Translate this page into:
Acquired cutis laxa associated with inflammatory bowel disease, inflammatory arthritis and IgA nephropathy
2 Department of Pathology, Christian Medical College, Vellore, Tamil Nadu, India
Correspondence Address:
Balakrishnan Nirmal
Department of Dermatology- Unit 1, Christian Medical College, Vellore, Tamil Nadu
India
| How to cite this article: Nirmal B, George R, Bindra MS. Acquired cutis laxa associated with inflammatory bowel disease, inflammatory arthritis and IgA nephropathy. Indian J Dermatol Venereol Leprol 2018;84:763 |
Sir,
Cutis laxa is a rare disorder of elastic tissue characterized clinically by lax pendulous skin and histologically by loss of dermal elastin. The disease can be inherited or acquired. The inherited form can be autosomal dominant, autosomal recessive or rarely X-linked. Autosomal dominant type is due to mutation in the elastin gene (ELN) and has a benign course with a few systemic manifestations including emphysema, bronchiectasis, genital prolapse and hernia. Autosomal recessive type is due to mutation of fibulin gene (FBLN 5,4), usually fatal, characterized by pulmonary emphysema, hernia and multiple diverticula.[1] Acquired cutis laxa may be type I (generalized) or type II (localized). There can be an underlying genetic susceptibility in acquired cutis laxa due to missense alleles in elastin and fibulin genes.[2] Systemic involvement is common in generalized acquired cutis laxa involving pulmonary, cardiovascular, gastrointestinal and urogenital systems. The findings include emphysema, pneumothorax, cardiomegaly, corpulmonale, aortic aneurysms, hernia, diverticula, cystocele and uterine prolapse. Type II or Marshall's syndrome is localized elastolysis usually characterized by preceding inflammatory skin lesions.[3]
A 25-year-old female from Bangladesh presented with a history of loose skin on the face, neck, axillae and abdomen for the past 3 years giving her an aged appearance. She also gave a history of recurrent wheals for the past 6 years. There was a history of abdominal pain involving the right upper quadrant and lower abdomen, and bleeding per rectum for the past 2 years. She also presented with inflammatory polyarthritis involving joints of both upper and lower limbs for the past 5 years. There was history of inadequate treatment with anti-tuberculosis therapy for pulmonary tuberculosis 5 years ago. There was no family history of lax skin or joint hyperextensiblity. On examination, the lax skin on the face, neck, axillae [Figure - 1] and abdomen had reduced recoil time after stretching. There were also skin-colored papules on the neck and striae distensae on the abdomen and thigh. Her blood parameters including complete blood count, liver function test, creatinine, electrolytes, antinuclear antibodies, complements, serum protein electrophoresis and rheumatoid factor were within normal limits. Serum alpha-1 antitrypsin level was 194 mg/dl (200–400 mg/dl). Urinalysis showed 7 RBCs/high power field and 24-hour urine protein was 424 mg/day (50–150 mg/day). Urine Bence–Jones protein was negative. Skin biopsy under hematoxylin and eosin staining showed mild increase in collagen and marked reduction in elastin fibers under orcein stain with fragmentation and elastolysis of elastin in the mid and deep dermis suggestive of cutis laxa [Figure - 2]. Renal biopsy showed mesangio-proliferative IgA deposits. Gastroscopy was normal and colonoscopy showed terminal ileal ulcers. Histopathology of the intestine revealed chronic active ileitis and pancolitis suggestive of Crohn's disease. Chest X-ray was normal. Computed tomography (CT) of the abdomen reported hepatomegaly with circumferential thickening of the bowel wall involving terminal ileum and rectosigmoid colon. We suggested her the option of plastic surgery for cutis laxa and referral to the relevant specialists for the treatment of associations. She was prescribed oral sulfasalazine 500 mg twice daily and oral losaratan 12.5 mg once daily at bedtime by gastroenterologist and nephrologist, respectively.
 |
| Figure 1: |
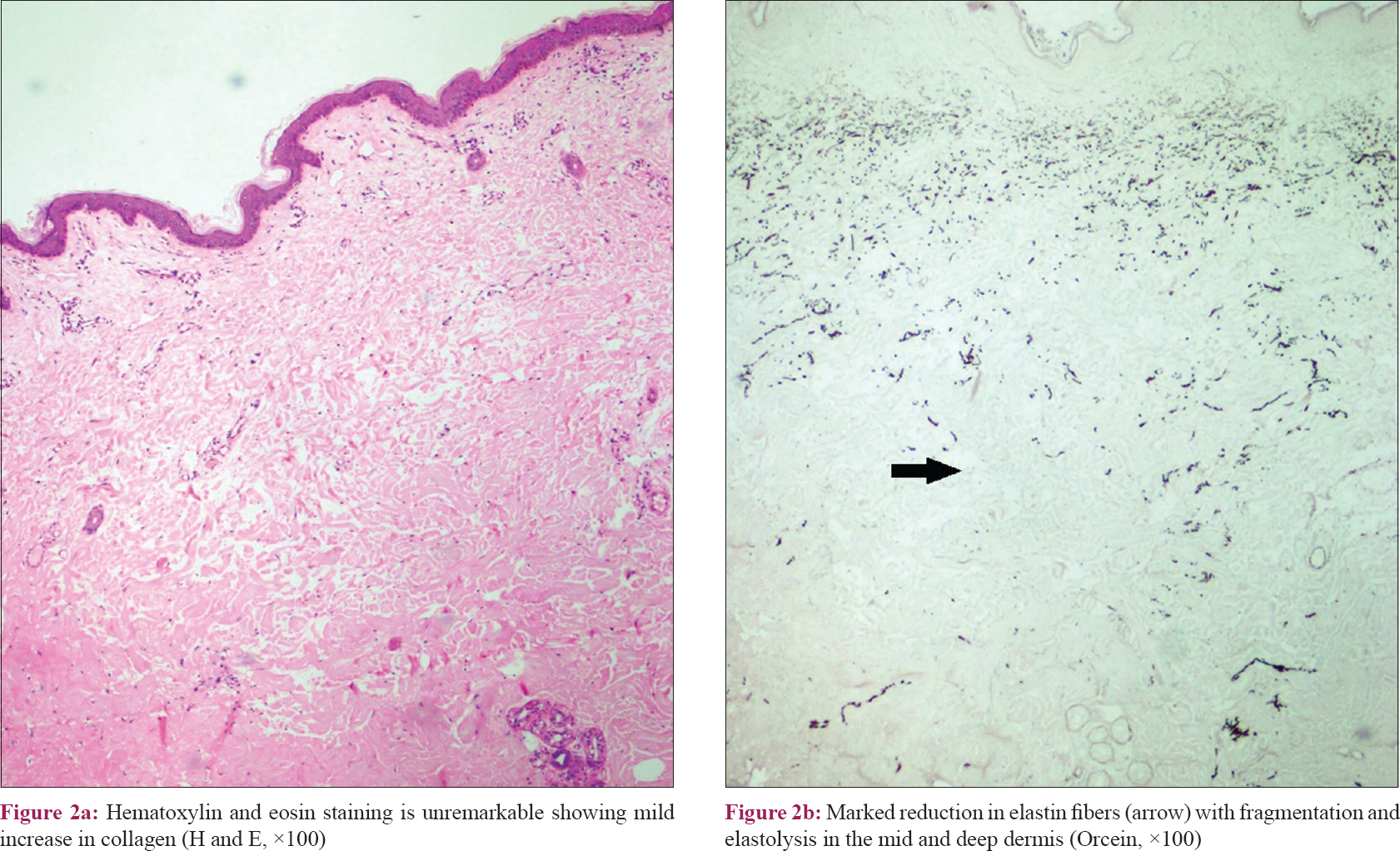 |
| Figure 2: |
Generalized acquired cutis laxa is a disorder of elastic tissue seen especially in adults characterized by appearance of lax skin beginning in the face and progressing cephalocaudally. More than half of the cases are preceded by or simultaneously develop inflammatory lesions such as edema, wheals or papulovesicles. Laxity can be also noticed in normal skin where there were no previous inflammatory lesions. Generalized acquired cutis laxa can be idiopathic or associated with infections, drugs, sarcoidosis, amyloidosis, systemic lupus erythematosus, glomerulonephritis, mesangial IgA nephropathy, paraproteinemia, multiple myeloma and Hodgkin's disease.[4] Our patient with generalized cutis laxa was associated with IgA nephropathy, Crohn's disease, and inflammatory polyarthritis suggesting that elastic tissue destruction may be an immune-mediated mechanism, as seen with these autoimmune disorders. Elastase from neutrophils act on the amorphous component of elastin in which microfibrils are embedded to make it susceptible to trypsin and pepsin digestion. Alpha1 antitrypsin is the main elastase inhibitor. Under the conditions of inflammation with neutrophil activation, normal serum levels of alpha1 antitrypsin is essential to prevent elastin digestion. Our patient had marginal decrease in alpha1 antitrypsin levels. Treatment for cutis laxa is unsatisfactory. Dapsone has been reported to control inflammation but was not able to halt the progression of the disease. Plastic surgery correction of the lax skin is an option in these patients; however, in many cases, surgery is unsuccessful.[5] This case is reported for its association with Crohn's disease, inflammatory arthritis and IgA nephropathy, which has not been reported in literature.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Alehossein M, Pourgholami M, Kamrani K, Soltani M, Yazdi A, Salamati P. Radiologic findings in cutis laxa syndrome and unusual association with hypertrophic pyloric stenosis. Iran J Radiol 2013;10:94-8.
[Google Scholar]
|
| 2. |
Gveric T, Baric M, Bulat V, Situm M, Pusic J, Huljev D, et al. Clinical presentation of a patient with localized acquired cutis laxa of abdomen: A case report. Dermatol Res Pract 2010;2010:402093.
[Google Scholar]
|
| 3. |
Fontenelle E, Almeida AP, Souza GM. Marshall's syndrome. An Bras Dermatol 2013;88:279-82.
[Google Scholar]
|
| 4. |
García-Patos V, Pujol RM, Barnadas MA, Pérez M, Moreno A, Condomines J, et al. Generalized acquired cutis laxa associated with coeliac disease: Evidence of immunoglobulin A deposits on the dermal elastic fibres. Br J Dermatol 1996;135:130-4.
[Google Scholar]
|
| 5. |
Rongioletti F, Cutolo M, Bondavalli P, Rebora A. Acral localized acquired cutis laxa associated with rheumatoid arthritis. J Am AcadDermatol 2002;46:128-30.
[Google Scholar]
|
Fulltext Views
2,934
PDF downloads
2,265





