Translate this page into:
High-frequency ultrasonography for the detection of subclinical arthritis in chronic plaque psoriasis patients – A cross-sectional study
Corresponding author: Dr. Shekhar Neema, Department of Dermatology, Base Hospital, Lucknow, Uttar Pradesh, India. shekharadvait@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vendhan S, Vasudevan B, Rai R, Neema S, Krishnan LP, Kamboj P. High-frequency ultrasonography for the detection of subclinical arthritis in chronic plaque psoriasis patients – A cross-sectional study. Indian J Dermatol Venereol Leprol. 2025;91:16-22. doi: 10.25259/IJDVL_410_2023
Abstract
Background
Psoriatic arthritis (PsA) is seen in almost 30–40% cases of psoriasis. Psoriasis precedes the onset of PsA in 85% of cases. Delay in the diagnosis of PsA may lead to poor functional outcomes and morbidity. Screening psoriasis patients with high-frequency ultrasound helps to diagnose arthritis at an early stage leading to prompt intervention and possible reduction in the morbidity associated with the disease.
Objectives
To determine the role of high frequency ultrasonography (USG) in the detection of subclinical PsA.
Methods
A cross-sectional study was conducted in a dermatology and radiology department of Armed Forces Medical College, Pune between July 2021 and December 2022. Patients of chronic plaque psoriasis with no clinical evidence of arthritis were assessed using high-frequency USG. Various parameters such as bony erosions, synovial thickening, tendon thickening, tendon hypo-echogenicity, calcifications and power doppler signals were assessed.
Results
A total of 117 patients were included in the study. The distal interphalangeal joint (DIP) and Achilles tendon were the most commonly affected sites. Synovial thickening in DIP was observed in 67 (57%) patients and Achilles tendon thickening was observed in 39 (33%) patients.
Limitations of the study
The cross-sectional nature of the study is the major limitation. A longitudinal study will be required to understand the clinical relevance of ultrasonographic changes in these patients. Another limitation of the study is the lack of age and gender-matched controls. Future research should include such controls to ensure more accurate results.
Conclusion
Subclinical arthritis is common in patients with chronic plaque psoriasis. High-frequency ultrasound is a useful tool for detecting subclinical synovitis and enthesitis in asymptomatic patients. The DIP joint and Achilles tendon ultrasound can be used for screening for early detection of PsA.
Keywords
psoriasis
psoriatic arthritis
ultrasonography
Introduction
Psoriasis is a chronic inflammatory skin disorder that affects 2–3% of the global population. It is an immune-mediated disease with a complex interplay of various genetic and environmental factors.1 Co-morbidities such as arthritis, metabolic syndrome, cardiovascular diseases, inflammatory bowel disease and depression are associated with psoriasis.2 Psoriatic arthritis (PsA), an inflammatory arthropathy, affects 10–40 % of people with psoriasis, most frequently in those aged between 30 and 50 years.3 Psoriasis precedes the onset of PsA in about 85% of patients; the symptoms of PsA precede or are present concurrently in the remaining patients.4 There are no biomarkers for the diagnosis of PsA; history, examination and imaging are the cornerstones in the diagnosis of PsA. Classification Criteria for Psoriatic Arthritis (CASPAR) is used as an objective tool for the clinical diagnosis of PsA and to standardise the diagnosis for clinical trials and observational studies.4 Juxta-articular new bone formation in plain radiograph of hands or foot is one of the criteria in CASPAR. The musculoskeletal imaging using ultrasonography (USG) and magnetic resonance imaging (MRI) can detect soft tissue and osseous inflammatory changes.5 USG is a sensitive, non-invasive, cost-effective and readily accessible technique for detecting early and subclinical joint involvement. The key elements of arthritic alterations in USG include hypo-echogenicity, thickened tendon insertions, calcification, enthesophytes and erosions.6 Delays in PsA diagnosis have been linked to poor long-term radiological and functional outcomes.7 Advances in imaging techniques have made it possible to detect joint involvement early, assisting in early diagnosis and prompt intervention, reducing disease progression and long-term morbidity.8 The objective of this cross-sectional study is to determine the role of USG in detecting subclinical PsA.
Methodology
It was a cross-sectional study, conducted in the Dermatology and Radiology Department of Armed Forces Medical College, Pune during the study period 01 Jul 21–31 Dec 2022. The study was approved by the Institutional Ethical Committee. Adult patients with chronic plaque psoriasis were assessed for inclusion in the study. All patients were assessed for the presence of PsA by history, clinical examination and early psoriatic arthritis screening questionnaire (EARP). Patients without any clinical evidence of arthritis, enthesitis and EARP score less than 3 were included in the study. The exclusion criteria for the study included systemic treatment in the last 6 months, arthritis, enthesitis and dactylitis on clinical examination or a cut-off value of more than 3 on EARP. Pregnant and lactating women, patients with concomitant rheumatologic disorder, trauma or surgery of joints being scanned were also exclusion criteria for the study.
Data collection
Clinical and epidemiologic details, including age, sex, duration of illness, dermatology life quality index (DLQI) and psoriasis area severity index (PASI), were recorded. Plain radiograph of hands was performed in all the cases.
Ultrasound parameters
High-frequency USG of five joints and five entheses was performed by a radiologist trained in musculoskeletal imaging. Joints included the distal interphalangeal joint (DIP), proximal interphalangeal joint (PIP) and metacarpo-phalangeal joint (MCP) of the left third digit, left wrist and left knee joint. Entheses included the flexor tendon of the third left digit, extensor tendons at left wrist, common extensor tendon at the elbow, left quadriceps tendon, left Achilles tendon and left Achilles bursa. Ultrasonographic assessment of the joints and enthesis was done using a wide band linear array transducer with frequency ranging from 5 to 13 MHz on a “GE LOGIQ e” portable ultrasound machine. All the joints and enthesis were scanned in axial and longitudinal planes.
-
1.
The joint parameters measured were bone erosions, synovial thickening and power doppler (PD) signals.
-
a.
Bony erosion is defined by a cortical break with a stepdown contour defect, seen in two perpendicular planes, at the insertion of the enthesis to the bone.
-
b.
Joint synovial thickening is assessed as grade 0 (<0.5 mm), grade 1 (0.5–2 mm), grade 2 (2–4 mm) and grade 3 as >4 mm.
-
c.
Joint PD signal is classified as grade 0 (no intra-articular colour signals), grade 1 (≤3 colour signals), grade 2 (<50% of the intra-articular area filled with colour signals), grade 3 (>50% of the intra-articular area filled with colour signals).
-
2.
Enthesis parameters measured were tendon thickening, echogenicity, calcification, enthesophytes and PD signals. Tendon thickening is graded as grade 1 – normal tendon with parallel margins and homogenous echotexture, grade 2 – thickened, bowed margin tendon with homogenous echotexture and grade 3 – tendon with discrete hypoechoic areas with or without tendon thickening.
Sample size calculation and statistical analysis: Based on an original study conducted by De Simone C et al.9 on the usefulness of ultrasound imaging in detecting PsA of fingers and toes in patients with psoriasis, after applying the population correction factor (15 cases per month), the corrected sample size for our study is calculated as 117 with 95% confidence interval. The data were compiled in Microsoft excel sheet and statistical analysis was performed using statistical package for social sciences (SPSS version 20, Chicago). Categorical data are presented as number with percentage and continuous data as mean with standard deviation. Quantitative data were compared using independent t-test and categorical data using chi-square test. All statistical tests were two-sided and were performed at a significance level of α = 0.05.
Results
A total of 186 patients were assessed for inclusion during the study period. Sixty-nine (37%) patients were excluded (32 – PsA or EARP more than 3, 21 – systemic treatment, 16 – did not consent) and 117 patients were included in the study. A total of 585 joints and 585 entheses were assessed among these patients. The study group consisted of 90 (77%) males and 27 (23%) females with the mean age being 43 (±12) years. The mean PASI and DLQI score were 9.53 +/- 4.4 S.D and 8.3 +/- 2.8 S.D respectively. Out of 117 patients with no clinical evidence of arthritis or enthesitis and normal plain radiographs, ultrasound detected joint involvement in 67 (57%) patients and enthesis involvement in 39 (33%) patients. The most common joint involved in our study was the DIP joint with bony erosions seen in 35 (30%), synovial thickening in 67 (57%) and PD signals in 58 (50%) patients [Figure 1a-b]. The PIP joint was the second most commonly involved joint with bony erosions in 11 (9%), synovial thickening in 39 (33%) and PD signals in 26 (22%) patients [Figure 2a-b]. The MIP joint showed bony erosions in 9 (8%) and synovial thickening in 23 (20%) patients [Figure 3a-b]. The rest of the joint involvement is tabulated in Table 1.
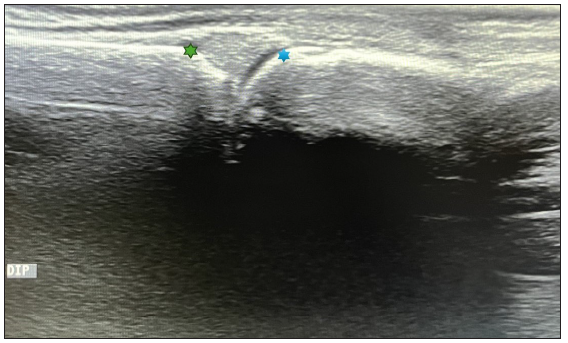
- Longitudinal ultrasound image at the normal distal interphalangeal joint (Green star – middle phalynx distal end; blue star – base of the distal phalynx).
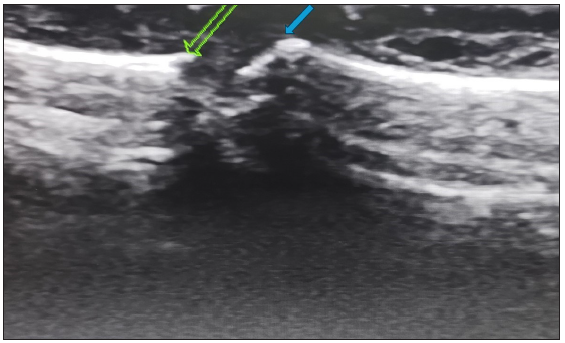
- Longitudinal ultrasound image at the distal interphalangeal joint showing erosions affecting the articular surface, bone loss and irregularity (Green arrow – middle phalynx distal end; blue arrow – base of the distal phalynx).
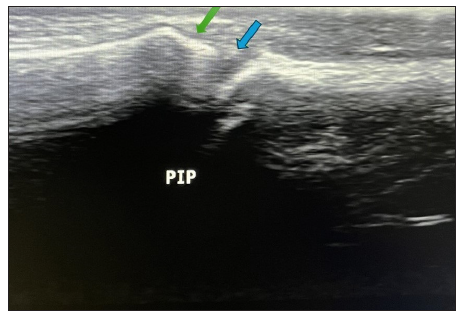
- Longitudinal ultrasound image at the normal proximal interphalangeal joint (Green arrow – middle phalynx distal end; blue arrow – base of the distal phalynx).

- Longitudinal ultrasound image through a proximal interphalangeal joint (marked by yellow square) showing characteristic synovial thickening (yellow star – head of the proximal phalynx; red star – base of the middle phalynx).

- Longitudinal ultrasound image at the normal metacarpophalangeal joint (Green arrow – metacarpal head; blue arrow – base of the phalanx).

- Longitudinal ultrasound image through an affected metacarpophalangeal joint (marked by yellow square) showing synovial thickening with increased doppler signals (yellow star – metacarpal head; red star – base of the phalanx).
| Bony erosions | Synovial thickening | ower doppler signals | ||||||
|---|---|---|---|---|---|---|---|---|
| G0 | G1 | G0 | G1 | G2 | G0 | G1 | G2 | |
| DIP | 82 (70.1%) | 35 (29.9%) | 50 (42.7%) | 60 (52.2%) | 7 (6%) | 59 (50.5%) | 57 (48.7%) | 1 (0.9%) |
| PIP | 106 (90.6%) | 11 (9.4%) | 78 (66.7%) | 34 (29.1%) | 05 (4.3%) | 91 (77.8%) | 26 (22.2%) | 0 |
| MCP | 108 (92.3%) | 09 (7.7%) | 94 (80.3%) | 21 (17.9%) | 2 (1.7%) | 98 (83.8%) | 19 (16.2%) | 0 |
| Wrist | 116 (99.1%) | 01 (0.9%) | 99 (84.6%) | 17 (14.5%) | 1 (0.9%) | 101 (86.3%) | 14 (12%) | 2 (1.7%) |
| Knee | 115 (98.3%) | 02 (1.7%) | 90 (76.9%) | 27 (23.1%) | 0 | 95 (81.2%) | 21 (17.9%) | 1 (0.9%) |
G0: Grade 1, G1: Grade 1, G2: Grade 2, DIP joint: Distal interphalangeal joint, PIP joint: Proximal interphalangeal joint, MCP joint: Metacarpophalangeal joint.
Achilles tendon thickening was the most common enthesis involved, with tendon thickening in 39 (33%), bony erosions at the site of attachment in 7 (6%), calcifications in 12 (10%) and tendon PD signals in 18 (15%) patients [Figures 4a-b and 5]. The tendon thickening of the quadriceps tendon, common extensor tendon of the elbow [Figure 6a-b], extensor tendons of the wrist and flexor tendon of the digit was observed in 5 (6%), 2 (1.7%),10 (8.5%) and 7 (6%) patients, respectively [Table 2]. DIP joint and Achilles tendon were more commonly involved than other joints and enthesis, respectively. The difference was statistically significant (p = 0.001) [Table 3]. The plain radiographs of hands of all the patients were normal.
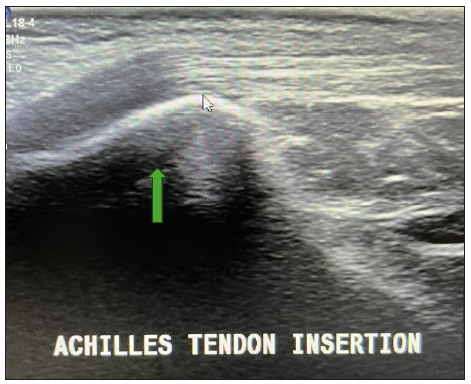
- Longitudinal ultrasound image at the insertion of the normal tendo-achilles (marked by green arrow).

- Longitudinal ultrasound image at the insertion site of the affected tendo-achilles (marked by yellow square). The image shows thickening and complete loss of the fibrillary pattern of the tendon. Increased doppler signal is seen along the tendon and the peritendinous tissue (yellow star – calcaneum; green arrow – tendo-achilles).

- Axial image through the tendon (marked by upward yellow arrow) shows fluid around the tendon (marked by downward yellow arrow).
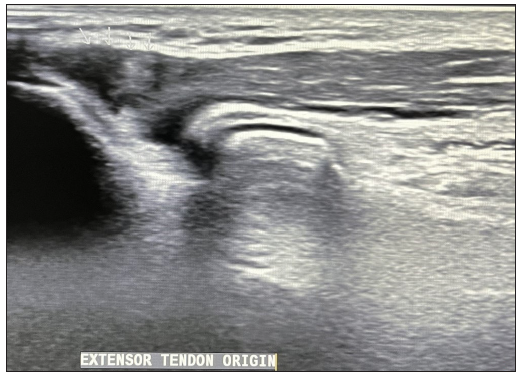
- Longitudinal ultrasound image at the normal extensor tendon at elbow.

- Longitudinal ultrasound image at the elbow joint (marked by yellow square) shows affliction of the common extensor tendon with loss of fibrillary pattern and increased doppler signals (Green star – lateral epicondyle; yellow star – tendon).
| Tendon thickening | Hypo-echogenicity | Power doppler signals | |||||
|---|---|---|---|---|---|---|---|
| G0 | G1 | G2 | G0 | G1 | G0 | G1 | |
| FTD | 110 (94.0%) | 07 (6%) | 0 | 115 (98.3%) | 02 (1.7%) | 115 (98.3%) | 2 (1.7%) |
| CETW | 107 (91.5%) | 10 (8.5%) | 0 | 116 (99.1%) | 01 (0.9%) | 114 (97.4%) | 3 (2.6%) |
| CETE | 115 (98.3%) | 02 (1.7%) | 0 | 116 (99.1%) | 01 (0.9%) | 116 (99.1%) | 01 (0.9%) |
| QT | 111 (94.9%) | 06 (5.1%) | 0 | 115 (98.3%) | 02 (1.7%) | 116 (99.1%) | 01 (0.9%) |
| AT | 77 (65.8%) | 39 (33.3%) | 01(0.9%) | 110 (94%) | 07 (6%) | 116 (99.1%) | 01 (0.9%) |
G0: Grade 1, G1: Grade 1, G2: Grade 2, FTD: Flexor tendon of the digit, CETW: Compartment of extensors tendons wrist, CETE: Common extensor tendon of elbow, QT: Quadriceps tendon, AT: Achilles tendon.
| DIP | PIP | P value | |
|---|---|---|---|
| Bony erosions | 35 (30%) | 11 (9%) | 0.001 |
| Synovial thickening | 67 (58%) | 39 (33%) | 0.001 |
| Power doppler | 58 (50%) | 26 (22%) | 0.001 |
| A | CETW | ||
| Tendon thickening | 40 (34%) | 10 (8.5%) | 0.001 |
DIP: distal interphalangeal joint, PIP: proximal interphalangeal joint, AT: Achilles tendon, CETW: common extensor tendon of the wrist.
Discussion
PsA is an inflammatory arthritis, which develops in 30–40% of psoriasis patients during their lifetime. Severe psoriasis, nail involvement, obesity, low education level and uveitis are considered predictive for the development of PsA.10 However, there are no biomarkers to predict development of the disease and early diagnosis is the only way to prevent morbidity associated with PsA. Five clinical subgroups of PsA were defined by Moll and Wright, demonstrating the disease heterogeneity. The subtypes were asymmetric oligo-arthritis (affecting four or less joints), polyarthritis (affects five or more joints), DIP predominant disease, spondyloarthropathy and arthritis mutilans. Asymmetric oligo-arthritis is the commonest while arthritis mutilans is most uncommon subtype of PsA.11 Enthesitis is seen in 30–50% of patients. It typically affects the plantar fascia and Achilles tendon, but it can also involve the patella, iliac crest, epicondyles and supraspinatus insertions. Dactylitis is observed in 40–50% of patients; it most frequently affects the third and fourth toes but also involves the fingers. Dactylitis can be acute (characterised by pain, swelling and skin redness) or persistent (swelling without inflammation). Dactylitis is frequently related to a severe illness marked by polyarthritis, bone erosive changes and new bone growth.12 Imaging is crucial for patients being screened for PsA. It is associated with bone erosion and new bone formation. Erosions occur early in the disease and studies found erosion in 27% of patients within 5 months and 50% of patients within 1 year of disease onset.13
Patients with asymptomatic disease benefit from ultrasound to identify subclinical joint inflammation.14 De Simone C et al. found that USG was useful in detecting joint and/or tendon abnormalities in the fingers and toes of patients with suspicious changes.9 According to Wiell and colleagues, clinical examination and x-ray are less sensitive to inflammatory and destructive changes than ultrasound and demonstrated strong inter-observer agreement for bone changes but poorer inter-observer agreement for inflammatory changes.15 Ultrasound typically reveals synovitis, enthesitis and tenosynovitis which are not typically seen on radiographs. Entheseal abnormalities were found in 33% of individuals who underwent USG examination in a study by De Fillipis et al. on clinically asymptomatic psoriasis patients.16 In our study too we noticed Achilles tendon thickening in 39 (33%) patients. Musculoskeletal ultrasound can also detect cortical abnormalities on the osteal surface and osteoproliferation but not intraosseous structures. PD or colour flow identifies vascularity in soft tissues without the need for contrast and suggest inflammation.17 A novel composite targeted PD scoring method that takes into account the joint, tendon, enthesis, skin and nail was reported by Gutierrez et al. In this study, USG was performed at baseline and 8 weeks in the locations with the highest baseline doppler signal on 16 patients with PsA receiving anti-TNF medication. The mean overall score improved across the board from the first baseline to the eighth week.18 The assessment of joints, tendons and entheses in the fingers and toes of PsA patients can be much enhanced by ultrasound.19 Our study demonstrated that high-frequency ultrasound can diagnose subclinical arthritis despite normal radiographs of the hand.
Another study by Pistone et al. demonstrated that USG is a sensitive technique that detects enthesitis more frequently than clinical examination in patients with psoriasis. They proposed the use of Achilles tendon USG in the early diagnosis of psoriatic arthropathy with the intention of limiting pathological progression.20 In our study, we found that the Achilles tendon is the most common enthesis involved in psoriasis followed by the common extensor tendon of the elbow, flexor tendon of the digit and quadriceps tendon.
Acquacalda E. et al. detected a high prevalence of ultrasonic enthesitis in psoriasis patients with or without musculoskeletal symptoms needing systemic treatment and discovered that at 6 months, USG morphological abnormalities were likely to improve with treatment.21
The DIP was the most common joint and the Achilles tendon was the most common tendon found involved in our study. DIP and Achilles tendon can be used for screening psoriasis patients for subclinical arthritis and enthesitis. PsA can result in permanent joint damage; therefore, early detection and treatment are crucial for improving long-term patient outcomes. More specifically, peripheral joint erosions and poor functional results are caused by diagnostic and therapeutic delays of more than 6 months. Early detection of PsA and the use of targeted medicines can greatly alleviate the signs and symptoms and stop radiographic progression.22 From the previous studies and from our results, it can be inferred that high-frequency ultrasound can diagnose arthritis at an early stage, even in psoriasis patients who do not have clinically obvious joint symptoms.
Limitations of the study
The cross-sectional nature of the study is a limitation, A longitudinal follow-up study will be required to understand the clinical relevance of ultrasonographic changes in these patients. The study has used EARP score more than 3 as an exclusion criterion. The screening criteria though sensitive do not pick up 100% of cases of PsA. Another exclusion criterion is no systemic treatment in the last 6 months; however, the disease can rarely have longer remission periods. It is possible that a few cases of existing PsA were included in the study inadvertently, resulting in bias. Another limitation of the study is the lack of age and gender-matched controls.
Conclusion
The majority of PsA patients have skin lesions before they develop joint involvement. At present, there are no biomarkers that can precisely predict which psoriasis patients will later develop PsA, even though they are actively being developed. The onset of inflammatory arthritis in a psoriasis patient can take many years. As a result, dermatology and primary care professionals should be well prepared to identify PsA in their at-risk psoriasis patients. A positive long-term clinical outcome for these patients depends on the physician’s ability to detect PsA early and start treatment before irreversible joint damage occurs. Our study concludes that high-frequency ultrasound is a reliable investigation for early diagnosis of PsA in a known case of psoriasis.
Ethics committee approval
The study was approved by the Institutional Ethical Committee number PG/2020/1/3 dated 20.12.2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Etiology and Pathogenesis of Psoriasis. Rheum Dis Clin North Am. 2015;41:665-75.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis: Which therapy for which patient: Psoriasis comorbidities and preferred systemic agents. J Am Acad Dermatol. 2019;80:27-40.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriatic arthritis and psoriasis: Differential diagnosis. Clin Rheumatol. 2016;35:1893-901.
- [CrossRef] [PubMed] [Google Scholar]
- The pathogenesis of psoriatic arthritis. Lancet. 2018;391:2273-84.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound assessment of elbow enthesitis in patients with seronegative arthropathies. J Ultrasound. 2014;17:33-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Role of diagnostic ultrasound in the assessment of musculoskeletal diseases. Ther Adv Musculoskelet Dis. 2012;4:341-55.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Improvements in diagnostic tools for early detection of psoriatic arthritis. Expert Rev Clin Immunol. 2016;12:1209-15.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic delay of more than 6 months contributes to poor radiographic and functional outcome in psoriatic arthritis. Ann Rheum Dis. 2015;74:1045-50.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of ultrasound imaging in detecting psoriatic arthritis of fingers and toes in patients with psoriasis. Clin Dev Immunol. 2011;2011:390726.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The incidence and risk factors for psoriatic arthritis in patients with psoriasis: A prospective cohort study. Arthritis Rheumatol. 2016;68:915-23.
- [CrossRef] [PubMed] [Google Scholar]
- Oligoarticular psoriatic arthritis: Addressing clinical challenges in an intriguing phenotype. Rheumatol Ther. 2018;5:311-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Psoriatic arthritis: What is happening at the joint? Rheumatol Ther. 2019;6:305-15.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A prospective, clinical and radiological study of early psoriatic arthritis: an early synovitis clinic experience. Rheumatology (Oxford). 2003;42:1460-8.
- [CrossRef] [PubMed] [Google Scholar]
- From psoriasis to psoriatic arthritis: insights from imaging on the transition to psoriatic arthritis and implications for arthritis prevention. Curr Rheumatol Rep. 2020;22:24.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ultrasonography, magnetic resonance imaging, radiography, and clinical assessment of inflammatory and destructive changes in fingers and toes of patients with psoriatic arthritis. Arthritis Res Ther. 2007;9:R119.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ultrasonography in the early diagnosis of psoriasis-associated enthesopathy. Int J Tissue React. 2005;27:159-62.
- [PubMed] [Google Scholar]
- Psoriatic dactylitis: Koebner phenomenon of the pulleys-comment on “Ultrasound assessment in psoriatic arthritis (Psoriatic arthritis) and psoriasis vulgaris (non-Psoriatic arthritis): which sites are most commonly involved and what features are more important in Psoriatic arthritis?”. Quant Imaging Med Surg. 2021;11:4687-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A sonographic spectrum of psoriatic arthritis: “The five targets”. Clin Rheumatol. 2010;29:133-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ultrasound and doppler US in evaluation of superficial soft-tissue lesions. J Clin Imaging Sci. 2014;4:12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Achilles tendon ultrasonography may detect early features of psoriatic arthropathy in patients with cutaneous psoriasis. Br J Dermatol. 2014;171:1220-2.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound study of entheses in psoriasis patients with or without musculoskeletal symptoms: A prospective study. Joint Bone Spine. 2015;82:267-71.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and ultrasonographic predictors for achieving minimal disease activity in patients with psoriatic arthritis: the UPSTREAM (Ultrasound in PSoriatic arthritis TREAtMent) prospective observational study protocol. BMJ Open. 2018;8:e021942.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






