Translate this page into:
Aleukemic leukemia cutis mimicking urticaria pigmentosa in a patient of T-cell acute lymphoblastic leukemia
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Neetu Bhari
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi
India
| How to cite this article: Singh S, Taneja N, Kaul S, Arava S, Bhari N. Aleukemic leukemia cutis mimicking urticaria pigmentosa in a patient of T-cell acute lymphoblastic leukemia. Indian J Dermatol Venereol Leprol 2020;86:105 |
Sir,
A 24-year-old woman presented with progressively increasing itchy, erythematous lesions on the face, trunk and arms since the past 6 months. She also complained of a slight reduction in appetite with mild constitutional symptoms, viz., malaise and early fatigue of 15 days' duration. On examination, there was predominant involvement of malar area and lateral part of the cheeks, trunk and both arms with multiple erythematous to brownish macules and plaques ranging from 0.5 to 3 cm in size [Figure - 1]a. The Darier's sign was strongly positive in the lesional skin [Figure - 1]b. Generalized lymphadenopathy with involvement of cervical, axillary and inguinal areas was present. With a clinical diagnosis of adult-onset mastocytosis, complete blood counts, serum trypsin levels and peripheral blood smear were evaluated, which were within normal limits. Skin biopsy on hematoxylin and eosin staining showed a pan-dermal dense infiltrate of lymphocytes and histiocytes, with few atypical lymphocytes [Figure - 2]a. Mast cells were absent and this finding was confirmed with Giemsa and toluidine blue staining. Four weeks after the initial visit, the complete blood count and peripheral blood smear were repeated, which revealed lymphocytosis (60%) along with some atypical cells in peripheral blood smear. A bone marrow biopsy was performed, which showed multiple, large atypical cells [Figure - 3]a. These cells showed negative staining for the markers of myeloid lineage, i.e. myeloperoxidase, Sudan black B and nonspecific esterase [Figure - 3]b and [Figure - 3]c. Immunophenotyping by flow cytometry showed positivity with CD3, CD5, CD7 and terminal deoxynucleotidyl transferase. Immunohistochemical staining of skin biopsy with CD3 and terminal deoxynucleotidyl transferase also revealed positive staining, suggesting the origin of lymphocytes being of T-cell lineage [Figure - 2]b and [Figure - 2]c, thus confirming the diagnosis of leukemia cutis masquerading as adult-onset mastocytosis with T-cell acute lymphoblastic leukemia. Leukemia cutis was further designated as aleukemic leukemia cutis because cutaneous involvement preceded the deranged hematological profile. The patient was referred to the hemato-oncology unit for further management, and was started on augmented Berlin-Frankfurt-Munster therapy for acute lymphoblastic leukemia. After consolidation phase of chemotherapy, the patient had flattening of her lesions and the erythematous lesions gradually turned hyperpigmented.
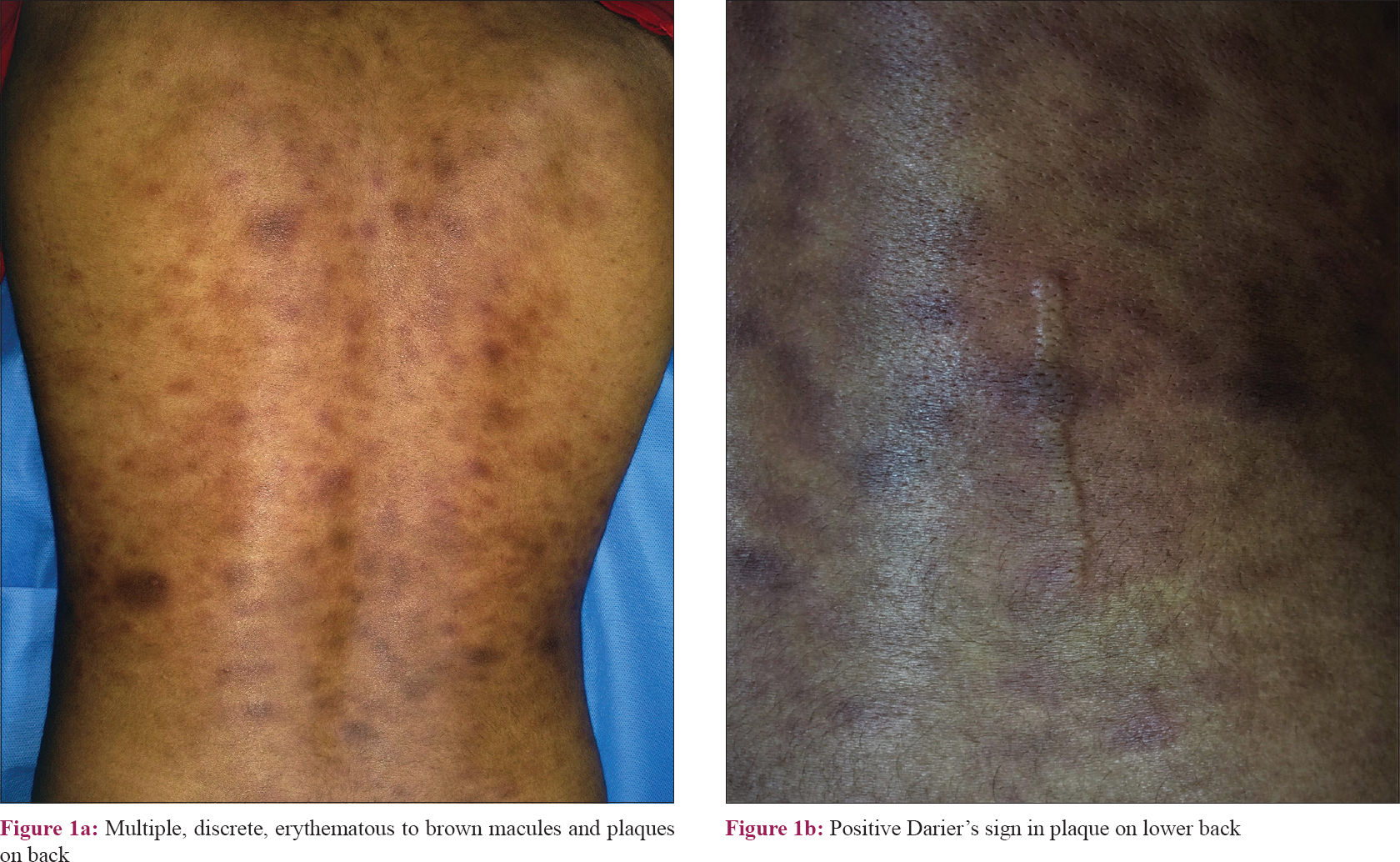 |
| Figure 1: |
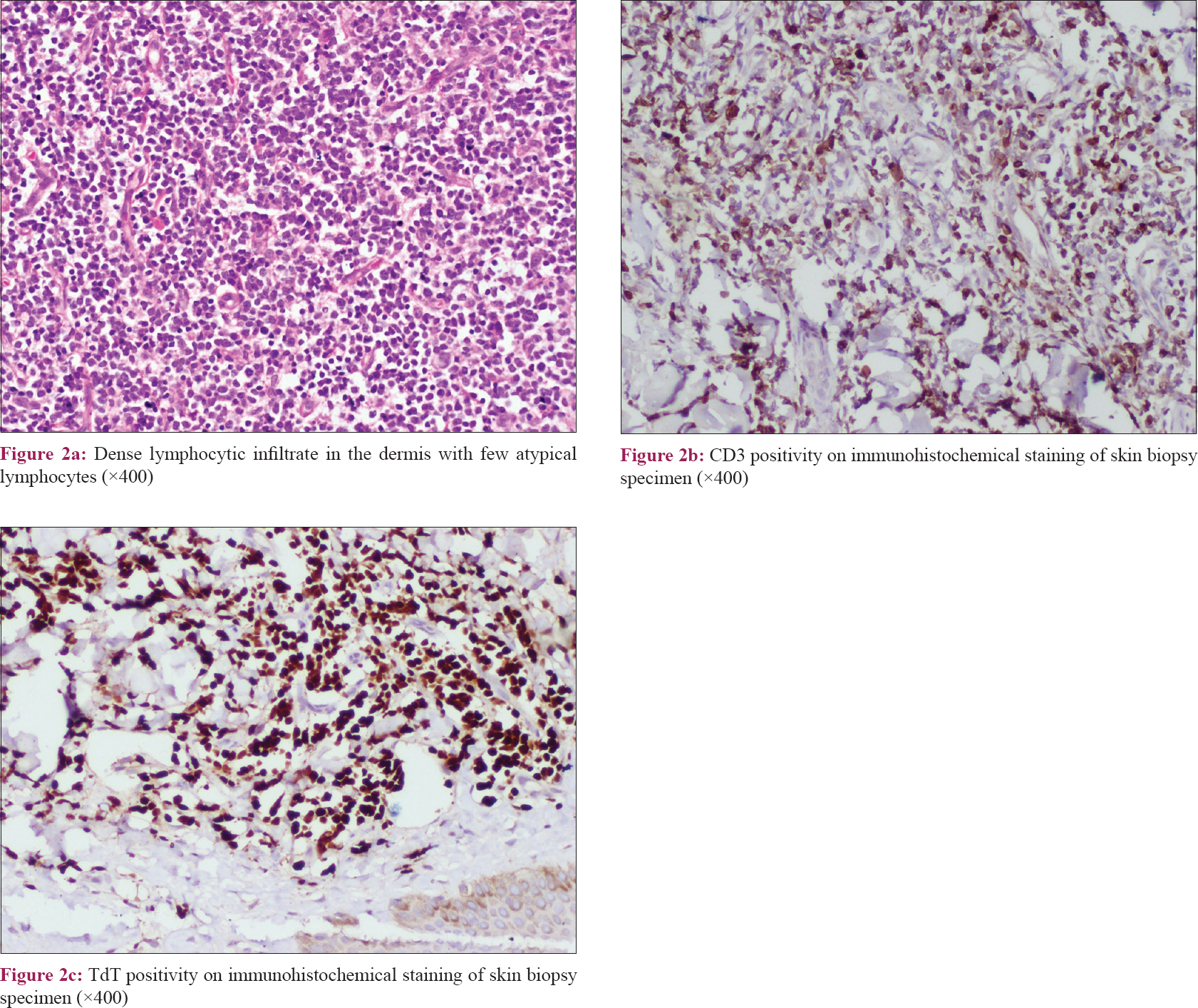 |
| Figure 2: |
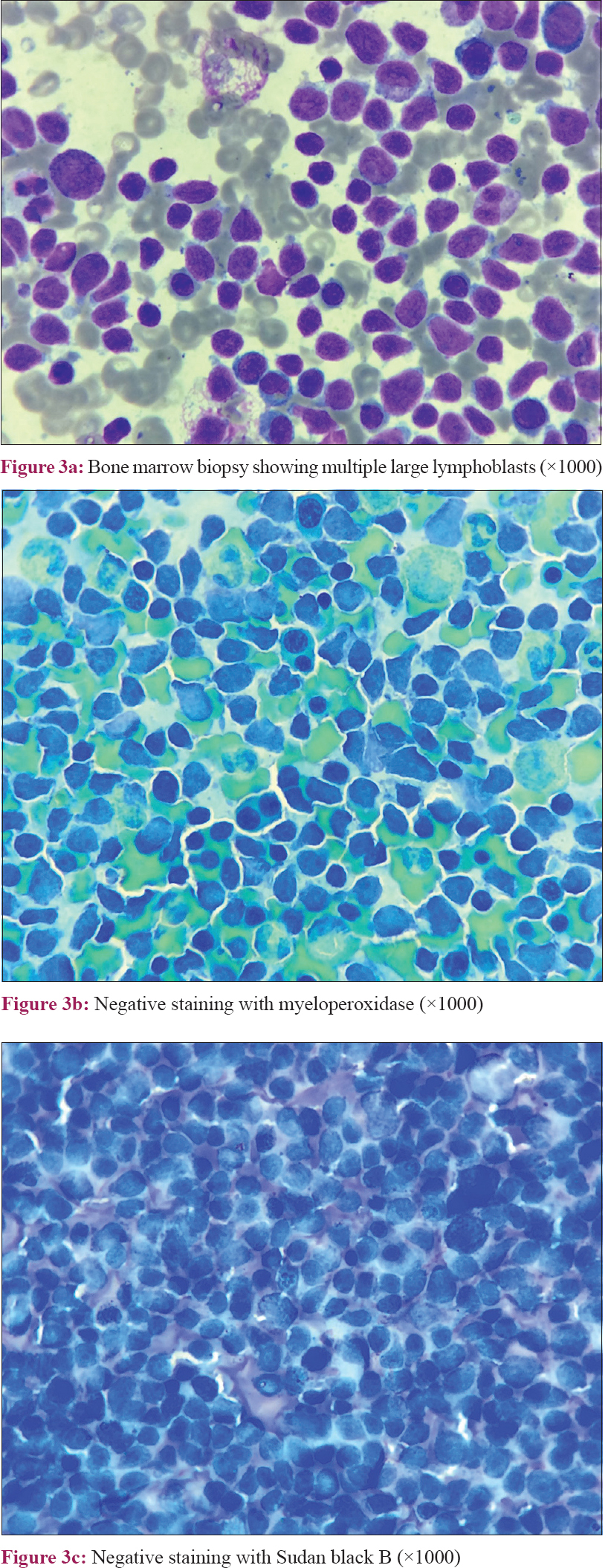 |
| Figure 3: |
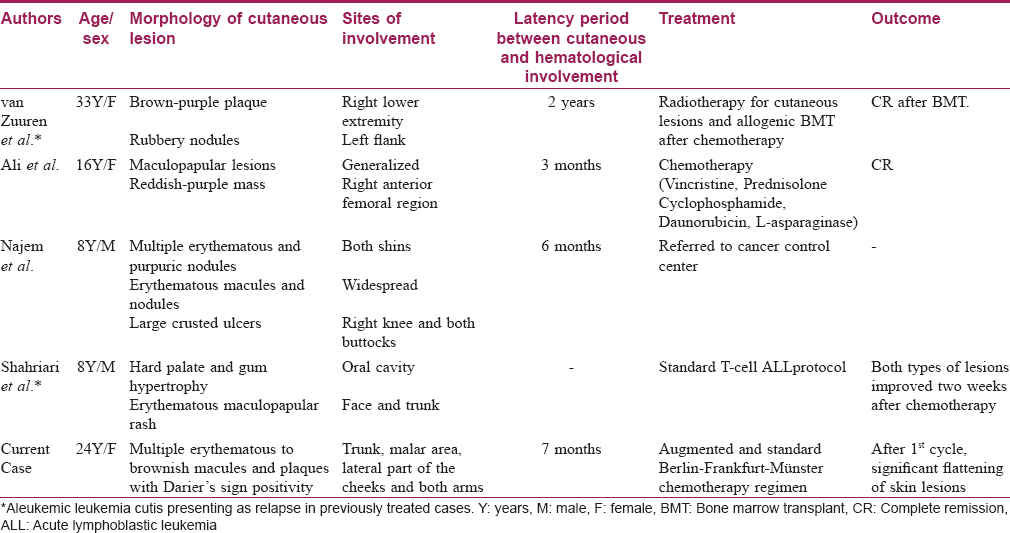
Leukemia cutis is defined as a cutaneous infiltration of leukemic cells, and is an extramedullary manifestation of underlying leukemia. It is observed more frequently in acute myeloid leukemia, particularly in myelomonocytic (M4) and monoblastic (M5) subtypes.[1] Cutaneous involvement in acute lymphoblastic leukemia is uncommon with an incidence ranging from 1 to 3%.[2] Furthermore, its T-cell variant rarely presents as leukemia cutis. The commonest cutaneous presentation of leukemia cutis is that of asymptomatic, indurated papules and nodules.[3] Macules, maculopapular lesions, plaques, ulcers, bullae, large nodule, ecchymosis, palpable purpura and erythroderma are uncommon presentations.[1],[3] The lower extremities are the most commonly involved site followed by the upper extremities, trunk, scalp and face.[2],[4] Leukemic changes in peripheral blood or bone marrow usually develop before skin involvement. Occasionally, leukemia cutis precedes the diagnosis of systemic leukemia by several months or even years (mean 6 months).[5] This interesting condition is known as aleukemic leukemia cutis. T-cell acute lymphoblastic leukemia presenting as aleukemic leukemia cutis is rarely described in the literature [Table - 1]. There is relative paucity of literature with regards to this clinical presentation on the overall prognosis; nonetheless, reports of a poor outcome do exist.[1],[4] Association of urticaria pigmentosa-like lesions with acute lymphoblastic leukemia has been described previously in case reports.[6]
In the classical Darier's sign, local itching, erythema and wheal formation occur within 2–5 minutes of gentle rubbing or stroking of the cutaneous lesions. It is considered to be pathognomonic of cutaneous mastocytosis; however, it is seen uncommonly in various other dermatological disorders such as leukemia cutis, juvenile xanthogranuloma, Langerhans cell histiocytosis and cutaneous large T-cell lymphoma.[7] As far as ascertained, our case is the first case of aleukemic leukemia cutis with the Darier's sign positivity, mimicking as urticaria pigmentosa, in a patient of T-cell acute lymphoblastic leukemia.
In conclusion, T-cell acute lymphoblastic leukemia rarely leads to leukemia cutis and furthermore, aleukemic leukemia cutis and dermatologic presentation masquerading as urticaria pigmentosa is very uncommon.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ali R, Ozan U, Ozkalemkas F, Ozcelik T, Ozkocaman V, Ozturk H, et al. Leukaemia cutis in T-cell acute lymphoblastic leukaemia. Cytopathology 2006;17:158-61.
[Google Scholar]
|
| 2. |
Jiang X, Wang W, Zhang M. Leukemia cutis: An unusual presentation of acute lymphoblastic leukemia in a child. Indian J Dermatol 2015;60:636.
[Google Scholar]
|
| 3. |
Najem N, Zadeh VB, Badawi M, Kumar R, Al-Otaibi S, Al-Abdulrazzaq A. Aleukemic leukemia cutis in a child preceding T-cell acute lymphoblastic leukemia. Pediatr Dermatol 2011;28:535-7.
[Google Scholar]
|
| 4. |
Shahriari M, Fathpour G, Saleh F. Mucocutaneous relapse as an unusual presentation of T-lineage acute lymphoblastic leukemia. Middle East J Cancer 2015;7:63-6.
[Google Scholar]
|
| 5. |
van Zuuren EJ, Wintzen M, Jansen PM, Willemze R. Aleukaemic leukaemia cutis in a patient with acute T-cell lymphoblastic leukaemia. Clin Exp Dermatol 2003;28:330-2.
[Google Scholar]
|
| 6. |
Masserot C, Adjaoud D, Haouy S, Deswarte C, Ballerini P, Landman-Parker J. Acute lymphoblastic leukemia and cutaneous mastocytosis in two children. Pediatr Blood Cancer 2008;51:444-5.
[Google Scholar]
|
| 7. |
Surjushe A, Jindal S, Gote P, Saple DG. Darier's sign. Indian J Dermatol Venereol Leprol 2007;73:363-4.
[Google Scholar]
|
Fulltext Views
3,826
PDF downloads
3,456





