Translate this page into:
Combined approach for intra-oral paratrichosis using electro-epilation and long pulsed NdYAG laser
Corresponding author: Dr. Sushil S. Savant Jr, Department of Dermatology, The Humanitarian Clinic: Skin, Hair and Laser Centre, Mumbai, Maharashtra, India. sushilsavant786@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Savant SS. Combined approach for intra-oral paratrichosis using electro-epilation and long pulsed NdYAG laser. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_125_2024
Dear Editor,
Intraoral paratrichosis commonly affects men following maxillofacial reconstruction for oral carcinoma.1 Presence of unwanted hair can downgrade patient’s quality of life (QoL) due to foul odour from entrapped food, pooling of saliva, gagging, nausea, intermittent dysphagia, and dysphonia, as well as oral paraesthesia. Treatment options include radiotherapy, revised surgery, flap de-epithelialisation, electro-epilation, and lasers.1,2 Here, we described the use of the serial combination technique of teflon-coated needle, electro-epilation, and 1064 nm long-pulsed Nd: YAG laser to treat two cases of intra-oral paratrichosis.
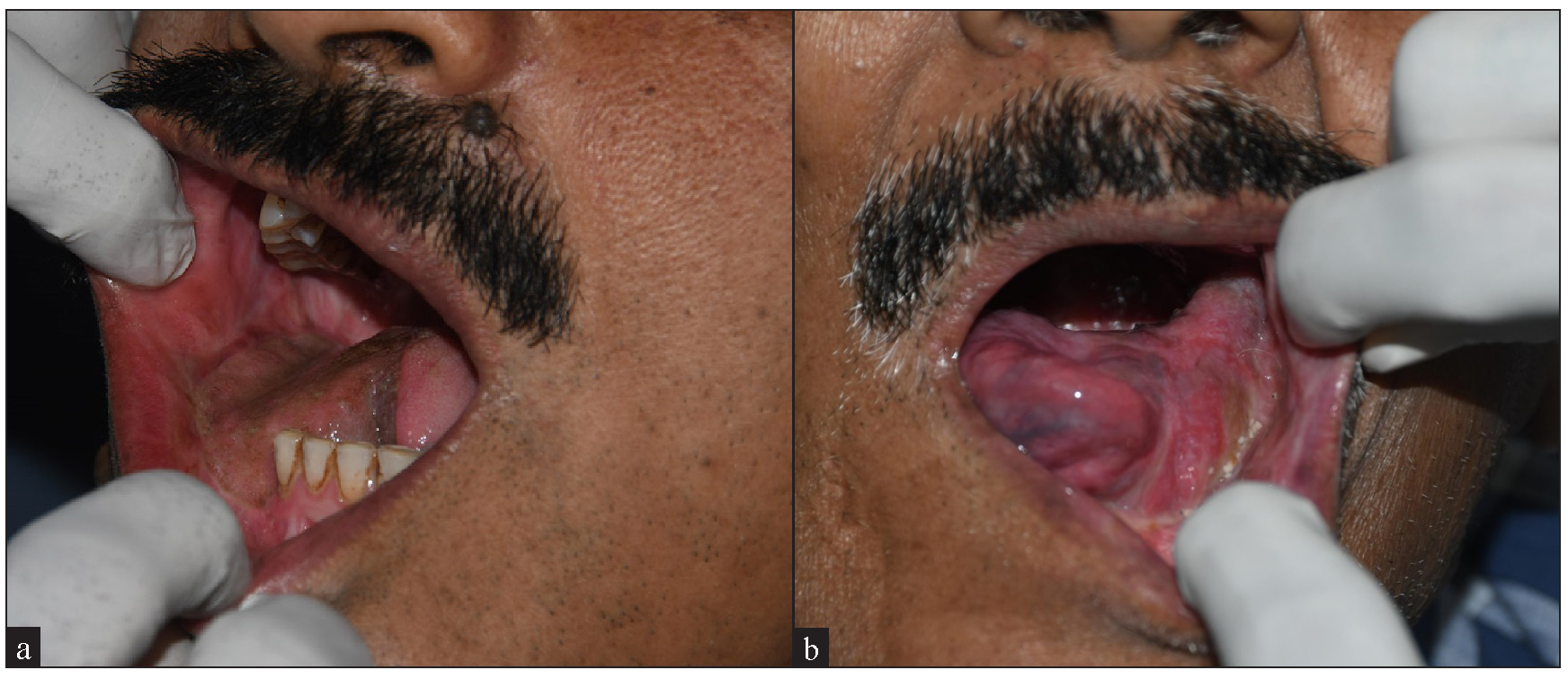
A 57-year-old man had thick terminal hair distributed over the right oral mucosa on the submental flap in parallel to the right lower molars [Figure 1a], following reconstructive surgery for tongue squamous cell carcinoma (SCC) a year ago. He experienced dysphagia, dysphonia, and bad odour with entangled food particles. On examination, terminal hairs were 0.6 to 1cm long with black hairs outnumbering white hairs.

- Thick terminal hair distributed over the right aspect of oral mucosa on the submental flap.
Our second case was a 69-year-old man who had thick terminal hair along the distribution of the left lower molars over the reconstructed site with radial free flap following radical excision of SCC of the tongue 9 months ago [Figure 1b]. He had dribbling of saliva, dysphagia, and gagging sensation with halitosis from entrapped food affecting QoL. On examination, terminal hairs were 0.8 to 1.4 cm long with white hairs outnumbering black hairs.

- Thick terminal hair along the distribution of left lower first, second, a nd third molars over the reconstructed site with radial free flap.
Both cases underwent three sessions of a combined approach involving teflon-coated needle electro-epilation (teflon-coated needle) followed by 1064 nm long-pulsed Nd: YAG laser treatment, done 8 weeks apart. After infiltrating the area with 2% plain lignocaine, electroepilation was done. Teflon-coated needle was attached to an electrocautery device (high electric current, 2 J/cm2). The needle tip was inserted in the direction of both white and black hair follicles till complete resistance was felt in antegrade movement resulting in perifollicular dimpling. The needle was slightly withdrawn, and the foot switch was used to release current at the base of the hair follicle over 1–3 seconds in 2–4 rapid spurts. The needle was then withdrawn and halfway through the hair follicle, an additional spurt of current was passed for better destruction. There was mild blanching in the peri-follicular area including the needle probe that was gauged as an end point, and the needle was completely withdrawn. Epilation forceps was employed to exert pull along the direction of the hair shaft, allowing for removal of the cauterised hair root along with the shaft. This was followed by a 1064 nm long-pulsed Nd: YAG laser setting (spot size: 10 mm, power: 29 watts, fluence: 175 J/cm, pulse width: 300 µs2). The laser handpiece was held perpendicularly in direct contact over the electro-epilated field, and moved to cover the target area horizontally and vertically to provide two consecutive passes with 10% overlap. There was difficulty in manoeuvring the hand piece over the posterior oral cavity, but laser energy was partially delivered by keeping the head nearest to the target. Simultaneous use of a smoke evacuator and cold air flow cooling device near the mouth opening avoids intraoral laser plume accumulation and facilitates a cool environment over the mucosal bed during long-pulsed Nd:YAG laser, thereby minimising pain and lateral thermal damage of the epithelial surface.
Teflon-coated needles are micro-needles (400 µm in diameter). They insulate along their length except at non-insulated tapered active needle tip (200 µm) from where energy is released. Heat generated causes coagulative necrosis, dessication, and destruction of hair root, while sparing the epidermis.2 Selective cooling of the epidermis is crucial to prevent adverse effects (blistering and post-inflammatory hyper- and/or hypopigmentation) when using laser systems for intra-oral paratrichosis. For intra-oral paratrichosis, a laser system with a narrow elongated hand piece is preferable and easily manoeuvred over the target area inside the oral cavity.3
The 1064 nm long-pulsed Nd: YAG laser causes minimal side effects and is more suitable for dark skin phototype. It is costly and requires multiple sessions without effect on grey/white hairs. The hand piece is comparatively narrower causing less difficulty in manoeuvring the posterior oral cavity with partial delivery of energy.4
Combining teflon-coated needle electro-epilation and 1064 nm long-pulsed Nd:YAG laser treatment offers a novel, effective approach for intra-oral paratrichosis. This multipronged method provides lasting, sustained, and safe results for both black and white hairs, enhancing functional and aesthetic outcomes without onchologic/trichologic recurrence in minimum sittings, thus improving a patient’s QoL. Since both patients presented with a mix of black and white hair, a combined approach was employed: electroepilation for white and black hair and long-pulsed Nd laser for seeded black hair. This combination could not only target visible black and white hair but could also achieve a zero hair growth by further targeting any seeded hair follicles through laser post epilation. It gradually reduces intra-oral hair count and successfully achieves zero hair count after three sessions. No intra-oral hair regrowth observed in both patients during 2-year long-term follow-up [Figure 2a and 2b]. However, mild pain, discomfort, and bleeding post-procedure can occur which can be treated with analgesics. Sessions can be repeated every 6–8 weeks till desirable results are achieved.
- No regrowth of hair in both patients after 3 laser sessions and 2-year follow up.
With this dual approach, we achieved long, sustained, and permanent hair removal with no onchologic/trichologic recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- A protocol for management of the hairs problem in oral cavity reconstruction by submental flap. J Maxillofac Oral Surg.. 2017;16:108-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Excessive hair in women. In: Savant SS, ed. Textbook of dermatosurgery and cosmetology principles and practice (3rd edition). Mumbai: Bhalani Publishing House; 2018. p. :1002-9.
- [Google Scholar]
- Successful ablation of iatrogenic intraoral hypertrichosis post mandibular reconstruction using a thermolysis hair epilation technique. Dermatol Surg.. 2013;39:1933-5.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional radiofrequency: Microneedle fractional and superficial fractional. In: Savant SS, ed. Textbook of dermatosurgery and cosmetology principles and practice (3rd edition). Mumbai: Bhalani Publishing House; 2018. p. :1075-88.
- [Google Scholar]





