Translate this page into:
Periungual tumor on the finger
Correspondence Address:
Jin Yu
Department of Dermatology and Venerology, Peking University First Hospital, 1st Xi'an Men Street, Xicheng District, Beijing
China
| How to cite this article: Wang XX, Yu J. Periungual tumor on the finger. Indian J Dermatol Venereol Leprol 2020;86:549-551 |
Sir,
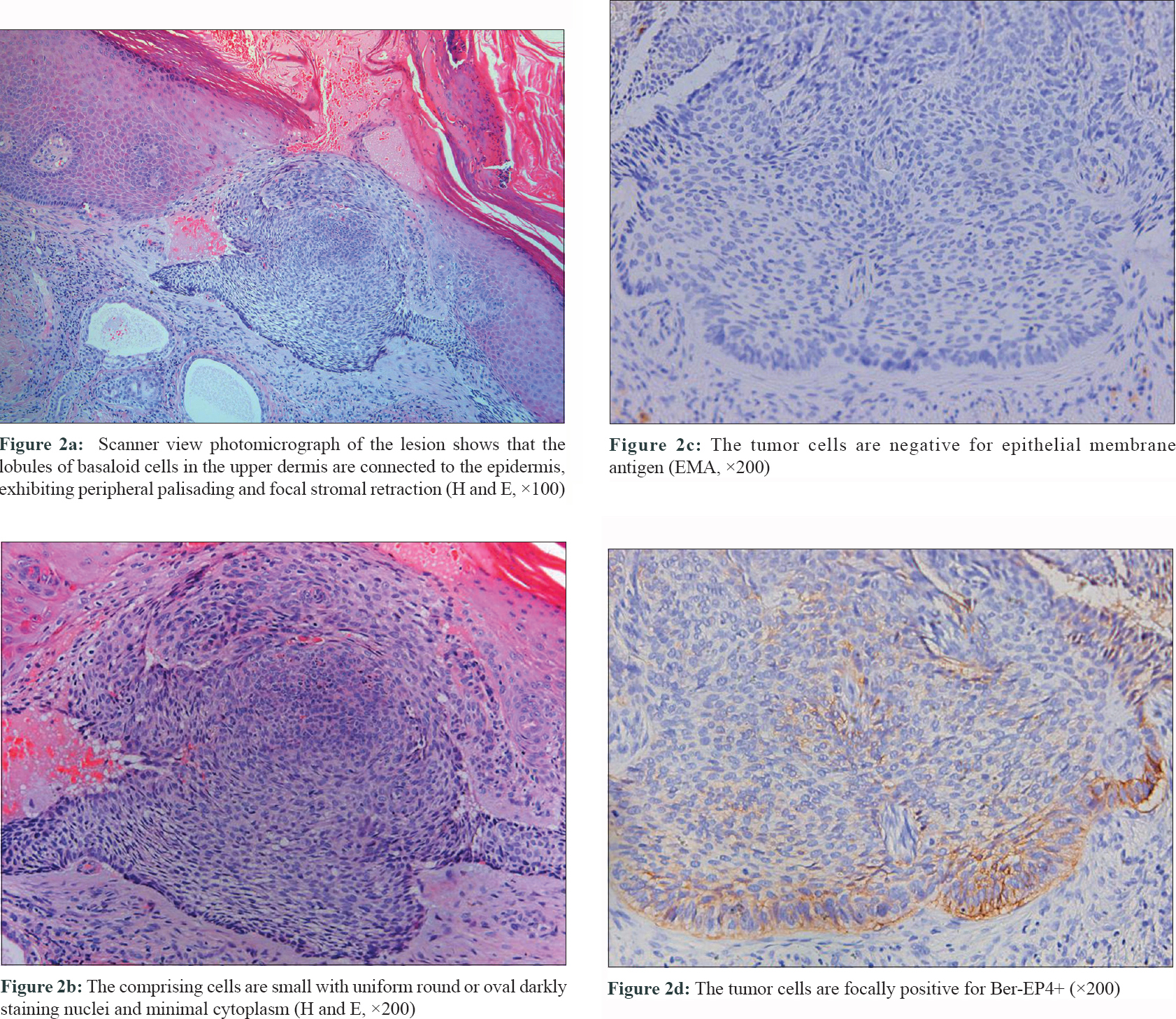
An apparently healthy 73-year-old man presented with a slow-growing mass, 1.0-cm in diameter, affecting the periungual region of his left middle finger, with ulceration and rolled out edges for three years. The lesion gradually invaded his nail to cause nail-bed hyperkeratosis [Figure - 1]. Lesional histopathology revealed nodules of basaloid cells (small cells having minimal cytoplasm with uniform round or oval darkly staining nuclei) interspersed with palisading and stromal retraction; predominantly affecting the upper dermis with epidermal intrusion [Figure - 2]a and b]. Tumor cells stained negative for epithelial membrane antigen [Figure - 2]c and Sox2, and positive for Ber-EP4 [Figure - 2]d, thus confirming the diagnosis of basal cell carcinoma. We performed Mohs micrographic surgery [Figure - 3]a. No recurrence has been noted at one-year follow-up [Figure - 3]b.
 |
| Figure 1: A 1.0 cm mass in the periungual region of the middle finger, with ulceration and rolled out edges and hyperkeratosis of the nail bed |
 |
 |
Basal cell carcinoma is the commonest skin neoplasm, but the least common nail tumor.[1] It predominantly affects the head and neck region,[2] nail unit involvement being extremely rare with only 31 reports in the English literature.[1],[2],[3] Fingers are involved more than toes, thumb being the commonest digit.[1]
Basal cell carcinoma is primarily caused by ultraviolet radiation, however, the rarity of nail unit basal cell carcinoma despite digits being relatively well sun-exposed remains unexplained.[1],[3] The paucity of pilosebaceous units in this region might be a possible reason.[4] Some factors implicated for the etiopathogenesis of nail unit basal cell carcinoma include trauma, carcinogens (azo dyes and arsenic) and chronic radiation exposure.[1]
The clinical presentation of nail unit basal cell carcinoma is variable, resembling several inflammatory or infectious diseases of the nail including chronic paronychia, dermatophytosis, bacterial infections, herpes simplex, chronic eczema and trauma. Differential diagnoses also include other benign or malignant neoplasms like pyogenic granuloma, squamous cell carcinoma, Bowen's disease, glomus tumor and longitudinal melanonychia or melanoma.[3],[5] It can also be misdiagnosed as a habit tic.[6] Characteristic dermoscopic features of basal cell carcinoma help us to rule out other clinical mimickers, however, histopathological examination is essential for diagnosis.[3]
Various therapeutic modalities exist for this condition like topical imiquimod, topical 5-fluorouracil, intralesional interferon, radiation therapy, electrodessication and curettage, cryosurgery, laser, standard excision and Mohs micrographic surgery.[2] Surgical excision is the treatment of choice due to lowest rate of recurrence.[2] Compared to standard surgical excision, Mohs micrographic surgery ensures better tissue conservation and marginal clearance, thus resulting in maximum preservation of digital function.[1] As a result, Mohs micrographic surgery is currently the most favoured treatment option for nail unit basal cell carcinoma where tissue conservation is important. Forman et al. concluded that 8 of the initial 22 reported cases of nail unit basal cell carcinoma were successfully treated with Mohs micrographic surgery.[5] Five cases healed by second intention while three cases required full-thickness skin grafts.[5] Until now, Mohs micrographic surgery has been performed for 14 nail unit basal cell carcinomas in English literature, including our case. In conclusion, Mohs micrographic surgery is a satisfactory treatment option for nail unit epithelial neoplasms, including basal cell carcinoma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal the identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Shimizu I, Cohen PR, Macfarlane DF. Surgical treatment of basal cell carcinoma of the nail unit. Int J Dermatol 2013;52:996-8.
[Google Scholar]
|
| 2. |
Pollo T, Rabay FM, de Lima EM, Gonçalves FD, Mandelbaum SH. Subungual basal cell carcinoma: A rare nail tumor with a challenging diagnosis. Skin Appendage Disord 2019;5:251-3.
[Google Scholar]
|
| 3. |
Tavares LL, Costa JC, Delcourt NC, Rodrigues NC. Periungual basal cell carcinoma. An Bras Dermatol 2018;93:114-5.
[Google Scholar]
|
| 4. |
Bandyopadhyay D, Sen S. Periungual Basal cell carcinoma: A case report with review of literature. Indian J Dermatol 2011;56:220-2.
[Google Scholar]
|
| 5. |
Forman SB, Ferringer TC, Garrett AB. Basal cell carcinoma of the nail unit. J Am Acad Dermatol 2007;56:811-4.
[Google Scholar]
|
| 6. |
Shah D, Leopold G, Sowden J. Basal cell carcinoma masquerading as habit tic. Clin Exp Dermatol 2011;36:920.
[Google Scholar]
|
Fulltext Views
3,751
PDF downloads
2,114





