Translate this page into:
Predictors of serological cure after treatment in patients with early syphilis: A retrospective observational study in Thailand
2 Bamrasnaradura Infectious Diseases Institute, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand
Correspondence Address:
Charussri Leeyaphan
Department of Dermatology, Faculty of Medicine, Siriraj Hospital, Mahidol University, 2 Wanglang Road, Bangkok 10700
Thailand
| How to cite this article: Leeyaphan C, Punyaratabandhu P, Jiamton S, Junsuwan N, Chirachanakul P, Chanyachailert P, Omcharoen V. Predictors of serological cure after treatment in patients with early syphilis: A retrospective observational study in Thailand. Indian J Dermatol Venereol Leprol 2019;85:235 |
Abstract
Background: Some patients with early syphilis who receive appropriate treatment do not reach a serological cure and have a persistent titer which does not meet the criteria for treatment failure (serofast state).
Aims: This retrospective study aimed to determine the prevalence of serological cure and the serofast state as well as the factors associated with serological cure after treatment of patients with early syphilis.
Methods: A serological cure was defined as occurring when there was a ≥4-fold decrease in nontreponemal titer, whereas patients with a ≥4-fold increase were considered as having either a treatment failure or reinfection. Nontreponemal titers that neither increased nor decreased ≥4-fold after treatment were considered to be in a serofast state. Seroreversion was defined as occurring when there was a negative test within 12 months of treatment.
Results: There were 179 patients with a mean age of 31.9 years; 174 (97.2%) were men, and 125 (70%) were HIV patients. Of the total, 174 (98%; 95% confidence interval 94.82–99.42%) patients achieved a serological cure, whereas five were in a serofast state 12 months after treatment. Those five serofast patients were all HIV-positive men, of which 4 (80%) had secondary-stage syphilis, a CD4 count ≤200 cells/μl and a titer <1:8. In a bivariate analysis, a serological cure was associated with a baseline Venereal Disease Research Laboratory >1:16 titers (P = 0.018), and a CD4 cell count >200 cells/μl in 6 months preceding treatment (P = 0.016). The median time to a serological cure was 96 days. Only 22 (12.3%) of the patients achieved seroreversion at 12 months after treatment.
Limitations: A retrospective medical record review is likely to have a selection bias, and in our study, 196 (52%) patients were excluded due to missing information.
Conclusions: Most patients with early syphilis who achieved a serological cure at 12 months after treatment had high baseline Venereal Disease Research Laboratory titers and CD4 cell counts. However, only 22 (12.3%) had a negative Venereal Disease Research Laboratory titer after 1 year of treatment.
Introduction
The Centers for Disease Control and Prevention and Thai National Guidelines for syphilis recommend that a nontreponemal test be performed to evaluate the serological response at 3, 6 and 12 months after treatment for early syphilis.[1],[2] In general, patients with nontreponemal titers that decline 4-fold or more within 12 months of treatment are regarded as having a serological cure, whereas those patients with either a <4-fold decrease or increase without reinfection are considered to be in a serofast state.[1] In clinical practice, some patients experience a slow rate of decrease in their serological titers and scarcely achieve a negative titer even with proper treatment.[3],[4],[5],[6] The purpose of this study was to evaluate the prevalence and predicting factors of serological cures after treatment in early syphilis patients.
Methods
Subjects
This was a retrospective review of the medical records of patients diagnosed with early syphilis at a tertiary hospital between January 2011 and December 2015. The study was approved by Institutional Review Boards of the Bamrasnaradura Infectious Diseases Institute, Nonthaburi, and the Faculty of Medicine, Mahidol University, Bangkok, Thailand.
The stages of syphilis were based on the sexually transmitted diseases treatment guidelines of 2015 from the Centers for Disease Control and the Thai National Guidelines.[1],[2] Early syphilis in this study included the primary, secondary and early latent stages of syphilis with <1 year of infection. Primary syphilis presents as genital ulcers (chancre) with or without regional lymphadenopathy, whereas secondary syphilis is characterized by mucocutaneous eruptions with or without generalized lymphadenopathy.
A serological cure is defined as occurring when there is more than a 4-fold decrease in a nontreponemal titer, whereas patients with a ≥4-fold increase are considered as having possible treatment failure or reinfection. Nontreponemal titers that neither increase nor decrease 4-fold after treatment are referred to as being in a serofast state, and seroreversion is defined as occurring when there is a negative test within 12 months of treatment.[7]
The following demographic data were collected: gender, age, sexual orientation, syphilis stage, HIV status, CD4 cell count, laboratory investigations, including Venereal Disease Research Laboratory test titer (B BBL Venereal Disease Research Laboratory antigen test, Becton Dickinson), and Treponema pallidum hemagglutination titer; treatment regimens; and complications. The serial follow-ups of the Venereal Disease Research Laboratory titers at 3, 6, 9 and 12 months were noted. The titers of the period since the onset of symptoms (in other words, the duration between first having signs or symptoms of syphilis, and receiving treatment), as well as any earlier histories of syphilitic infection and treatments before 2011 revealed in the patients' self-reports were also collected for analysis. The treatment regimens prescribed by physicians included intramuscular injections of benzathine penicillin G (2.4 million units, administered either as a one-off dose or as three-weekly doses), oral doxycycline (100 mg twice daily for 14 days) or intravenous ceftriaxone (1 g daily for 10–14 days).
People who had previously achieved a serological cure but subsequently had recurring signs or symptoms of early syphilis and had at least a 4-fold increase in a nontreponemal test titer were considered to be reinfected. All patients who fulfilled the diagnostic criteria of early syphilis used in this study were included. Any missing results of Venereal Disease Research Laboratory tests conducted during the follow-up period and all data from reinfection episodes were excluded from the analysis.
Statistical analysis
A Chi-square test was used to compare differences in the categorical data, and an independent t-test was used for continuous variables. A P value of <0.05 was considered statistically significant. The odds ratio with 95% confidence interval was also calculated for each relevant variable. All analyses were performed using IBM SPSS Statistics for Windows, version 22.0 (IBM Corp., Armonk, NY, USA).
Results
Demographic data and prevalence of serological cure and serofast state
Of the 375 early syphilis cases reviewed, 179 patients had complete data and were therefore included [Figure - 1]. Those patients had a mean age of 31.9 years, with 174 (97.2%) being male; 125 (70%) of the 179 cases were HIV patients, of which 115 (64.1%) were on highly active antiretroviral therapy. In the case of the 174 men, 160 (92%) were men who have sex with men. Most of the patients, 159 (89%), were in the secondary stage of syphilis. A history of syphilitic infection was found in 34 (18.9%) cases. There were no cases of concurrent sexually transmitted infections, other than HIV. Benzathine penicillin G was used to treat 153 (85.5%) patients, and this was followed by doxycycline for 18 (10%) and ceftriaxone for 8 (4.5%) patients [Figure - 1]. Of the 153 patients on benzathine penicillin G treatment, 68 (44.4%) received a single dose while 85 (55.6%) had three doses of benzathine penicillin G weekly. Compliance with the treatment was evaluated, and it revealed 100% adherence. The baseline demographic data and clinical presentations of the two benzathine penicillin G groups were not significantly different, except that a higher proportion of the patients given three-weekly doses of benzathine penicillin G was HIV-infected than those receiving a single dose (83.5 vs 55.9%, with P < 0.001).
 |
| Figure 1: Patient selection criteria used in this study. Abbreviations: BPG single dose: Benzathine penicillin G (2.4 MU, IM), single dose, BPG 3 doses: Benzathine penicillin G (2.4 MU, IM), weekly for 3 weeks, Doxycycline: Doxycycline (100 mg), twice daily for 14 days, Ceftriaxone: Ceftriaxone (1 g, IV), for 10–14 days |
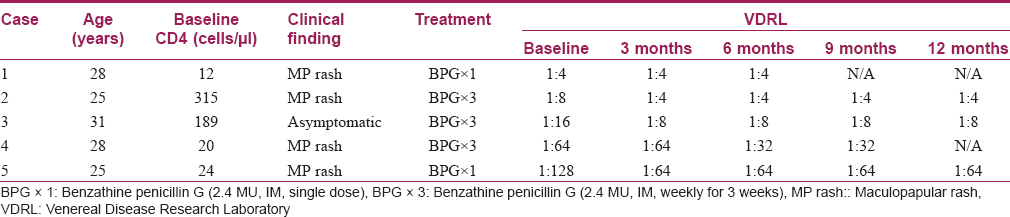
By 6 months after treatment, 139 (77.7%, with 95% confidence interval 71.3–83.4%) patients had achieved a serological cure. That figure increased to 174 (98%, with 95% confidence interval 94.8–99.4%) patients who had achieved a serological cure by 12 months after therapy, with the remaining five patients (2%, with 95% confidence interval 0.6%–5.2%) in a serofast state [Table - 1]. All five serofast patients had been treated with benzathine penicillin G. Four of them had initially been diagnosed as having secondary syphilis due to the presence of a maculopapular rash without other causes; their rashes completely resolved after treatment. Because those five patients had not achieved a serological cure within 12 months of the initial treatment, neurosyphilis was investigated; however, no signs or symptoms of neurosyphilis were detected. In the case of two serofast patients with Venereal Disease Research Laboratory serum titers >1:32, cerebrospinal fluid examinations were performed; they revealed normal results for the cerebrospinal fluid cell count and protein and sugar levels, as well as negative cerebrospinal fluid Venereal Disease Research Laboratory. Three patients received an additional treatment of weekly, intramuscular benzathine penicillin G (2.4 million units) for 3 weeks; they demonstrated a gradual decrease in their titers.
Of the 174 patients who had achieved a serological cure at some point during the 12-month follow-up period, reinfection was found in 32 (18.4%, with 95% CI 13.3%–24.8%) patients; they presented with recurring signs or symptoms, and with a >4-fold increase in titer from their last serological test result. All of them reported having had unprotected sexual intercourse between their last syphilis treatment and the recurring symptoms or signs.
Serological cure and stage of syphilis
In patients with a serological cure, the rate of cure varied with the stage of syphilis. All patients with primary syphilis (6/6) had a serological cure within 6 months of treatment. Moreover, 122 (76.7%) patients with secondary syphilis had a serological cure by 6 months, which increased to 154 (97.4%) by 12 months. Similarly, 11 (78.6%) patients with early latent syphilis had a serological cure by 6 months, with another 2 (14.3%) progressing to a serological cure by 12 months with a total of 13 (92.9%) patients.
Comparing patients with a single benzathine penicillin G dose and those with three-weekly benzathine penicillin G doses, there was no significant difference in their serological cure rates at 6 and 12 months after treatment (P = 0.179 and 1.000, respectively); [Figure - 1].
Predicting factors of serological cure
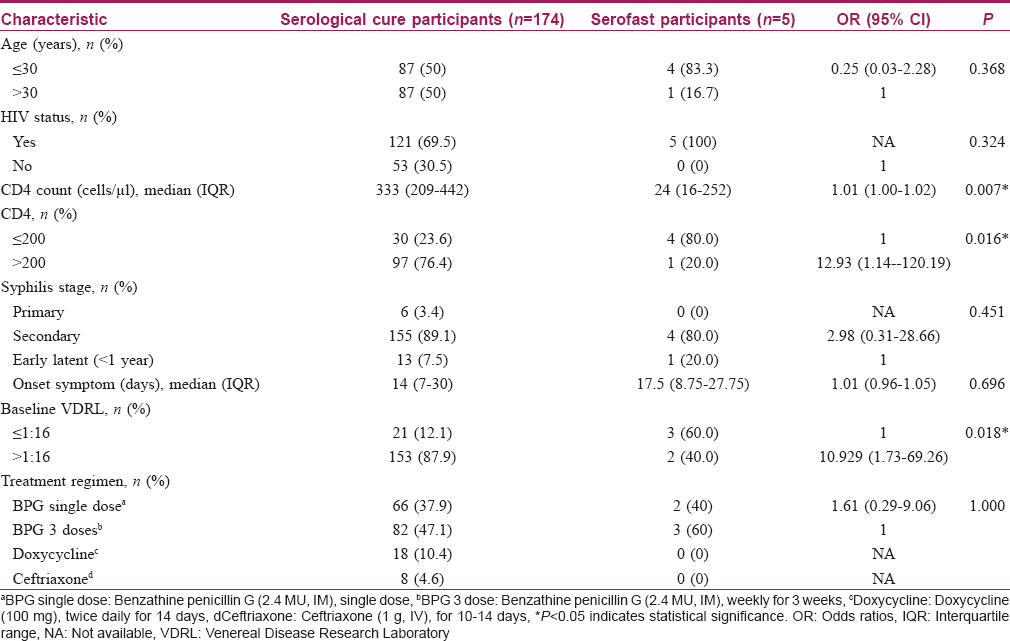
An analysis of 174 patients with a serological cure and five patients in a serofast state demonstrated that a baseline Venereal Disease Research Laboratory titer >1:16 had a higher probability of a serological cure (odds ratio, 10.9 [95% confidence interval 1.7–69.3]). A serological cure was also related to a CD4 count >200 cells/μl in the 6 months preceding treatment (odds ratio, 12.9 [95% confidence interval 1.1–120.2]). In contrast, age, sexual orientation, a history of syphilitic infection, the syphilis stage, HIV status, treatment regimen and the onset of symptoms were not significantly associated with a serological cure [Table - 2].
Median time to serological cure
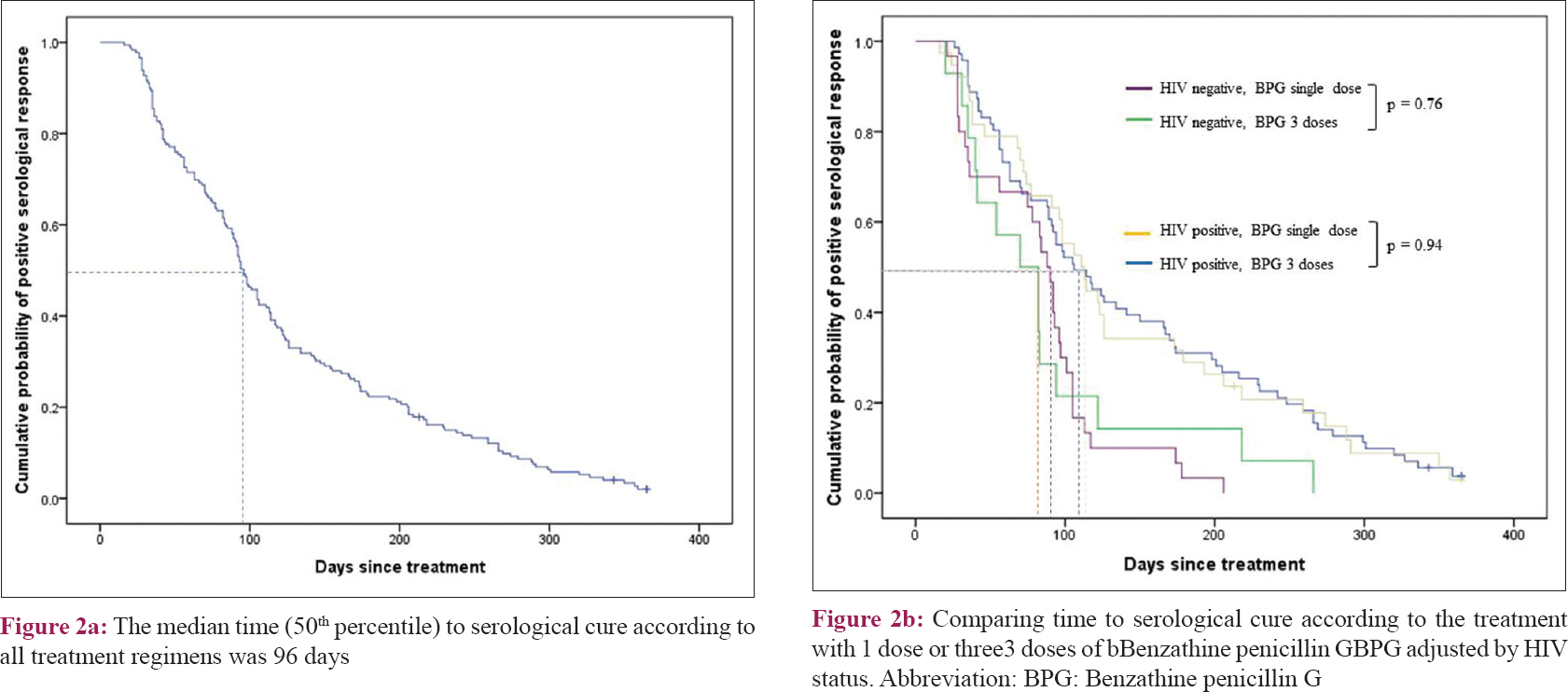
The overall median time to a serological cure for all treatment regimens was 96 (interquartile range 54–173) days, regardless of the treatment regimen [Figure - 2]a. Of the 153 patients treated with benzathine penicillin G, the median time to cure was shorter for the HIV-negative patients than the HIV-positive patients (83 days vs 111 days, respectively; P < 0.001). In addition, the median time to a serological cure was not significantly different for those early syphilis patients treated with a single dose of 2.4 million units of benzathine penicillin G compared to those who received three-weekly, intramuscular doses of benzathine penicillin G (2.4 million units), when adjusted for HIV infection status [Figure - 2]b.
 |
| Figure 2: |
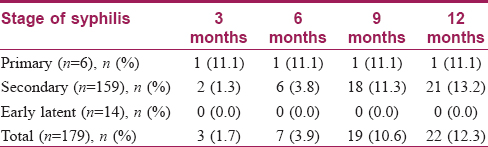
Prevalence and factors of seroreversion
Of the 179 patients, 7 (3.9%) had achieved seroreversion as a negative Venereal Disease Research Laboratory within 6 months of the treatment [Table - 3], and the figure increased to 22 (12.3%) within 12 months of the treatment. The median Venereal Disease Research Laboratory titer for the 152 patients who did not have seroreversion was 1:2 (range, NR–1:32) at 12 months after treatment. The proportion of patients who had seroreversion at 12 months was highest (13.2%; 21/159) for patients with secondary syphilis, and lowest (0%; 0/14) among those with early latent syphilis.
Discussion
This study demonstrated that the vast majority of patients with early syphilis, 174 (98%), achieved a serological cure, while only 6 (2%) were in a serofast state at 12 months after treatment. Having a baseline Venereal Disease Research Laboratory titer >1:16 and a CD4 cell count >200 cells/μl in the 6 months preceding the treatment were associated with a higher probability of a serological cure. The overall median time to a serological cure was 96 days regardless of the treatment regimen given. Only 22 (12.3%) had achieved complete seroreversion by 12 months after the treatment.
Previous reports about the serological cure of HIV-negative patients showed that about 369 (79%) achieved a serological cure within 6 months.[7],[8] Similar to those studies, 139 (77.2%) in the present study achieved a serological cure within 6 months of treatment, and that was despite the fact that 121 (70%) were HIV patients. Furthermore, a previous study demonstrated that 17% of early syphilis patients achieved seroreversion, which is similar to the proportion found in this study of 12.3%.[8] The findings of the present study, therefore, show that a majority of patients who receive appropriate treatment achieve a serological cure but do not subsequently exhibit negative titers at 12 months after treatment.
An earlier study found that 4.3% early syphilis patients presented a serofast state at 12 months after treatment; the current study demonstrated that a slightly lower proportion, 2% patients with early syphilis were in the serofast state at 12 months.[9] Another study also reported that age, gender, stage of infection, lower baseline titers, treatment regimen, cellular immune suppression and disorders, Treponema pallidum occult infection and the subtypes of the Treponema pallidum repeat gene were associated with the serofast state; however, the associations of baseline Venereal Disease Research Laboratory titers and CD4 cell counts remained unclear, and further studies were recommended by the author's of that study.[10],[11]
The management of patients in a serofast state is uncertain. Because those patients in the present study had not achieved a serological cure by 12 months after treatment, neurosyphilis needed to be excluded. On the basis of a study recommendation that a cerebrospinal fluid examination be conducted on asymptomatic HIV-infected patients with a titer >1:32, an examination was performed on the two serofast patients in the current study who had baseline Venereal Disease Research Laboratory serum titers >1:32; the findings were normal.[12]
The present study showed that patients who do not achieve a serological cure at 12 months may have slow serological responses. As those patients may have a benign immune response, long-term follow-up may be essential in order to ensure that there is a serological cure and to detect early complications or treatment failure. Further studies on the most appropriate retreatment may be needed.[1],[3],[13]
Some of the previous studies have reported that factors related to a serological cure in HIV-negative patients are young age, less sex partners, higher baseline rapid plasma regain titers and an early syphilis stage.[7],[14] Similarly, in this study, a serological cure was highly associated with having a baseline Venereal Disease Research Laboratory titer >1:16 and a CD4 cell count >200 cells/μl in the 6 months preceding treatment. Another study also found that a higher baseline rapid plasma regain titer is associated with a serological cure, leading to the hypothesis that a high baseline rapid plasma regain titer may signify a beneficial inflammatory and immune response to T. pallidum, thereby facilitating its clearance.[15]
A number of studies have reported that patients with an HIV infection showed a slower decrease in rapid plasma regain titers after syphilis treatment than HIV-negative patients.[8],[16],[17],[18] This study found no association between HIV infection and serological cure; nevertheless, a high CD4 cell count was found to be related with serological cure. The immune status may be more important in determining the cure rate than the HIV infection status. A low CD4 cell count could lead to dysfunction of antibody formation and thereby result in a less effective immune clearance of T. pallidum in HIV patients.[16],[17] On the contrary, a previous study reported that the CD4 cell count and HIV viral load was not associated with cure.[3] Further studies are important to evaluate the relationship between serological cure and HIV status, including the CD4 cell count and viral load.
In Thailand, as treatment for early syphilis has not been well defined during the past 5 years, treatment has depended on individual physicians' judgments. Consequently, some patients received single doses of benzathine penicillin G, while others had three doses. When the treatment outcomes were analyzed in this study, no significant associations were demonstrated between the dosage of benzathine penicillin G and either the cure rate or the median time to cure, when adjusted for HIV infection status. Moreover, a single dose of benzathine penicillin G has been reported elsewhere to have a similar level of effectiveness to three doses of benzathine penicillin G in the treatment of early syphilis.[19],[20] The results of this study are also in accord with the Centre for Disease Control guidelines, which recommend the administration of a single dose of benzathine penicillin G for patients with early syphilis, regardless of their HIV infection status.[1]
This study had several limitations. First, it dealt mostly with male patients. Only five women (2.9% of all subjects) were included because women with syphilis are usually treated by gynecologists. Consequently, there was insufficient data for the conduct of an analysis to identify any gender differences. In addition, this retrospective medical record review may have a selection bias: 196 (52%) of the potential study population were excluded because the patients' medical records did not contain information related to the 12-month Venereal Disease Research Laboratory follow-up. Also, most patients, 89%, were in the secondary stage. That may have resulted from the patients being aware of the need to visit a doctor due to having generalized mucocutaneous eruptions (in contrast with the painless and self-improving ulcers of primary syphilis, and the asymptomatic early latent syphilis). Status of partner was not collected in this study. Furthermore, the study had only five patients with a serofast state, which limited the ability to detect the associated factors. Lastly, due to the low sensitivity of the Venereal Disease Research Laboratory which this study used for screening, primary syphilis presenting with painless ulcers may have been missed. An IgM enzyme-linked immunosorbent assay for syphilis is an additional screening test to increase sensitivity for diagnosis and treatment monitoring purposes, but it is relatively costly.[13] As a result, the enzyme-linked immunosorbent assay is infrequently used in a resource-limited country like Thailand. Therefore, further prospective studies based on a wider range of population groups, including a larger patient group and a higher proportion of female patients, may be required.
Conclusions
Most early syphilis patients had achieved a serological cure by 12 months after treatment. The serological cures were associated with a baseline Venereal Disease Research Laboratory >1:16 titers and a CD4 cell count >200 cells/μl in the 6 months preceding the treatment. However, only 22 (12.3%) had a negative Venereal Disease Research Laboratory titer at 1 year after treatment.
Acknowledgements
The authors thank Professor Kanokvalai Kulthanan, Chairman of the Department of Dermatology, Siriraj Hospital, for administrative support. We also thank Mr. Suthipol Udompanthurak and Miss. Orawan Supapueng for statistical advice.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015;64:1-37.
[Google Scholar]
|
| 2. |
Kongkrungkaite N, Paiboonsin N. Thailand national guidelines on the management of sexually transmitted infections 2015. In: Kongkrungkaite P, Kittiyaowamarn R, Daengsaard E, editors. Syphilis. 1st ed. Bangkok: Aksorn Graphic and Design Publication; 2015. p. 14-21.
[Google Scholar]
|
| 3. |
Seña AC, Zhang XH, Li T, Zheng HP, Yang B, Yang LG, et al. A systematic review of syphilis serological treatment outcomes in HIV-infected and HIV-uninfected persons: Rethinking the significance of serological non-responsiveness and the serofast state after therapy. BMC Infect Dis 2015;15:479.
[Google Scholar]
|
| 4. |
Tipple C, Taylor GP. Syphilis testing, typing, and treatment follow-up: A new era for an old disease. Curr Opin Infect Dis 2015;28:53-60.
[Google Scholar]
|
| 5. |
Spagnuolo V, Poli A, Galli L, Cernuschi M, Nozza S, Maillard M, et al. Predictors of lack of serological response to syphilis treatment in HIV-infected subjects. J Int AIDS Soc 2014;17:19654.
[Google Scholar]
|
| 6. |
Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: A systematic review. JAMA 2014;312:1905-17.
[Google Scholar]
|
| 7. |
Seña AC, Wolff M, Martin DH, Behets F, Van Damme K, Leone P, et al. Predictors of serological cure and serofast state after treatment in HIV-negative persons with early syphilis. Clin Infect Dis 2011;53:1092-9.
[Google Scholar]
|
| 8. |
Seña AC, Wolff M, Behets F, Martin DH, Leone P, Langley C, et al. Rate of decline in nontreponemal antibody titers and seroreversion after treatment of early syphilis. Sex Transm Dis 2017;44:6-10.
[Google Scholar]
|
| 9. |
Ghanem KG, Erbelding EJ, Wiener ZS, Rompalo AM. Serological response to syphilis treatment in HIV-positive and HIV-negative patients attending sexually transmitted diseases clinics. Sex Transm Infect 2007;83:97-101.
[Google Scholar]
|
| 10. |
Qin J, Yang T, Wang H, Feng T, Liu X. Potential predictors for serofast state after treatment among HIV-negative persons with syphilis in cChina: A systematic review and meta-analysis. Iran J Public Health 2015;44:155-69.
[Google Scholar]
|
| 11. |
Tong ML, Lin LR, Liu GL, Zhang HL, Zeng YL, Zheng WH, et al. Factors associated with serological cure and the serofast state of HIV-negative patients with primary, secondary, latent, and tertiary syphilis. PLoS One 2013;8:e70102.
[Google Scholar]
|
| 12. |
Marra CM, Maxwell CL, Smith SL, Lukehart SA, Rompalo AM, Eaton M, et al. Cerebrospinal fluid abnormalities in patients with syphilis: Association with clinical and laboratory features. J Infect Dis 2004;189:369-76.
[Google Scholar]
|
| 13. |
Knaute DF, Graf N, Lautenschlager S, Weber R, Bosshard PP. Serological response to treatment of syphilis according to disease stage and HIV status. Clin Infect Dis 2012;55:1615-22.
[Google Scholar]
|
| 14. |
Jinno S, Anker B, Kaur P, Bristow CC, Klausner JD. Predictors of serological failure after treatment in HIV-infected patients with early syphilis in the emerging era of universal antiretroviral therapy use. BMC Infect Dis 2013;13:605.
[Google Scholar]
|
| 15. |
Salazar JC, Hazlett KR, Radolf JD. The immune response to infection with treponema pallidum, the stealth pathogen. Microbes Infect 2002;4:1133-40.
[Google Scholar]
|
| 16. |
Moir S, Fauci AS. B cells in HIV infection and disease. Nat Rev Immunol 2009;9:235-45.
[Google Scholar]
|
| 17. |
Lane HC, Masur H, Edgar LC, Whalen G, Rook AH, Fauci AS, et al. Abnormalities of B-cell activation and immunoregulation in patients with the acquired immunodeficiency syndrome. N Engl J Med 1983;309:453-8.
[Google Scholar]
|
| 18. |
Janier M, Chastang C, Spindler E, Strazzi S, Rabian C, Marcelli A, et al. A prospective study of the influence of HIV status on the seroreversion of serological tests for syphilis. Dermatology 1999;198:362-9.
[Google Scholar]
|
| 19. |
Costa-Silva M, Azevedo C, Azevedo F, Lisboa C. Early syphilis treatment in HIV-infected patients: Single dose vs. Three doses of benzathine penicillin G. J Eur Acad Dermatol Venereol 2016;30:1805-9.
[Google Scholar]
|
| 20. |
Andrade R, Rodriguez-Barradas MC, Yasukawa K, Villarreal E, Ross M, Serpa JA, et al. Single dose versus 3 doses of intramuscular benzathine penicillin for early syphilis in HIV: A randomized clinical trial. Clin Infect Dis 2017;64:759-64.
[Google Scholar]
|
Fulltext Views
3,656
PDF downloads
2,590





