Translate this page into:
Subclinical atherosclerosis and cardiovascular markers in patients with lichen planus: A case–control study
2 Department of Dermatology, Rasoul-e-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran
3 Department of Radiology, Shohada-e-Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Correspondence Address:
Afsaneh Sadeghzadeh-Bazargan
Department of Dermatology, Rasoul-e-Akram Hospital, Iran University of Medical Sciences, Tehran
Iran
| How to cite this article: Nasiri S, Sadeghzadeh-Bazargan A, Robati RM, Haghighatkhah HR, Younespour S. Subclinical atherosclerosis and cardiovascular markers in patients with lichen planus: A case–control study. Indian J Dermatol Venereol Leprol 2019;85:138-144 |
Abstract
Background: Lichen planus is an idiopathic and chronic inflammatory disease that affects the skin and the mucous membranes, and has been associated with an increased risk for cardiovascular diseases. Hyperhomocysteinemia has been regarded as a risk factor for atherosclerosis and cardiovascular diseases. Increased plasma fibrinogen levels are also associated with increased risk of myocardial infarction.
Objective: The main aim of this study is the evaluation of common carotid artery mean intima media wall thickness, serum fibrinogen and homocysteine levels in patients with lichen planus.
Methods: Forty-three patients with lichen planus and 43 age, gender and body mass index (BMI) matched healthy controls (from general population without the disease) were included in this study.
Results: Compared to the healthy controls, patients had statistically significant greater mean intima media wall thickness of the common carotid artery. Moreover, a positive correlation was observed between lichen planus and increased serum homocysteine and c-reactive protein levels.
Limitations: The main limitation of this study is the small sample size due to the time limitation and financial constraints.
Conclusion: Early diagnosis of atherosclerosis in patients with lichen planus might afford better prophylaxis, including weight control and/or lipid profile monitoring. Measurement of the mean intima media wall thickness of the common carotid artery by duplex high-resolution B-mode ultrasound scanning could be beneficial as a valuable method for early diagnosis of atherosclerosis in lichen planus.
Introduction
Lichen planus is an idiopathic inflammatory skin condition, characterized by itchy, small, polygonal, flat-topped pink or purple lesions on the arms and legs. Other parts of the body may also be involved, including the mouth, nails, scalp, vulva, vagina and penis. Involvement of the scalp can result in hair loss, sometimes permanent.
Although its etiology remains unknown, it is believed that lichen planus represents a T-cell-mediated inflammatory disorder. Psoriasis is associated with an increased risk of cardiovascular diseases, metabolic syndrome and dyslipidemia. Being similar to psoriasis, it is possible that lichen planus may also be associated with such a risk, as a result of chronic inflammatory disease.[1],[2],[3]
Homocysteine is an amino acid in the body and an essential amino acid present in foods regularly consumed within the diet.[4] Hyperhomocysteinemia has been regarded a risk factor for atherosclerosis and cardiovascular diseases.[5] It has been seen as an independent risk factor for cardiovascular disease in adults.[6],[7] An increase of 5 μmol/L of homocysteine in serum was associated with a significant increased risk of ischemic heart disease, thromboembolism and stroke. A small number of studies have shown that homocysteine was increased in patients with lichen planus.[8],[9]
Fibrinogen is a circulating glycoprotein involved in wound-healing, thrombosis, platelet aggregation and inflammation which also plays a role in cell adhesion, vasoconstriction and chemotactic activity.[10] Increased plasma fibrinogen levels are also associated with increased risk of myocardial infarction, stroke and vascular mortality.[11] Increasing evidence from epidemiological studies suggests that elevated plasma fibrinogen levels may promote a prothrombotic or hypercoagulable state and are associated with an increased risk of cardiovascular disorders.[12]
Past studies performed by high-resolution B-mode ultrasound imaging indicate that the increase in intima-media wall thickness of common carotid arteries may be associated with higher prevalence of coronary heart disease. Therefore, an increased intima-media wall thickness can be considered as an indicator of generalized atherosclerosis.[3],[13]
In this study, we evaluated the potential association between subclinical atherosclerosis and lichen planus. We measured mean intima-media wall thickness of common carotid artery and serum fibrinogen and homocysteine in patients with lichen planus and compared them with those in sex- and age-matched controls.
Methods
A total of 43 consecutive patients with lichen planus presenting to dermatology clinic completed study examinations and follow-up; 43 age, gender and body mass index-matched controls were also included in this study. The controls were selected amongst companions of patients with cosmetic problems who were attending the dermatology clinic, and without any known dermatologic disease. The matching algorithm for age is as follows: the frequency of controls in each 5-year interval equalizes to the number of patients on it. In addition, the total P value for age is 0.26 [reported in [Table - 1]] which is not statistically significant. Participants were ≥18 years. The diagnosis of lichen planus was based on clinical findings and confirmed by biopsy. Participants were recruited from Shohada-e-Tajrish Hospital of Shahid Beheshti University of Medical Sciences, Tehran, Iran, between January 2014 and January 2015. The institutional ethics committee approved the study protocol which was formulated as per the Declaration of Helsinki. The inclusion criteria were the presence of lichen planus affecting the skin or mucosa and the participants signing an informed consent before participation. The exclusion criteria were as follows:
Patients with: lichenoid drug eruption, receiving lichen planus treatment such as systemic corticosteroids, retinoids or methotrexate, pregnancy, collagen vascular disease, hypothyroidism, malignancy, systemic or hormonal drug intake during the previous 6 months, eating disorders, neurologic diseases, polycystic ovary syndrome and other gynecologic diseases, a serum creatinine level ≥1.5 mg/dL and hypercoagulability states.
Clinical and laboratory measurements
Height and weight were measured. Body mass index was calculated using the following formula: weight (kg)/height (m2). Abdominal circumference and systolic and diastolic blood pressures were measured after a 10-min rest.
Serum total cholesterol, triglycerides, high-density lipoprotein, low-density lipoprotein, fasting blood glucose, high-sensitivity c-reactive protein and homocysteine and fibrinogen levels were studied in samples drawn between 8 and 9 a.m., after a 12-h fasting period.
Data was gathered on smoking, alcohol consumption and personal or family history of cardiovascular disease. The presence of metabolic syndrome was determined according to adult treatment plan-III criteria if three or more of the five following criteria were present:[14] abdominal circumference >102 cm in men and >88 cm in women; hypertriglyceridemia >150 mg/dL, high-density lipoprotein cholesterol >40 mg/dL in men and >50 mg/dL in women, blood pressure >130/85 mm Hg or glucose levels >110 mg/dL. The presence of dyslipidemia was defined by the following parameters: triglycerides >150 mg/dL, total cholesterol >200 mg/dL and low-density lipoprotein cholesterol >130 mg/dL.
Serum homocysteine and fibrinogen levels were studied by enzyme-linked immunosorbent assay technique.
Ultrasound measurement of the mean intima-media wall thickness of common carotid artery
An ultrasound specialist scanned the right common carotid artery. Patients were lying in a supine position during examination, and common carotid arteries were scanned longitudinally. A magnified image was recorded from the angle showing the greatest distance between the interface of lumen–intima and media–adventitia. From this offline image, at least three measurements of the common carotid artery wall were taken approximately 10 mm proximal to the bifurcation (the arterial segment 1 cm proximal to the carotid bulb) to derive mean intima-media wall thickness of common carotid artery. Ultrasound scanning was performed using carotid duplex high-resolution B-mode equipment (Ultrasound, Diagnostic, Samsung Medison, Sonoace X8, Gyeonggi-do, South Korea) with a 12-MHz linear-array transducer (axial resolution of at least 0.3 mm). The final intima-media wall thickness value represents an average of the intima-media wall thickness results from three different points on the right side. Plaque was assumed as a localized thickening >1.2 mm that did not uniformly involve the whole artery. A carotid intima-media wall thickness value >0.8 mm was also considered as an index of subclinical atherosclerosis. The reproducibility of intima-media wall thickness and plaque detection has been well documented.[15] To measure the cross-sectional diameter of common carotid arteries, the ultrasound specialist calculated the intima–intima distance between two sides of the artery in the recorded image.
Statistical methods
Continuous variables are expressed as mean ± standard deviation or as medians with total and interquartile ranges (25th to 75th percentiles). Categorical data were reported as numbers (percentages). Shapiro–Wilk's W-test was used to examine the normality assumption of continuous variables.
Chi-square test and Fisher's exact test, wherever appropriate, were performed for data analysis. Mann–Whitney U-test was used for comparison between serum triglycerides, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein/high-density lipoprotein ratio, fasting blood glucose, c-reactive protein, homocysteine and fibrinogen levels and mean intima-media wall thickness of common carotid artery of the two groups.
Spearman's correlation test was used to assess the association between mean intima-media wall thickness and other continuous variables.
Statistical analyses were performed using the statistical software JMP, version 7 (SAS Institute Inc., Cary, NC, USA; 1989–2007). P values < 0.05 were considered statistically significant. All tests were two-sided.
Results
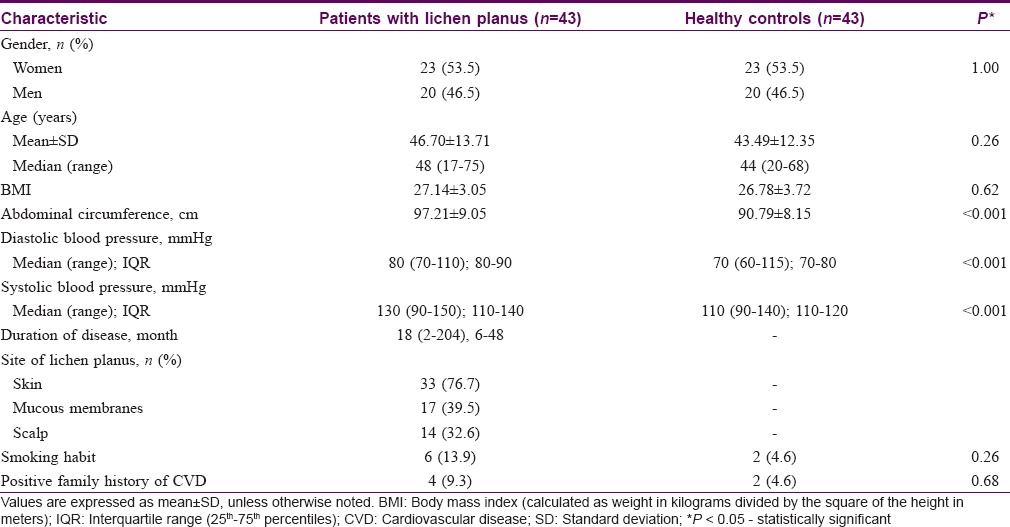
A total of 43 patients with lichen planus and 43 healthy control subjects (who do not have lichen planus) matched for age, gender and body mass index were recruited in this study. The demographics and baseline clinical characteristics of the two groups are summarized in [Table - 1]. The two groups did not differ significantly on age, gender, body mass index, positive family history of cardiovascular disease and self-reported smoking habits [Table - 1]. The severity in all lichen planus subtypes constitutes a wide range from limited to generalized involvement; from early stage of limited inflammation to cicatricial follicular involvement and from reticular non-erosive type to ulcerative mucosal involvement. The analysis of the association between different subtypes and severity of lichen planus with parameters of this study was not performed due to the small sample size.
The median abdominal circumference and diastolic and systolic blood pressures were significantly higher in patients with lichen planus in comparison to control individuals [Table - 1]. Laboratory findings and mean intima-media wall thickness of common carotid artery of the two groups are presented in [Table - 2]. Patients had significantly higher serum triglycerides, total cholesterol, low-density lipoprotein, high-density lipoprotein, low-density lipoprotein/high-density lipoprotein ratio and fasting blood glucose level as compared to controls [Table - 2].

In all, 22 patients with lichen planus (51.2%) and 11 controls (25.6%) had metabolic syndrome. This condition was significantly more frequent in patients than in controls (P < 0.001). In addition, dyslipidemia was observed in 35 patients with lichen planus (81.4%) and 6 controls (13.9%), the difference between the two groups being significant (P < 0. 001).
Compared with controls, patients had significantly higher serum levels of c-reactive protein [Figure - 1], [Table - 2] and homocysteine [both P = 0.02, [Table - 2]. However, the two groups did not differ significantly in median serum level of fibrinogen [P = 0.67, [Table - 2].
 |
| Figure 1: Box plot of serum c-reactive protein (mg/dL) concentrations in patients with lichen planus and healthy controls. Middle point: median; box: interquartile range (25–75 percentiles); whisker: range (excluding outliers). The median, interquartile box and whisker range of patients are greater than their equivalents in controls. As a result, there is a statistically significant difference between the two groups in terms of serum c-reactive protein level and considering the confidence interval of this marker in the patients' group is significantly higher |
The median serum c-reactive protein level was significantly higher in patients with dyslipidemia than in patients without dyslipidemia [P = 0.01 and [Table - 3]. However, there was no significant difference in median serum homocysteine and fibrinogen levels of patients with and without dyslipidemia [P = 0.86 and P = 0.91, respectively; [Table - 3].
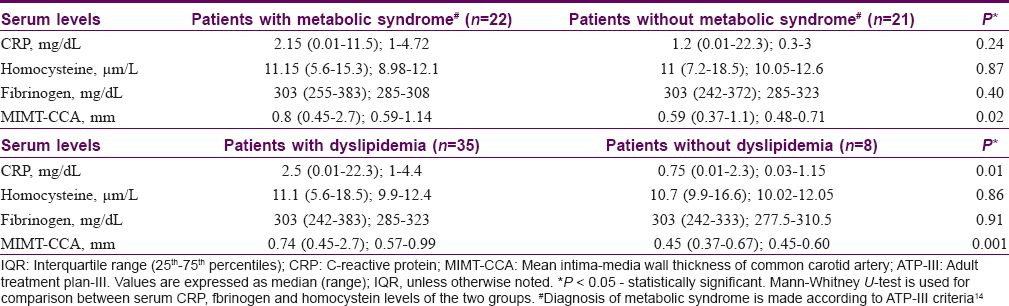
No significant difference was found in median serum c-reactive protein and homocysteine and fibrinogen levels of patients with and without metabolic syndrome [P = 0.24, P = 0.87 and P = 0.40, respectively; [Table - 3].
Intima-media wall thickness
Patients had significantly greater mean intima-media wall thickness of common carotid artery as compared to controls [P < 0.001, [Table - 2] and [Figure - 2].
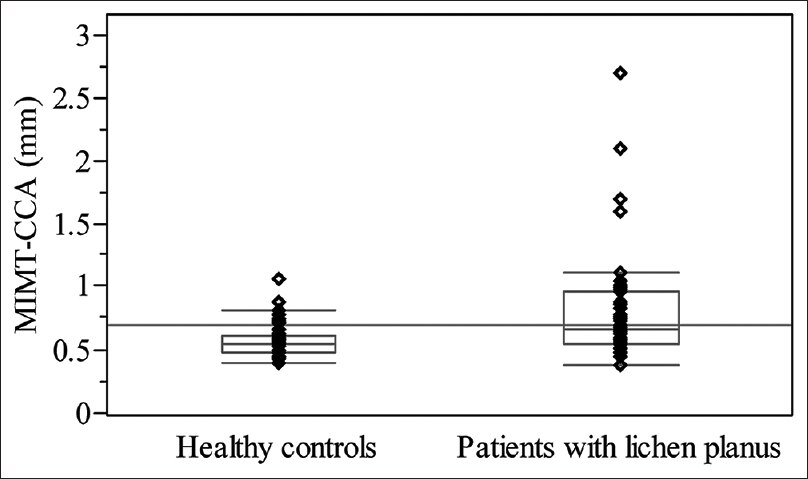 |
| Figure 2: Mean intima-media wall thickness of common carotid artery in patients with lichen planus and healthy controls. Middle point: median; box: interquartile range (25–75 percentiles); whisker: range (excluding outliers). The median, interquartile box and whisker range of patients are greater than their equivalents in controls. As a result, there is a statistically significant difference between the two groups in terms of mean intima-media wall thickness of common carotid artery and the confidence interval of this marker in the patients' group is significantly higher |
The median mean intima-media wall thickness of common carotid artery was significantly higher in patients with lichen planus with metabolic syndrome in comparison to patients without metabolic syndrome [P = 0.02 and [Table - 3].
In addition, the median mean intima-media wall thickness of common carotid artery was significantly higher in patients with lichen planus with dyslipidemia compared with that of patients without dyslipidemia [P = 0.001 and [Table - 3].
According to the results of covariance analysis, there was no significant difference in the mean intima-media wall thickness of common carotid artery of the two groups after adjusting for age, systolic blood pressure and fasting blood glucose levels of subjects (P = 0.19).
Fifteen patients with lichen planus (34.9%) and three controls (7%) had subclinical atherosclerosis (mean intima-media wall thickness of common carotid artery ≥0.8 mm), representing a significant difference between the two groups (P = 0.002).
Correlation between serum c-reactive protein, homocysteine and fibrinogen levels in patients with lichen planus
A positive correlation was observed between serum homocysteine and serum c-reactive protein levels (r = 0.31, P = 0.046). However, no significant association was observed between serum c-reactive protein and homocysteine levels with serum fibrinogen levels in patients (r = 0.18, P = 0.26 and r = 0.04, P = 0.78, respectively).
Discussion
Lichen planus is a chronic inflammatory mucocutaneous disease of unknown etiology and may be caused by a cell-mediated immunological response. When inflammation becomes chronic, the changes in lipid profile become sustained and thereby augment the accumulation of cholesterol in cells and formation of lipid foam cells which, in turn, produce fatty streaks in the arterial walls. This increases the chance of occurrence of atherosclerotic plaques, which may lead to symptomatic cardiovascular disease in such patients.
Recent studies have documented dyslipidemia and increased cardiovascular risk factors in patients with lichen palnus.[16],[17] Previous reports showed that increased high-sensitivity c-reactive protein, insulin resistance, dyslipidemia, obesity and hypertension play an important role in the pathogenesis of atherosclerosis and cardiovascular disease.[18] Our results showed that patients with lichen planus had a significantly abnormal lipid profile, and a high association with obesity and metabolic syndrome compared with controls, which was consistent with previous studies.
Previously, significantly elevated serum homocysteine, fibrinogen and high-sensitivity c-reactive protein have been reported in patients with lichen planus.[8],[9] Our results also showed that there was a significant increase in serum high-sensitivity c-reactive protein and homocysteine levels in patients with lichen planus, but there was no significant difference in fibrinogen levels between cases and controls. Plasma fibrinogen is an important component of the coagulation cascade, and elevated plasma fibrinogen levels are associated with an increased risk of cardiovascular disorders, including ischemic heart disease, stroke and other thromboembolisms.[12] Although some studies have shown a relationship between elevated plasma fibrinogen levels and lichen planus, our study did not throw up any such findings.[9],[16]
Homocysteine is known to have proatherogenic and prothrombotic effects mediated through adverse effects on platelet, endothelial and smooth muscle cell function.[19] It has been demonstrated that homocysteine may have permissive role in endothelial damage of coronary artery mediated by increasing oxidative stress.[20] Similar to findings in previous studies, serum levels of homocysteine were significantly higher in patients than in controls in our study. Previous studies mentioned that homocysteine is an independent predictor of atherosclerotic events and of carotid intimal-media thickness in hyperlipidemic subjects.[21] However, our results showed that homocysteine levels were not significantly associated with increased intima-media wall thickness of common carotid artery in either cases or controls. However, homocysteine was increased in patients with lichen planus and could be a predictor of cardiovascular disease.
Similar findings have been reported in other inflammatory skin diseases such as psoriasis which show higher serum levels of inflammatory cardiovascular indicators, metabolic syndrome parameters and higher range of mean intima-media wall thickness of common carotid artery.[3],[22],[23]
We found some previous studies that evaluated subclinical atherosclerosis in patients with lichen planus and showed, similar to this study, that mean intima-media wall thickness of common carotid artery is significantly elevated in lichen planus compared with the controls.[24],[25]
Our cross-sectional single-center study has some notable limitations. The main limitation is the small sample size, which, in turn, makes it statistically infeasible to assess the association between different subtypes of lichen planus, severity and duration of disease and cardiovascular risk. Future multicenter studies with a larger sample size are needed to more definitively determine the associations between lichen planus and atherosclerosis.
Finally, early diagnosis of atherosclerosis in patients with lichen planus may afford better prophylaxis, including weight control and/or lipid profile monitoring. Measurement of the mean intima-media wall thickness of common carotid artery by duplex high-resolution B-mode ultrasound scanning could be beneficial as a valuable method for early diagnosis of atherosclerosis in lichen planus.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Skin Research Center, Department of Dermatology, Shohada-e-Tajrish Hospital, Tehran, Iran.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ruiz-Carrascosa JC, Arias-Santiago S. Psoriasis and metabolic syndrome. Piel 2010;25:133-45.
[Google Scholar]
|
| 2. |
Gisondi P, Tessari G, Conti A, Piaserico S, Schianchi S, Peserico A, et al. Prevalence of metabolic syndrome in patients with psoriasis: A hospital-based case-control study. Br J Dermatol 2007;157:68-73.
[Google Scholar]
|
| 3. |
Robati RM, Partovi-Kia M, Haghighatkhah HR, Younespour S, Abdollahimajd F. Increased serum leptin and resistin levels and increased carotid intima-media wall thickness in patients with psoriasis: Is psoriasis associated with atherosclerosis? J Am Acad Dermatol 2014;71:642-8.
[Google Scholar]
|
| 4. |
Wierzbicki AS. Homocysteine and cardiovascular disease: A review of the evidence. Diab Vasc Dis Res 2007;4:143-50.
[Google Scholar]
|
| 5. |
Hodeib AA, Elsharawy TA, Fawzi HA. Assessment of serum homocysteine, endothelin-1, and nitric oxide levels in Behçet's disease. Indian J Dermatol 2010;55:215-20.
[Google Scholar]
|
| 6. |
Ozkan Y, Yardim-Akaydin S, Imren E, Torun M, Simşek B. Increased plasma homocysteine and allantoin levels in coronary artery disease: Possible link between homocysteine and uric acid oxidation. Acta Cardiol 2006;61:432-9.
[Google Scholar]
|
| 7. |
Nygård O, Nordrehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE, et al. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med 1997;337:230-6.
[Google Scholar]
|
| 8. |
Kawada T. Blood homocysteine level in patients with oral lichen planus. J Formos Med Assoc 2015;114:789.
[Google Scholar]
|
| 9. |
Saleh N, Samir N, Megahed H, Farid E. Homocysteine and other cardiovascular risk factors in patients with lichen planus. J Eur Acad Dermatol Venereol 2014;28:1507-13.
[Google Scholar]
|
| 10. |
Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 1999;340:448-54.
[Google Scholar]
|
| 11. |
Fibrinogen Studies Collaboration; Danesh J, Lewington S, Thompson SG, Lowe GD, Collins R, et al. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: An individual participant meta-analysis. JAMA 2005;294:1799-809.
[Google Scholar]
|
| 12. |
Kamath S, Lip GY. Fibrinogen: Biochemistry, epidemiology and determinants. QJM 2003;96:711-29.
[Google Scholar]
|
| 13. |
Craven TE, Ryu JE, Espeland MA, Kahl FR, McKinney WM, Toole JF, et al. Evaluation of the associations between carotid artery atherosclerosis and coronary artery stenosis. A case-control study. Circulation 1990;82:1230-42.
[Google Scholar]
|
| 14. |
Adult Treatment Plan III. Executive summary on the third report of the national cholesterol education program (NECP). Expert panel on detection, evaluation and treatment of high blood cholesterol in adults. JAMA 2001;285:2486-97.
[Google Scholar]
|
| 15. |
Roman MJ, Shanker BA, Davis A, Lockshin MD, Sammaritano L, Simantov R, et al. Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. N Engl J Med 2003;349:2399-406.
[Google Scholar]
|
| 16. |
Arias-Santiago S, Buendía-Eisman A, Aneiros-Fernández J, Girón-Prieto MS, Gutiérrez-Salmerón MT, Mellado VG, et al. Cardiovascular risk factors in patients with lichen planus. Am J Med 2011;124:543-8.
[Google Scholar]
|
| 17. |
Dreiher J, Shapiro J, Cohen AD. Lichen planus and dyslipidaemia: A case-control study. Br J Dermatol 2009;161:626-9.
[Google Scholar]
|
| 18. |
Fernández-Real JM, Ricart W. Insulin resistance and chronic cardiovascular inflammatory syndrome. Endocr Rev 2003;24:278-301.
[Google Scholar]
|
| 19. |
Mallika V, Goswami B, Rajappa M. Atherosclerosis pathophysiology and the role of novel risk factors: A clinicobiochemical perspective. Angiology 2007;58:513-22.
[Google Scholar]
|
| 20. |
Nasir K, Tsai M, Rosen BD, Fernandes V, Bluemke DA, Folsom AR, et al. Elevated homocysteine is associated with reduced regional left ventricular function: The multi-ethnic study of atherosclerosis. Circulation 2007;115:180-7.
[Google Scholar]
|
| 21. |
Refsum H, Ueland PM, Nygård O, Vollset SE. Homocysteine and cardiovascular disease. Annu Rev Med 1998;49:31-62.
[Google Scholar]
|
| 22. |
Malekzad F, Robati RM, Abaei H, Hejazi S, Ayatollahi A, Younespour S. Insulin resistance in psoriasis: A case-control study. Iran J Dermatol 2011;14:136-9.
[Google Scholar]
|
| 23. |
Robati RM, Partovi-Kia M, Sadat-Amini H, Haghighatkhah HR, Younespour S, Toossi P, et al. Serum osteopontin level and common carotid artery intima-media wall thickness in psoriasis. Int J Dermatol 2016;55:e262-7.
[Google Scholar]
|
| 24. |
Koseoglu C, Erdogan M, Klu G, Kurmus O, Ertem AG, Efe TH, et al. The relationship between lichen planus and carotid intima media thickness. Acta Cardiol Sin 2016;32:738-43.
[Google Scholar]
|
| 25. |
Aksu F, Karadag AS, Caliskan M, Uzuncakmak TK, Keles N, Ozlu E, et al. Does lichen planus cause increased carotid intima-media thickness and impaired endothelial function? Can J Cardiol 2016;828:4-7.
[Google Scholar]
|
Fulltext Views
4,033
PDF downloads
1,543





