Translate this page into:
Bilateral agminated skin-colored papules and nodules on the dorsum of the hands
2 Department of Dermatology, Royal Infirmary of Edinburgh, Edinburgh, UK
3 Department of Dermatology, University of Edinburgh, Edinburgh, UK
4 Department of Pathology, Western General Hospital and University of Edinburgh, Edinburgh, UK
Correspondence Address:
Asok Biswas
Department of Pathology, Western General Hospital and University of Edinburgh, Crewe Road, Edinburgh EH4 2XU
UK
| How to cite this article: Ayele A, Kravvas G, Weller RB, Biswas A. Bilateral agminated skin-colored papules and nodules on the dorsum of the hands. Indian J Dermatol Venereol Leprol 2019;85:192-194 |
A 63-year-old Caucasian man presented with multiple asymptomatic papules and nodules clustered on the dorsum of both hands. It started 2.5 years ago as a single papule with more lesions developing subsequently on the dorsal aspect of the right (two lesions) and left (three lesions) hands. On examination, they ranged from 7 to 14 mm in diameter. Individual lesions were soft, mobile, skin-colored with a slightly violaceous hue [Figure - 1]a and [Figure - 1]b. Hair, nail and mucosae were spared. Clinically, erythema elevatum diutinum was suspected.
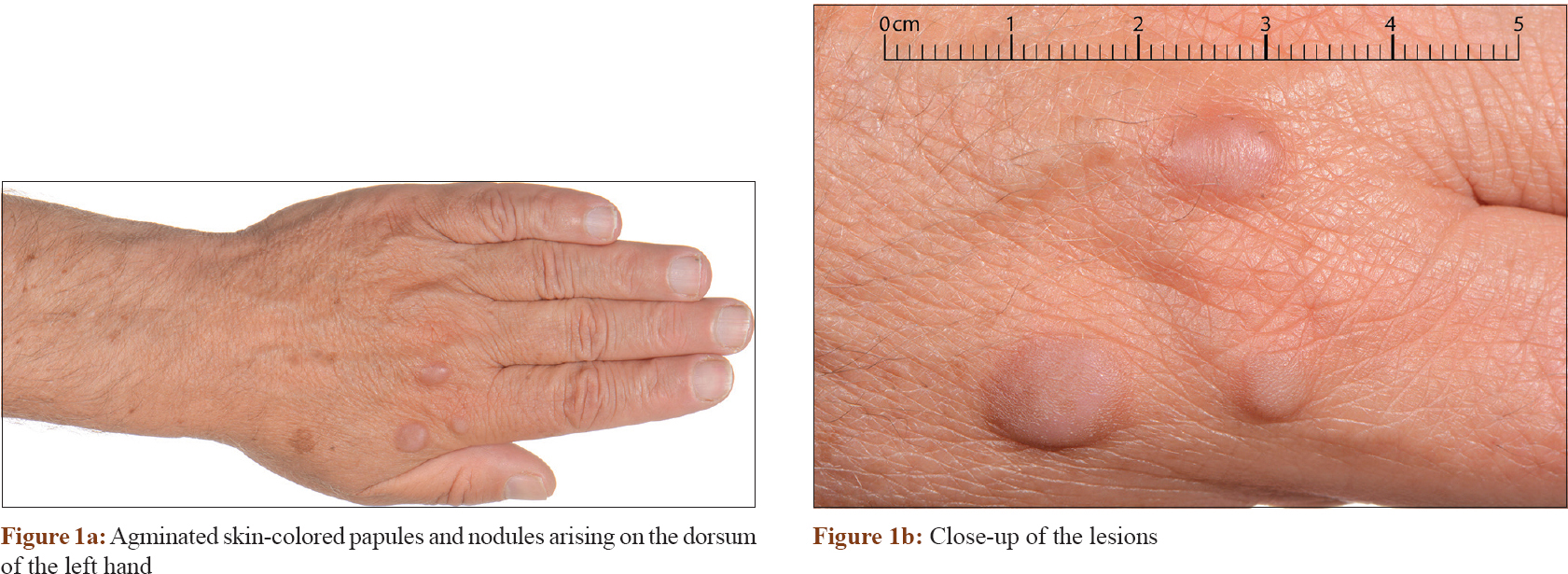 |
| Figure 1: |
An incisional biopsy from one of the nodules showed mild verrucous epidermal hyperplasia and a poorly defined pandermal proliferation of small blood vessels lined by plump endothelial cells, accompanied by fibrosis, spindle cells, and scattered multinucleated giant cells. The latter were irregular and bizarre shaped having scalloped or angular margins, containing multiple nuclei which were either closely aggregated or arranged peripherally in a ring-like fashion [Figure - 2]a and [Figure - 2]b. A mild perivascular infiltrate of lymphocytes, plasma cells, and mast cells was present. Immunohistochemical stains for dermal dendritic cells (factor XIIIa) highlighted the spindle cells but the multinucleated cells (arrows) remained unstained [Figure - 2]c. The macrophage marker CD68 stained the mononuclear and scattered multinucleated cells [Figure - 2]d.
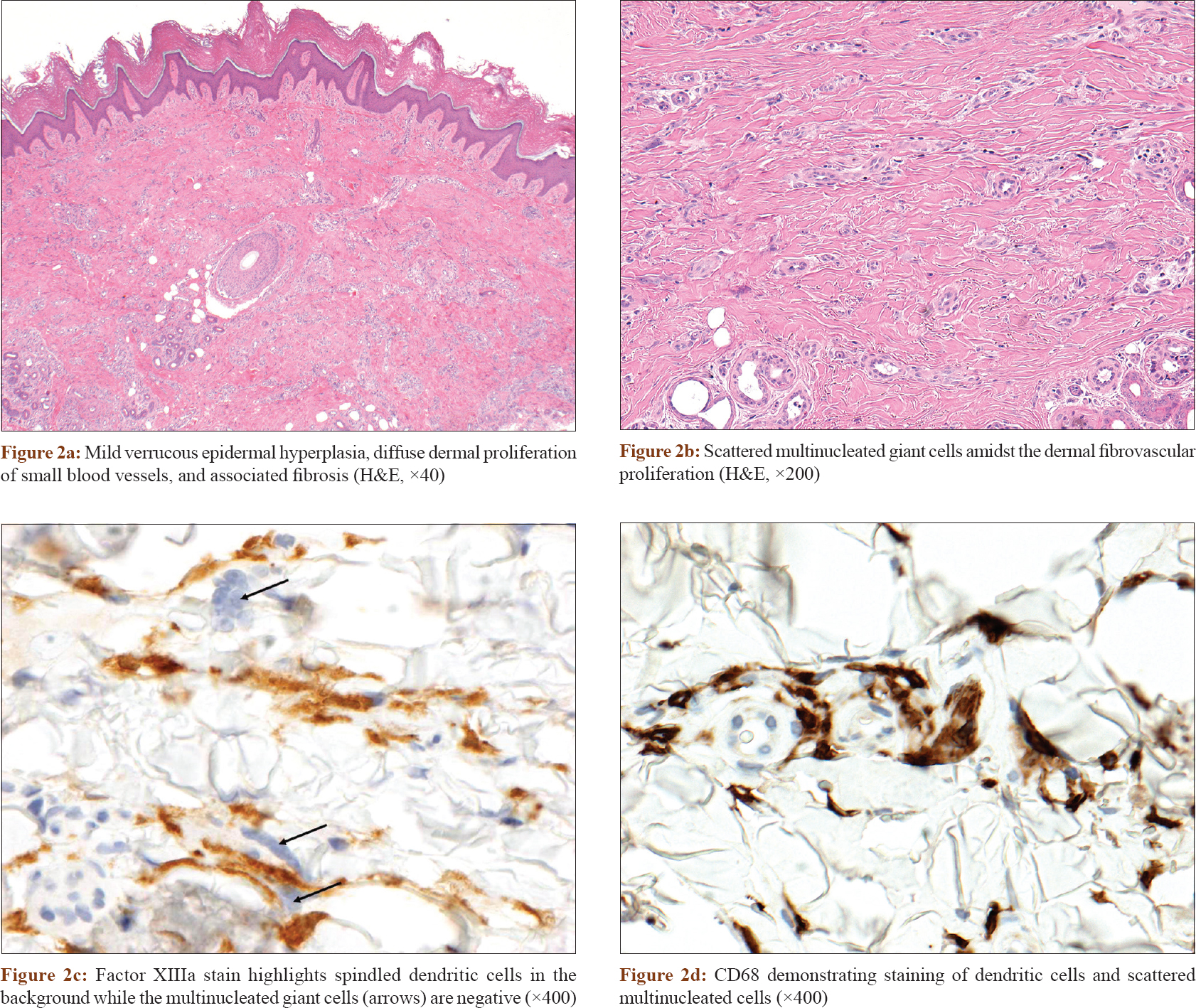 |
| Figure 2: |
What is Your Diagnosis?
Diagnosis
Multinucleate cell angiohistiocytoma.
Discussion
Multinucleate cell angiohistiocytoma is an uncommon entity with a distincte clinical and histopathologic appearance. First described by Smith and Wilson Jones in 1985,[1] barely 150 cases of multinucleate cell angiohistiocytoma have been reported till date.[2]
It has a strong female predilection (female:male ratio of 3:1), affecting middle-aged and elderly women. Classically, it presents as slightly reddish, pink or violaceous elevated, dome-shaped or flat-topped papules or nodules. These lesions tend to be grouped over a particular anatomical area predominantly involving the dorsal aspect of the hands, wrists, thighs, and legs. In rare cases, they may involve the mucosa or assume a disseminated or generalized distribution. The lesions tend to be asymptomatic, progress very slowly and persist indefinitely although spontaneous regression may occur in 10% of cases.[3] Clinical differential diagnoses of this condition include Kaposi's sarcoma, acroangiodermatitis, arthropod bites and erythema elevatum diutinum. A skin biopsy is essential for a definitive diagnosis.
Histopathologically, the lesions are characterized by proliferation of capillaries, venules, and small arterioles mainly affecting the upper and mid-dermis. These blood vessels are embedded in fibrotic dermal connective tissue which contain scattered multinucleated giant cells often having irregular, bizarre shapes with scalloped or angular margins. Isolated spindled cells accompany the distinctive multinucleated giant cells. There is also sparse perivascular and interstitial infiltrate containing plasma cells, lymphocytes, neutrophils and almost invariably, large number of mast cells. The immunophenotype is variable but nearly half of the reported cases have shown factor XIIIa positivity and variable CD68 reactivity in the multinucleated giant cells.[2] Other fibromatous and angiomatous proliferations like atrophic vascular dermatofibroma (denser dendritic cell proliferation in whorled or storiform pattern along with thinned dermis) and fibrous papule of the face (telangiectasia of existing blood vessels surrounded by lamellar collagen rather than actual vascular proliferation) may resemble this condition histopathologically.[4]
Multinucleate cell angiohistiocytoma may be a reactive condition or a true neoplasm; exact pathogenesis is still unclear. Some authors have stressed on the putative role of estrogen receptor α, dermal dendritic cells, and mast cells. It is being increasingly speculated that multinucleate cell angiohistiocytomas and dermatofibromas are closely related dermal dendritic cell proliferations. Unlike dermatofibromas, this condition tends to show an agminated or multifocal clinical distribution.[5]
Given the slow progression and indolent behavior, treatment is not always necessary. They may be surgically excised without any significant risk of local recurrence, if cosmetically unacceptable. Other treatment modalities which have been reported to be effective include argon laser therapy, cryotherapy, intense pulse light, and potentially antihormonal therapy.[6]
Despite the characteristic clinical appearance, histology and distribution, this disorder is rarely considered clinically due to lack of awareness about this entity. Both clinicians and pathologists should be familiar with this entity to reassure affected patients and increase awareness about this unusual condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Smith N, Wilson Jones E. Multinucleate cell angiohistiocytoma: A new entity. Br J Dermatol 1985;113:15.
[Google Scholar]
|
| 2. |
Frew JW. Multinucleate cell angiohistiocytoma: Clinicopathological correlation of 142 cases with insights into etiology and pathogenesis. Am J Dermatopathol 2015;37:222-8.
[Google Scholar]
|
| 3. |
Pérez LP, Zulaica A, Rodríguez L, Campo MC, Peñaranda JM, Fernández-Redondo V, et al. Multinucleate cell angiohistiocytoma. Report of five cases. J Cutan Pathol 2006;33:349-52.
[Google Scholar]
|
| 4. |
Puig L, Fernández-Figueras MT, Bielsa I, Lloveras B, Alomar A. Multinucleate cell angiohistiocytoma: A fibrohistiocytic proliferation with increased mast cell numbers and vascular hyperplasia. J Cutan Pathol 2002;29:232-7.
[Google Scholar]
|
| 5. |
McCalmont TH. Everything you wanted to know about dermatofibroma but were afraid to ask. J Cutan Pathol 2014;41:5-8.
[Google Scholar]
|
| 6. |
Cesinaro AM, Roncati L, Maiorana A. Estrogen receptor alpha overexpression in multinucleate cell angiohistiocytoma: New insights into the pathogenesis of a reactive process. Am J Dermatopathol 2010;32:655-9.
[Google Scholar]
|
Fulltext Views
4,770
PDF downloads
2,694





