Translate this page into:
Efficacy and safety of weekend cyclosporine treatment as maintenance therapy for preventing frequent disease exacerbations in moderate to severe chronic plaque psoriasis patients – A retrospective cohort study
-
Received: ,
Accepted: ,
How to cite this article: Dogra S, Kumar S, Narang T, Mehta H, Hanumanthu V, Handa S. Efficacy and safety of weekend cyclosporine treatment as maintenance therapy for preventing frequent disease exacerbations in moderate to severe chronic plaque psoriasis patients - A retrospective cohort study. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1089_2023
Abstract
Background
Psoriasis is a chronic, inflammatory, systemic disease with predominant manifestations in the skin and joints impairing patient’s quality of life. A proportion of patients have frequent severe disease exacerbations requiring repeated systemic treatments. There is a scarcity of literature evaluating the role of systemic maintenance therapy in psoriasis patients in preventing such frequent disease flares.
Objective
To evaluate the efficacy and safety of weekend cyclosporine treatment (WCT) as maintenance therapy in moderate to severe chronic plaque psoriasis patients for the prevention of frequent disease exacerbations.
Methods
In this retrospective cohort study, 22 psoriasis patients with a history of frequent disease exacerbations (≥ 3 in the last 1 year) who were administered WCT (group A) were compared with the same number of matched patients (age and gender) not on WCT or any systemic maintenance therapy (group B).
Results
Four patients (18.2%) in group A had disease exacerbations which was significantly lower (p = 0.00, Fisher’s exact test) as compared to 21 patients (95.5%) in group B during the study period. Also, patients in group A had significantly lower number of overall exacerbations [mean ± SD: 0.23 ± 0.53 vs 2.95 ± 1.43) p = 0.00, Mann–Whitney U test] as compared to group B. Four (9.1%) patients in group A encountered adverse effects (acneiform eruptions – two, mild gingival hyperplasia – one, myalgia – one) as compared to three (acneiform eruptions – two, headache – one) in group B (p = 1.00).
Conclusion
WCT significantly reduced the number of disease exacerbations and is a safe and effective mode of maintenance therapy in such subset of psoriasis patients.
Keywords
Weekend cyclosporine therapy
cyclosporine
psoriasis
maintenance therapy for psoriasis
Introduction
Psoriasis is a chronic inflammatory condition with predominant manifestations in skin and joints. The clinical course of psoriasis is unpredictable and a proportion of patients suffer from frequent disease exacerbations. Although several established treatment modalities are available for inducing remission in psoriasis patients, there is paucity of literature in evaluating the safety and efficacy of various interventions for maintaining remission and preventing frequent disease exacerbations. Oral cyclosporine (CYC) is one of the most widely used therapies for inducing rapid remission in patients with moderate to severe psoriasis.1,2 Different regimens of CYC have been tried for inducing and maintaining remission of psoriasis.3,4 However, long-term continuous oral CYC therapy may be associated with several adverse effects including risk of nephrotoxicity, warranting its discontinuation after attaining remission.5 Disease exacerbation is common in psoriasis patients on discontinuing CYC or other systemic treatments which is frustrating for both clinicians and patients. Some strategies and regimens using weekend CYC therapy for the maintenance of remission in moderate to severe chronic plaque psoriasis have been tried previously. Weekend cyclosporine therapy (WCT) involves administration of CYC on two consecutive days per week as a maintenance therapy in psoriasis. Fernandes et al. found it to be comparable in efficacy to continuous CYC therapy in preventing exacerbations in psoriasis patients.6 Colombo et al. found that time to relapse was prolonged in psoriasis patients receiving WCT as compared to placebo.5 Both the above studies included patients of chronic plaque psoriasis but did not mention the frequency of exacerbations in the included patients prior to the initiation of CYC. In clinical practice, there are certain psoriasis patients who have a tendency of frequent exacerbations where the use of WCT may be justified as maintenance therapy. In this retrospective study, we analysed the safety and efficacy of WCT as a maintenance therapy for preventing exacerbations in a subset of chronic plaque psoriasis patients having moderate to severe disease who had a history of frequent disease flares in the recent past.
Materials and Methods
Study setting
This retrospective study was carried out at the psoriasis clinic of our centre. The clinical and demographic records including the severity scores, treatment plans, adverse effects and investigations of the patients attending our psoriasis clinic at each visit were maintained and updated both in the outpatient cards retained by the patient and psoriasis clinic files stored in the hospital records. Daily CYC at a dose of 3–5 mg/kg/day is one of the most commonly used systemic agents for the control of disease activity in patients with moderate to severe psoriasis at our clinic with usually good clinical response (PASI-90 or PASI ≥ 75) in terms of achievement of disease control in the majority of patients. After attaining good clinical response, the daily CYC was usually tapered in the next 6–10 weeks (reduction of around 1 mg daily dose every other week) and stopped. Out of the subset of patients who achieved good clinical response (Ninety percent reduction psoriasis area and severity index (PASI-90) or more with daily CYC, few of the willing patients especially those with a history of frequent disease exacerbations (three or more exacerbations in 1 year) were maintained on WCT (CYC at a dose of 3–5 mg/kg/day administered only on two consecutive days in a week), while some of the patients were managed without any systemic agents.
Any patient on WCT or without any systemic agent as maintenance therapy experiencing disease exacerbations was usually restarted on daily CYC to induce clinical remission (≥ PASI-90) followed by tapering as described above. The choice of CYC as the systemic agent to manage the exacerbations in these patients was based on the previous history of response to daily CYC. Patients on daily CYC or WCT were followed up regularly (every 2 weeks for the first 4 weeks and every 4 weeks thereafter).
Data collection
Clinical records (psoriasis clinic files) of patients with moderate to severe psoriasis who were enrolled in the psoriasis clinic from January 2014 to December 2022 were screened. After screening a large number of patients, those satisfying the inclusion and exclusion criteria of both groups were included after careful matching [Figure 1]. The demographic and clinical details of the included patients were retrospectively reviewed and entered into a pre-designed clinical proforma followed by statistical analysis of data.
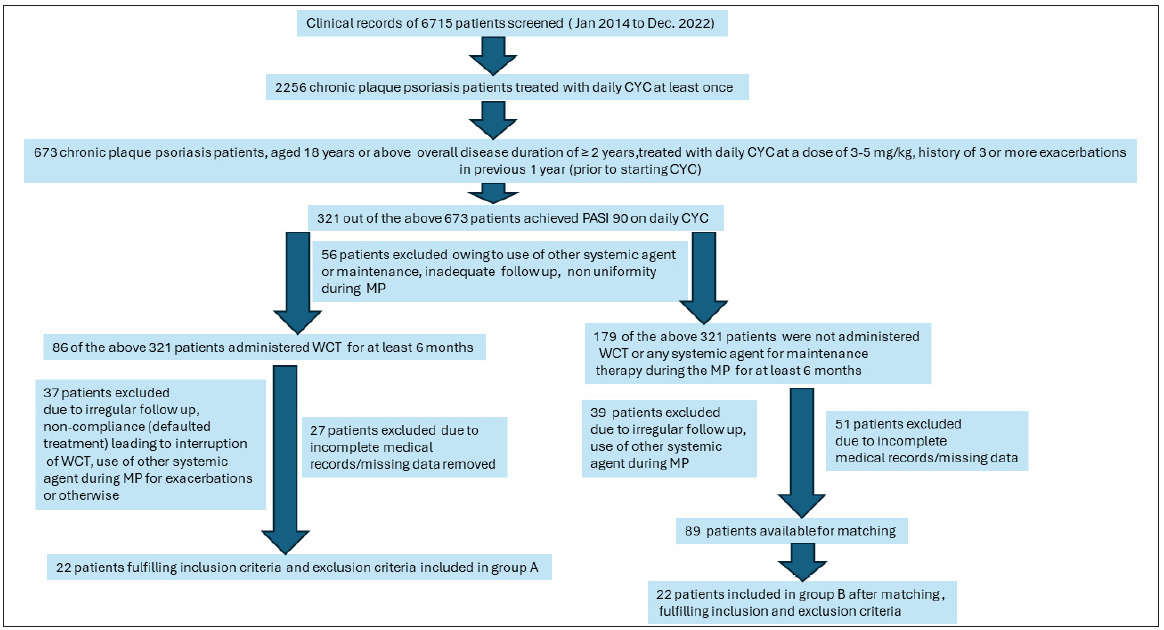
- The flow diagram depicting the screening and inclusion of patients based on inclusion and exclusion criteria. WCT: Weekend cyclosporine treatment, CYC: Oral Cyclosporine, PASI: Psoriasis Area and Severity Index, MP: maintenance phase.
Inclusion criteria
Chronic plaque psoriasis patients aged 18 years or above, with an overall disease duration of ≥ 2 years, treated with daily CYC, with a history of three or more exacerbations (characterised by PASI ≥ 10 or Body surface area (BSA) ≥ 10 during exacerbations) in the previous 1 year (prior to starting CYC) were screened for inclusion in the study. After meticulous screening, patients who were treated with daily CYC at a dose of 3–5 mg/kg/day (induction phase – IP) and achieved clinical remission (≥ PASI 90), followed by tapering and cessation of daily CYC and continuation of WCT for at least 6 months (maintenance phase – MP) were included in group A. In group B, patients who achieved clinical remission (PASI ≥ 90) on daily CYC (IP), after which it was tapered and stopped but were not started on WCT or any systemic agent for maintenance (MP) were included. Subjects in both groups were matched with respect to age (± 5 years but ≥ 18 years), gender, and duration of MP. The exacerbations during the MP in both the groups were managed by switching to daily CYC (3–5 mg/kg/day which was tapered and stopped after achieving PASI ≥ 90). Topical therapy and antihistamines if required were allowed in both the groups during the IP and MP.
Exclusion criteria
Patients who were treated with any other systemic agents other than daily CYC during the MP for exacerbations were excluded from the study. Group A or group B patients in whom there was any non-uniformity of MP ( non-compliance, irregular follow-ups, incomplete medical records or missing data, use of other systemic therapies) during the study period were also excluded from the study or the duration was adjusted to maintain the uniformity (e.g., for any group B patient who was not on any systemic treatment for 15 months but was later started on WCT to avoid frequent exacerbations, the maintenance phase duration was calculated as 15 months only). Thus, it was ensured that patients in both the groups either received WCT (group A) or no systemic therapies (group B) during the MP except during the exacerbations when they received daily CYC.
Study duration and follow-up
The MP in both the groups was defined as the study duration when the outcome parameters were assessed. The duration of MP in both the groups was ≥ 6 months. Blood pressure readings, renal and liver function tests, lipid profile, and complete blood count were conducted at baseline and at follow-up visits for each patient in both groups.
Outcome parameters
The outcome parameter was the number of psoriasis patients having disease exacerbations and the total number of exacerbations during MP. Exacerbations were defined as PASI ≥ 10 or involved body surface area (BSA) of 10 % during the MP. All the patients were monitored for adverse effects including nephrotoxicity and hypertension as per the standard protocol at each follow-up visit.
Statistical analysis
Descriptive quantitative data were presented as mean ± standard deviations (SD). Qualitative or categorical data were described as frequencies and proportions. Qualitative data were compared between the two treatment groups using Pearson’s Chi-square test or Fisher’s exact test. The normality of the quantitative data was assessed by the Kolmogorov–Smirnov test. Quantitative data were compared using an unpaired t-test for normally distributed data and Mann–Whitney test for skewed data. P value < 0.05 was considered as significant in all the tests. Statistical analysis was carried out using Statistical Package for Social Sciences (SPSS for Windows, version 28, IBM, New York, USA).
Results
Twenty-two patients each fulfilling the inclusion and exclusion criteria were recruited in both the study groups. The flow diagram depicting the screening and inclusion of patients based on inclusion and exclusion criteria has been illustrated in Figure 1. The mean duration of MP was the same (11.64 ± 3.13 months) in both the groups due to matching at the time of inclusion. The baseline (both matched and unmatched) clinico-demographic characteristics including age, gender, weight of patients, duration of disease at the time of inclusion, the severity at the beginning of MP (PASI and BSA), and number of exacerbations in the past one year (prior to IP) of group A and group B were comparable and are illustrated in Table 1.
| Baseline clinico-demographic characteristics | Group A | Group B | P value |
|---|---|---|---|
| Age (years) | 34.1 ± 9.7 | 35.0 ± 10.2 | 0.76 (unpaired t-test) |
| Gender (M:F) | 12:10 | 12:10 | 1 (chi square test) |
| Weight (kg) | 66.9 ± 7.6 | 68.7 ± 5.4 | 0.36 (unpaired t- test) |
| Duration of disease in months | 50.8 ± 12.4 | 54.8 ± 11.8 | 0.27 (unpaired t- test) |
| Body surface area (baseline) | 1.86 ± 0.93 | 1.70 ± 0.98 | 0.58 (unpaired t- test) |
| Baseline PASI | 2.66 ± 1.22 | 2.51 ± 1.26 | 0.69 (unpaired t-test) |
|
Number of exacerbations in the past 1 year prior to IP Mean ± SD Range |
3.41 ± 0.59 (3-5) |
3.36 ± 0.49 (3-5) |
0.93 (Mann–Whitney test) |
| Duration of MP (months) |
11.64 ± 3.13 Range (6–18 months) |
11.64 ± 3.13 Range (6–18 months) |
1 (unpaired t-test) |
PASI: Psoriasis Area and Severity Index, IP: Induction Phase, SD: Standard Deviation
On comparing the outcome parameters in the two groups [Table 2], four (18.2%) patients receiving WCT had exacerbations during MP which was significantly lower (p = 0.00, Fisher’s exact test) as compared to 21 patients (95.5%) in the group not receiving WCT. Out of four patients in group A having exacerbations in MP, three patients had only one exacerbation while one patient had two exacerbations [Table 2]. None of the group A patients had more than two exacerbations. Out of the 21 patients in group B having exacerbations, the number of patients according to number of exacerbations [Table 2] were seven (three exacerbations), five (two exacerbations), four (four exacerbations), two (five exacerbations), two (one exacerbation) and one (six exacerbations).
| Outcome parameters | Group A | Group B | P value |
|---|---|---|---|
| Number of patients having exacerbations during MP | 4 (18.2%) | 21 (95.5%) | 0.00 (Fisher’sexact test) |
| Comparison of the number of patients according to the number of exacerbations in MP in both groups | |||
| 0 exacerbation | 18 (81.8%) | 1 (4.5%) | <0.001 (chi-square test) |
| 1 exacerbation | 3 (13.6%) | 2 (9.1%) | |
| 2 exacerbations | 1 (4.5%) | 5 (22.7%) | |
| 3 exacerbations | 0 | 7 (31.8%) | |
| 4 exacerbations | 0 | 4 (18.2%) | |
| 5 exacerbations | 0 | 2 (9.1%) | |
| 6 exacerbations | 0 | 1 (4.5%) | |
|
Body surface area at the end of MP ( mean ± SD) |
1.98 ± 1.52 | 4.07 ± 2.10 | 0.00 (unpaired t-test) |
|
PASI at the end of MP ( mean ± SD) |
2.93 ± 2.14 | 5.41 ± 2.40 | 0.00 (unpaired t-test) |
|
Total number of exacerbations during MP Mean ± SD (Range) |
0.23 ± 0.53 (0-2) |
2.95 ± 1.43 (0-6) |
0.00 (Mann–Whitney test) |
| Adverse effects | 2 (9.1 %) (acneiform eruptions – 1, gingival hyperplasia – 1) | 0 (0 %) | 0.49 (Fisher’s exact test) |
MP: Maintenance phase, SD: Standard Deviation
The number of exacerbations during MP (mean ± SD: 0.23 ± 0.53 vs 2.95 ± 1.43) was significantly lower (P = 0.00, Mann–Whitney U test) in group A as compared to group B.
The BSA involved (4.07 ± 2.10 vs 1.98 ± 1.52, p = 0.00, unpaired t-test) and PASI (5.41 ± 2.40 vs 2.93 ± 2.14, p = 0.00, unpaired t-test) at the end of MP were found to be significantly higher in group B as compared to group A.
Four (9.1%) patients in the WCT group encountered adverse effects (acneiform eruptions – two, mild gingival hyperplasia – one, myalgia – one) during MP as compared to three (acneiform eruptions – two, headache – one) in another group (p = 1.00, Fisher’s exact test). None of the patients in both the groups experienced serious adverse effects like nephrotoxicity and severe hypertension during the MP requiring cessation of therapy.
Discussion
Psoriasis is an inflammatory cutaneous disorder marked by chronic, unpredictable course and frequent systemic manifestations like arthritis and metabolic syndrome. The management of psoriasis is aimed at controlling disease activity, prevention of systemic inflammation and comorbidities and improving the quality of life.7, 8 Long-term use of systemic modalities like methotrexate, acitretin and CYC is often required in patients with moderate to severe psoriasis for controlling disease activity and exacerbations.9 There has been a paradigm shift in the management of psoriasis after the advent of newer treatment modalities like biologics. However, owing to financial constraints, the use of biologicals is not feasible in several setups.
Exacerbations in psoriasis after stopping systemic therapies is a major challenge which may require repeated cycles of systemic agents in severe disease. There are limited systematic studies in published literature evaluating systemic maintenance therapies in psoriasis to prevent exacerbations. Fernandes et al. compared WCT after inducing remission with continuous CYC for 12 weeks versus continuous CYC for 20 weeks as maintenance therapy in psoriasis and found them comparable in efficacy.6 We further explored WCT as maintenance therapy in psoriasis patients with a previous history of frequent exacerbations and compared it with matched patients, not on any maintenance systemic therapies. The duration of follow-up (11.64 ± 3.13 months) and number of patients on WCT (n = 22) were higher in our study as compared to those (20 weeks and n = 10) in the study by Fernandes et al.6 Also, patients only with a previous history of frequent exacerbations (≥ 3 exacerbations in the last 1 year) were included in our study while no such criteria were used in the study by Fernanades et al.6
In a similar study, Colombo et al. tried to assess the efficacy and tolerability of WCT for the prevention of exacerbations.5 The follow-up period was 24 weeks and the clinical success rate (relapse-free follow-up period) was found to be higher in the CYC group (66.9%) as compared to the placebo group (55.2%), but the difference could not reach statistical significance (p = 0.07). However, when only patients with moderate to severe psoriasis were accounted for (excluding mild cases) in their study, the difference in success rate reached statistical significance (69.9% vs 46.3%, p = 0.01). The disparity in “success rate” in our study as compared to Colombo et al.5 can be attributed to several factors in their study which include a different definition of relapse (PASI> 75% of baseline) and shorter study duration. Moreover, only patients who had a history of frequent exacerbations (≥ 3 or more in 1 year before the induction phase) were included in our study while there was no such criterion in the study by Colombo et al. Like our study, Colombo et al. found that WCT was well tolerated with no serious adverse effects attributed to drug intake. In addition, there was no significant difference in raised serum creatinine and blood pressure between the CYC and placebo groups in their research.5
Apart from psoriasis, WCT as maintenance therapy has also been tried in patients of chronic atopic dermatitis in which 4/5 (80%) patients maintained remission on WCT, suggesting that it can be further explored as maintenance therapy in atopic dermatitis and other chronic cutaneous inflammatory disorders where CYC is a therapeutic option.10
The findings of our study also suggested that WCT is a safe and effective modality for preventing exacerbations in chronic plaque psoriasis with a tendency for frequent exacerbations often requiring systemic modalities for control. Significantly fewer patients on WCT had exacerbations as compared to the non-WCT group indicating the effective role of WCT in the prevention of exacerbations. The incidence of adverse effects in the WCT group was seen only in two (9.1%) patients, while none was serious.
This is the first study in which the efficacy of WCT was evaluated in the specific subset of psoriasis patients with a history of frequent exacerbations in the past. The use of WCT as maintenance therapy in these patients is justified to prevent exacerbations and improve the quality of life. Also, the mean duration of MP in our study (11.64 ± 3.13 months) was considerably longer as compared to previous studies (20 weeks and 24 weeks by Fernandez et al.6 and Colombo et al.5, respectively).
The swift action of CYC on the inflammatory cells (T lymphocytes) and endothelial cells within 72 hours, its liposolubility in adipose tissue (high lipid content in skin) which acts as a reservoir enhancing its bioavailability and slow inflammatory recovery time in psoriasis as compared to other inflammatory skin disorders may be the factors contributing to the efficacy of WCT in psoriasis allowing treatment discontinuation of 5 days.11
Retrospective design of the study was a major limitation of the study. Another limitation was that the duration of CYC treatment for the management of exacerbations was not uniform and based on achievement of PASI 90.
Conclusion
To conclude, WCT is an efficacious and safe systemic modality for the prevention of exacerbations in chronic plaque psoriasis patients and can be considered as maintenance therapy in those having a tendency for frequent relapses.
Ethical approval
As this was a retrospective study, prior ethical approval was not needed. Nonetheless, all efforts were made to adhere to ethical standards ensuring patient confidentiality and privacy throughout the research process.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Cyclosporine consensus conference: With emphasis on the treatment of psoriasis. J Am Acad Dermatol. 1998;39:464-75.
- [CrossRef] [PubMed] [Google Scholar]
- Oral cyclosporin in psoriasis: A systematic review on treatment modalities, risk of kidney toxicity and evidence for use in non‐plaque psoriasis. J Eur Acad Dermatol Venereol. 2011;25:19-27.
- [CrossRef] [PubMed] [Google Scholar]
- Intermittent vs. continuous 1‐year cyclosporin use in chronic plaque psoriasis. J Eur Acad Dermatol Venereol. 2007;21:1203-8.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life and clinical outcome in psoriasis patients using intermittent cyclosporin. Br J Dermatol. 2001;144:967-72.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis relapse evaluation with week-end cyclosporine A treatment: Results of a randomized, double-blind, multicenter study. Int J Immunopathol Pharmacol. 2010;23:1143-52.
- [CrossRef] [PubMed] [Google Scholar]
- Maintenance treatment of psoriasis with cyclosporine A: comparison between continuous and weekend therapy. J Am Acad Dermatol. 2013;68:341-2.
- [CrossRef] [PubMed] [Google Scholar]
- Implementing treatment goals for successful long‐term management of psoriasis. J Eur Acad Dermatol Venereol. 2012;26:12-20.
- [CrossRef] [PubMed] [Google Scholar]
- S3–Guidelines on the treatment of psoriasis vulgaris. J Dtsch Dermatol Ges. 2012;10:s1-s95.
- [Google Scholar]
- Current guidelines for psoriasis treatment: A work in progress. Cutis. 2018;101:10-2.
- [PubMed] [Google Scholar]
- Oral cyclosporine weekend therapy: A new maintenance therapeutic option in patients with severe atopic dermatitis. Pediatr Dermatol. 2015;32:551-2.
- [CrossRef] [PubMed] [Google Scholar]
- Ciclosporina-A e week-end therapy nella psoriasi a placche: La nostra esperienza. Bollettino della Società Medico Chirurgica di Pavia. 2011;124:217-25.
- [PubMed] [Google Scholar]







