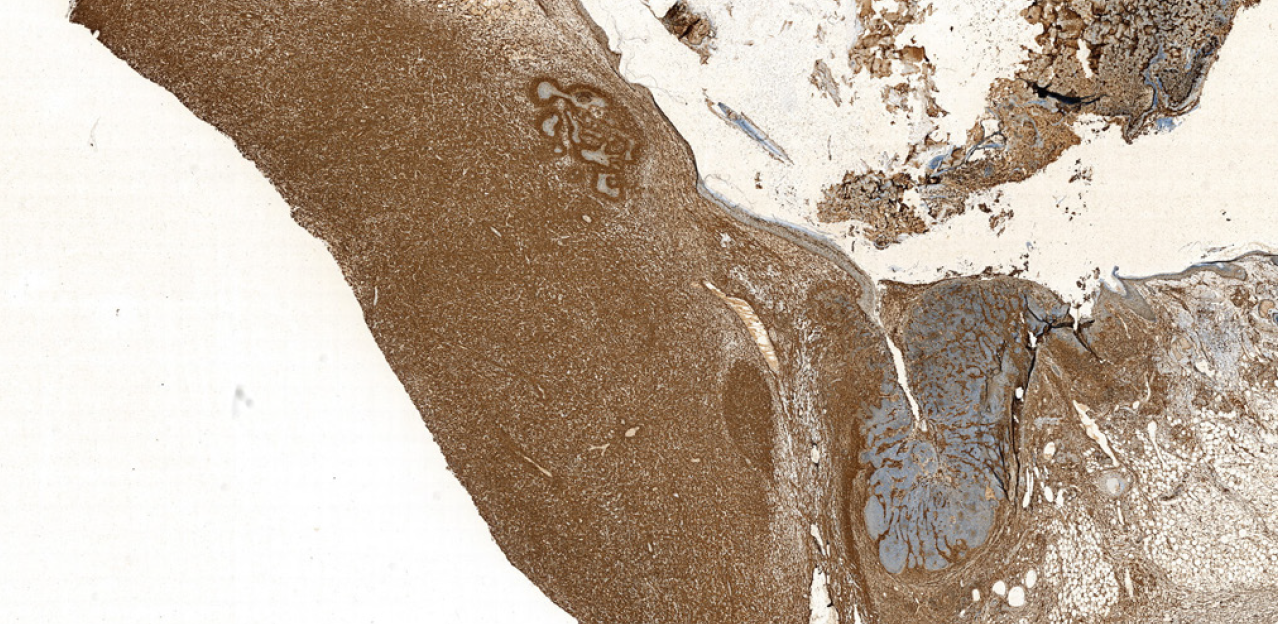
A wide margin excision was performed and sent for pathological study. Histological section revealed a dermal tumour without involvement of epidermis and subcutaneous tissue which was composed of spindle-shaped cells with highly pleomorphic nucleus and abundant mitosis. Occasional giant multinucleated cells were also noted. We did not find necrosis. Another section revealed interconnected tumor islands budding from epidermis. These aggregates were composed of basaloid cells with peripheral palisading of the nuclei and a retraction artifact from a mucinous stroma [Figures 2a–2d]. These classic superficial BCC islands were surrounded by the neoplastic spindle cell proliferation in the dermis.
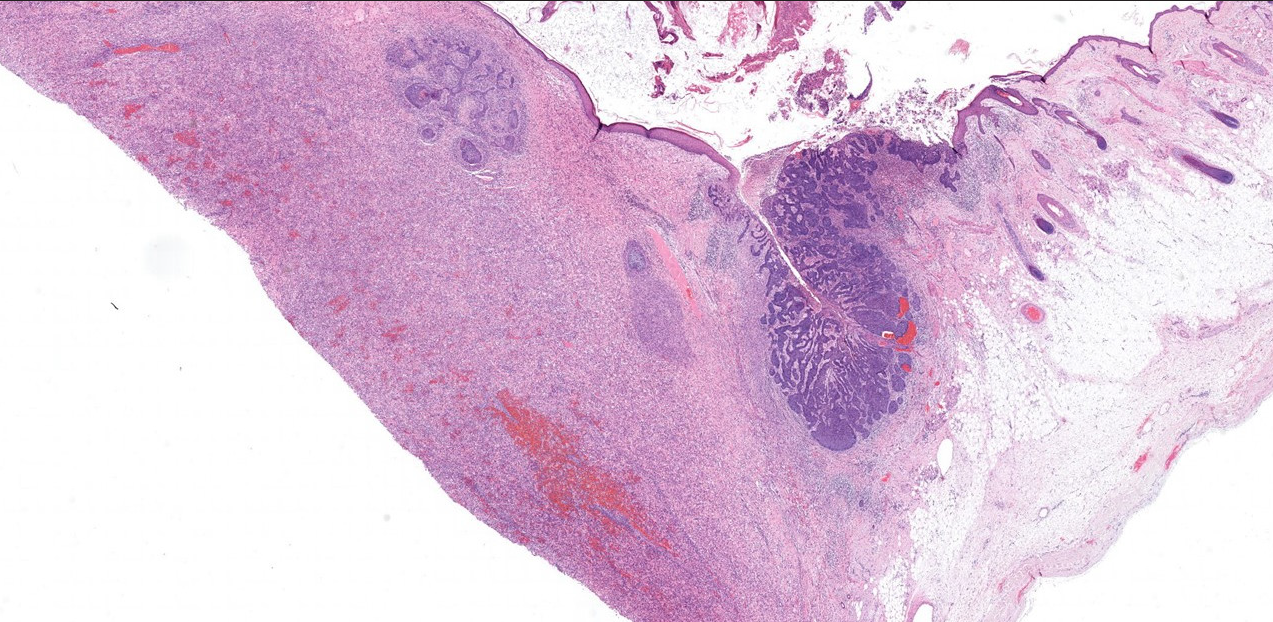
- Solar elastosis and two different proliferations present within the same lesion (Haematoxylin & Eosin, 10x)
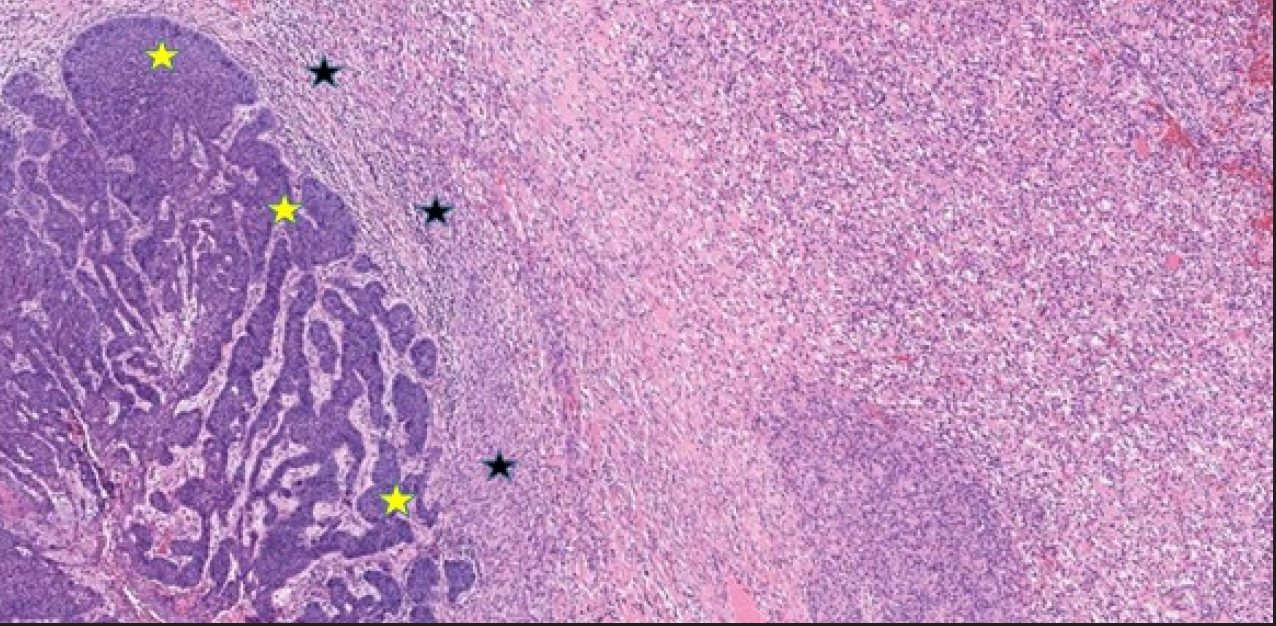
- BCC island within palisading artifact (yellow asterisk) in close contact with a spindle cell tumor in the dermis (black asterisk) (Haematoxylin & Eosin, 40x)
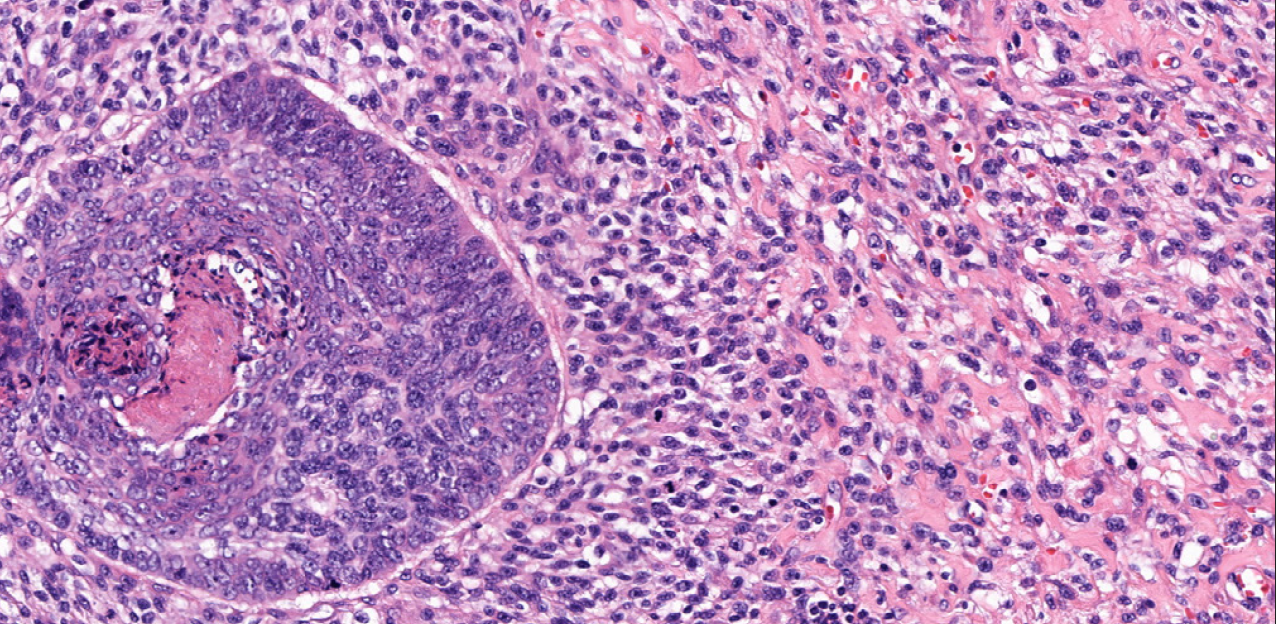
- Details of a combined tumor of a BCC and an AFX (Haematoxylin & Eosin, 200x)
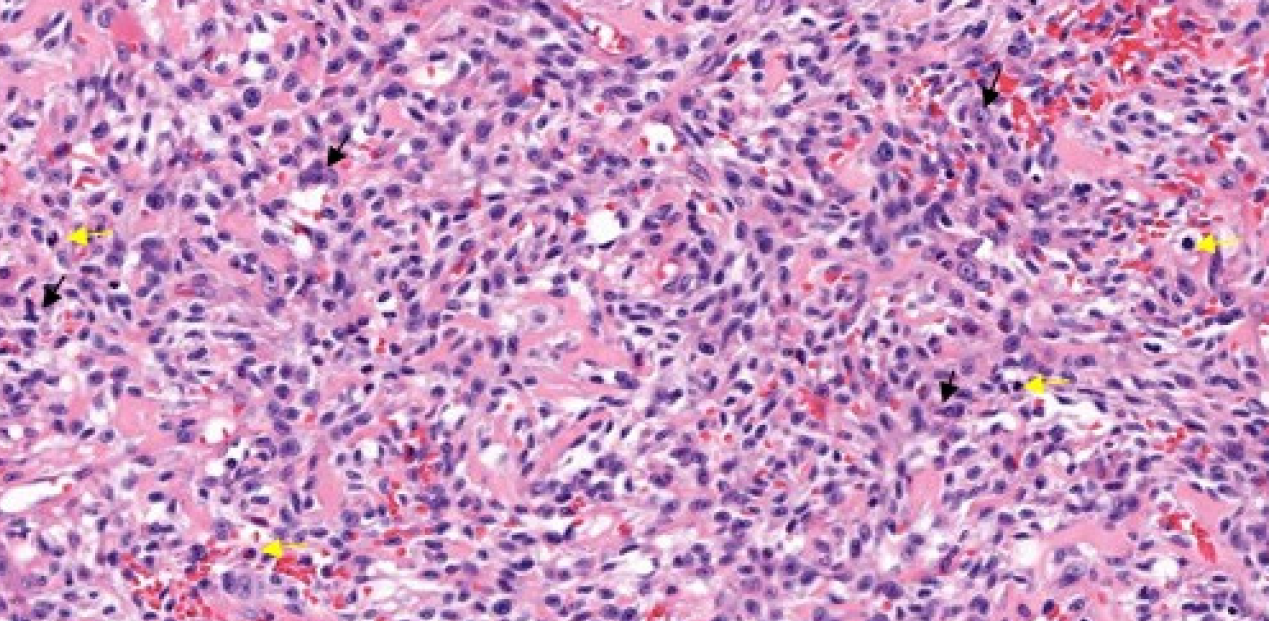
- Dermal proliferation composed of atypical spindle cells with pleomorphic nucleus (black arrows) and frequent atypical mitosis (yellow arrows) (Haematoxylin & Eosin, 200x)
Immunohistochemical stain results were different in both neoplasms [Figure 3]. Vimentin, CD10, CD68, and CD99 were highly positive in the spindle cell tumor and negative in the BCC. Desmin, EMA, S100, and Melan A were negative in both tumors. BCC was positive for Ber EP4 and pancytokeratins AE1-3. Ki67 was highly positive in both neoplasms [Figures 3a–3d]. The final diagnosis was collision tumor of BCC and AFX. After complete excision, no recurrence was observed at one-year follow up.
- Immunohistochemistry (10x). BCC showing positivity for BerEp4.
- Immunohistochemistry (10x). Strong positivity for pancitokeratins AE1-AE3 in BCC.
- Immunohistochemistry (10x). AFX showing strong and diffuse positivity to vimentin.
- Immunohistochemistry (10x). CD10 strongly positive in AFX and negative in BCC.
Collision tumors are composed of two or more different neoplastic proliferations coexisting within the same lesion.6 They represent an infrequent finding in dermatopathology (0.17% of 40,000 biopsies in a retrospective study) and their diagnosis can be challenging.7 Recently, coexisting neoplasms have been classified based on their pathogenesis under the term “multiple skin neoplasm at one site.”8 This concept englobes the categories collision, colonization, combined and biphenotypic tumor defined by Satter et al.9 Although this classification was designed for epithelial and melanocytic neoplasms, it can be useful in our case. Collision tumors have well-defined borders, unlike in our case where the border of both neoplasms is not sharp. Biphenotypic tumors arise from a common stem cell precursor differentiating into different populations. BCC develops from interfollicular epidermal stem cells whereas AFX is mainly thought to arise from mesenchymal lineage although an epithelial origin has also been suggested.10,11 Colonization was defined as a permeation of a melanoma in situ into a BCC. BCC is a slow growing tumor, and it would be unlikely that is able to colonize the underlying faster growing and more aggressive AFX. Therefore, our case could fit into the combined tumor category, where the two populations are intertwined.6,9
AFX is a fibrohistiocytic tumor developing in highly sun-exposed areas and clinically presenting as a rapid growing neoplasia with the possibility of ulceration and bleeding.14 Note that all the previously collision cases described presented ulceration, including ours.3–5 AFX is not usually suspected on clinical presentation and histologic diagnosis is made by exclusion of other proliferations based on immunohistochemistry.14 In our patient we could identify a blue-grey ovoid nest that histologically correlates with the dermal BCC tumor nests.16
In this report, we present the clinical, dermoscopy, and pathological features of a collision of BCC and AFX. It is interesting to describe more of these rarities to extract conclusions about their pathogenesis and different characteristics.
Declaration of patient consent
Patient’s consent not required as the patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Basal cell carcinoma: Epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80:303-17.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical fibroxanthoma: A review of the literature. Dermatologic Surg.. 2011;37:146-57.
- [Google Scholar]
- Basal cell carcinoma and atypical fibroxanthoma: An unusual collision tumor. J Am Acad Dermatol. 2010;63:e74-e76.
- [CrossRef] [PubMed] [Google Scholar]
- A rare collision in dermatopathology: Basal cell carcinoma and atypical fibroxanthoma. Am J Dermatopathol. 2015;37:950-3.
- [CrossRef] [PubMed] [Google Scholar]
- A rare collision of atypical fibroxanthoma and basal cell carcinoma. J Case Rep Images Pathol 2018
- [Google Scholar]
- Collision tumors: A review of their types, pathogenesis, and diagnostic challenges. Dermatol Ther. 2020;33
- [Google Scholar]
- Cutaneous collision tumors: An analysis of 69 cases and review of the literature. Am J Dermatopathol. 1994;16:253-7.
- [PubMed] [Google Scholar]
- Multiple skin neoplasms at one site (Musk in a nest): A comprehensive review of basal cell carcinoma and benign or malignant “collision” tumors at the same cutaneous location. Clin Cosmet Investig Dermatol. 2020;13:731-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tumors composed of malignant epithelial and melanocytic populations: A case series and review of the literature. J Cutan Pathol. 2009;36:211-9.
- [CrossRef] [PubMed] [Google Scholar]
- Adult interfollicular tumour-initiating cells are reprogrammed into an embryonic hair follicle progenitor-like fate during basal cell carcinoma initiation. Nat Cell Biol. 2012;14:1282-94.
- [CrossRef] [PubMed] [Google Scholar]
- Genome-wide methylation profiling and copy number analysis in atypical fibroxanthomas and pleomorphic dermal sarcomas indicate a similar molecular phenotype. Clin Sarcoma Res. 2019;9:2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Malignant Melanoma Within Squamous Cell Carcinoma and Basal Cell Carcinoma. Am J Dermatopathol. 2013;35:226-34.
- [CrossRef] [PubMed] [Google Scholar]
- Collision skin lesions—results of a multicenter study of the International Dermoscopy Society (IDS) Dermatol Pract Concept. 2017;7:51-62.
- [Google Scholar]
- Atypical fibroxanthoma and pleomorphic dermal sarcoma: Updates on classification and management. Dermatol Clin. 2019;37:253-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy features of atypical fibroxanthoma: A multicenter study of the international dermoscopy society. Australas J Dermatol. 2018;59:309-14.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy and dermatopathology correlates of cutaneous neoplasms. J Am Acad Dermatol. 2019;80:341-63.
- [CrossRef] [PubMed] [Google Scholar]





