Translate this page into:
An unusual early onset of lentigo maligna in the fourth decade of life
2 Department of Plastic Surgery, Private Clinic, Metropolitan, Piraeus, Greece
Correspondence Address:
Eftychia Platsidaki
5, Ionos Dragoumi Street, Athens 16121
Greece
| How to cite this article: Platsidaki E, Kostopoulos N, Gesakis K, Polydorou D, Agiasofitou E. An unusual early onset of lentigo maligna in the fourth decade of life. Indian J Dermatol Venereol Leprol 2019;85:129 |
Sir,
Lentigo maligna (LM) occurs on the sun-exposed skin, particularly the head and neck. Clinically, it presents as a slow-growing, asymmetric macule with irregular, poorly-defined borders and varied pigmentation. Areas of partial regression within the lesion are not uncommon. With such lesions, the differential diagnosis includes solar lentigo (flat seborrheic keratosis), pigmented actinic keratosis and lichenoid keratosis.[1] Dermoscopy has been demonstrated to be an efficient technique that helps the dermatologist to distinguish lentigo maligna from other melanocytic lesions. Patients with lentigo maligna tend to be older than those with superficial spreading malignant melanoma or nodular melanoma. In clinical practice, the peak age of diagnosis is between 60 and 80 years. Nevertheless, suspicion of lentigo maligna could be raised for the differential diagnosis of a pigmented lesion even in young adults.[2]
We report a case of a 36-year-old man with Fitzpatrick skin type III who presented with an unevenly pigmented brown plaque on the right side of his upper lip involving the vermilion border, the oral commissure and extending to his right cheek, measuring 35 × 25 mm [Figure - 1]. Based on a private photograph of the patient, we could ascertain that the lesion was already present at the age of 29 years. According to the patient, the above lesion started to increase in size rapidly over the last 3 months. He had no personal or family history of melanoma. He was employed as an outdoor construction worker for the last 10 years and was exposed to the sun without adequate protection.
 |
| Figure 1: An unevenly pigmented brown plaque on the right side of upper lip |
Dermoscopy revealed a multicomponent global pattern, with a pseudopigment network, asymmetric pigmented follicular openings, dark (brown or black) rhomboidal structures and slate-gray dots [Figure - 2]. The above findings raised the suspicion of lentigo maligna. Skin biopsy was obtained and showed a lentiginous proliferation of atypical melanocytes tracking down adnexae [Figure - 3] and [Figure - 4], confirming the initial diagnosis. Given the fact that the anatomical area was very demanding and Mohs micrographic surgery was not available in our hospital, a surgical excision (5 mm) with clear margins was performed by the plastic surgeons. The resulting defect was reconstructed with a local Estlander flap harvested from the lower lip. There were no signs of local recurrence and no obvious deformity (modiolus alteration or microstomia) during a follow-up visit after 3 months.
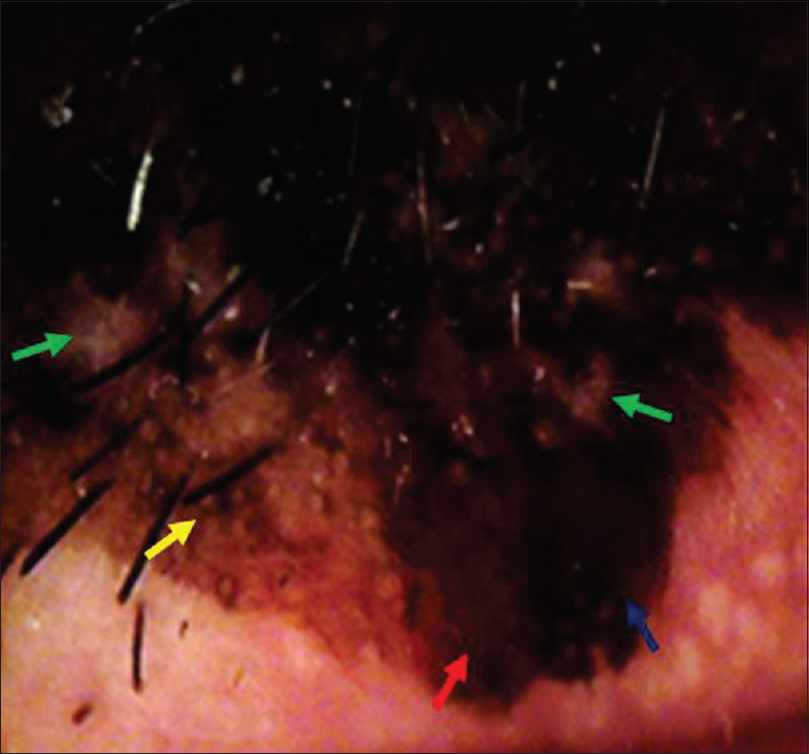 |
| Figure 2: Multicomponent pattern. Dark and bluish gray spots (green arrows), rhomboidal structures (yellow arrow), different shades of brown (blue arrow) and pseudopigment network (red arrow) |
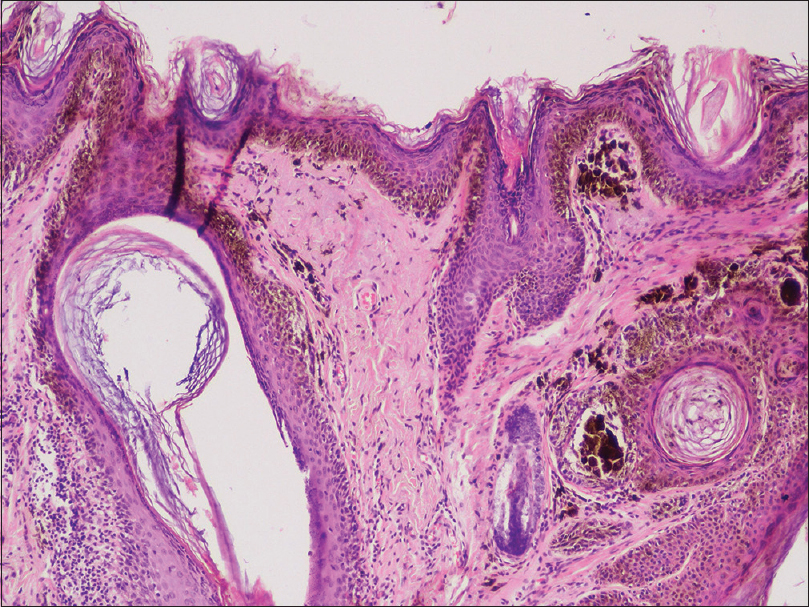 |
| Figure 3: Lentiginous proliferation of melanocytes tracking down adnexae (H and E, ×100) |
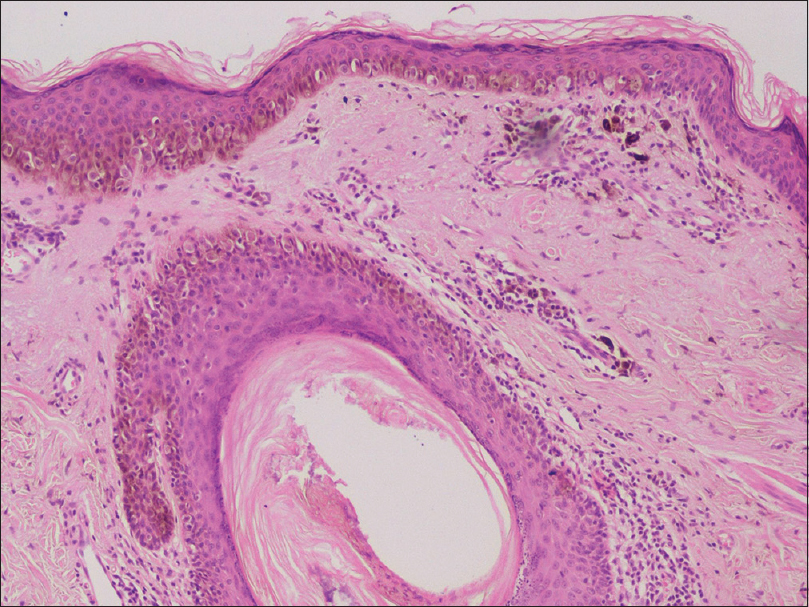 |
| Figure 4: Infiltration of melanophages and histiocytes in the dermis (H and E, ×100) |
Lentigo maligna is a lentiginous proliferation of atypical melanocytes confined to the epidermis, typically on chronically sun-damaged skin. Consequently, the most significant risk factor is considered to be lifetime ultraviolet radiation exposure. It increases in size even after many years of onset and may become lentigo maligna melanoma.[1] The diagnosis remains a challenge for clinicians because it often shows overlapping clinical features with benign lesions. The knowledge about patient's age as well as the site-related clinical features of lentigo maligna may enhance clinical recognition. The following four dermoscopic criteria in combination have achieved a diagnostic sensitivity of 89% and a specificity of 96%: asymmetric pigmented follicular openings, dark rhomboidal structures, slate gray dots and slate gray globules.[3] On the other hand, under dermoscopy, the presence of structureless homogenous pigmentation and numerous openings of hair follicle ostia and adnexal structures are characteristic of solar lentigo.[4] Histology remains the diagnostic method of choice and surgery remains the mainstay of treatment. Only a few isolated case reports were found in the published literature presenting lentigo maligna in adults younger than 40 years.[5] Our case underlines the fact that the clinical suspicion of lentigo maligna cannot be dismissed because of young age. In addition, our observation supports the effectiveness of dermoscopy in diagnosing pigmented skin lesions on the sun-exposed areas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Mazzei ME. Is it solar lentigo or lentigo maligna? (It is not a nevus). Actas Dermosifiliogr 2016;107:451-3.
[Google Scholar]
|
| 2. |
Helm MF, Bax MJ, Augenblick DJ, Chung CG. Melanoma in situ of lentigo maligna type in a young woman. Int J Dermatol 2017;56:961-2.
[Google Scholar]
|
| 3. |
Tschandl P, Rosendahl C, Kittler H. Dermatoscopy of flat pigmented facial lesions. J Eur Acad Dermatol Venereol 2015;29:120-7.
[Google Scholar]
|
| 4. |
Bollea-Garlatti LA, Galimberti GN, Galimberti RL. Lentigo maligna: Keys to dermoscopic diagnosis. Actas Dermosifiliogr 2016;107:489-97.
[Google Scholar]
|
| 5. |
Ferrara G, Ligrone L, Zalaudek I, Mordente I, Argenziano G. Lentigo maligna in a young adult. Dermatology 2008;217:66-8.
[Google Scholar]
|
Fulltext Views
2,469
PDF downloads
2,432





