Translate this page into:
Recurrent pyogenic granuloma over nevus flammeus
2 Department of Surgery, VMMC, Safdarjung Hospital, New Delhi, India
Correspondence Address:
Fouzia Siraj
National Institute of Pathology, ICMR, Safdarjung Hospital, New Delhi
India
| How to cite this article: Shruti S, Siraj F, Ramesh V, Ramesh V. Recurrent pyogenic granuloma over nevus flammeus. Indian J Dermatol Venereol Leprol 2019;85:236 |
Sir,
Pyogenic granuloma is an acquired reactive vascular proliferation in the skin and oral mucosa, commonly affecting the children and young adults.[1] It has been infrequently reported in association with other vascular abnormalities such as nevus flammeus and vascular hemangiomas, especially after laser therapy.[2] Various vascular neoplasms like capillary hemangiomas, tufted angiomas, and cavernous hemangiomas, have been rarely associated with port-wine stain (PWS), also a type of nevus flammeus.[3] The occurrence of recurrent pyogenic granuloma in association with such vascular lesions is rare. Few of them have arisen in nevus flammeus without any predisposing factor like trauma, laser treatment, or pregnancy.[2] This spontaneous development may be promoted by arteriovenous anastomoses in vascular lesions, especially in the richly vascularized areas like fingers, hands, lips, tongue and face leading to the development ofpyogenic ranuloma.[4] We hereby report an unusual case of spontaneously recurrent pyogenic ranuloma within a nevus flammeus in the absence of any predisposing factor and further discuss their relationship with arteriovenous malformations.
A 26-year-old male presented to us with a single, 2 × 3 cm dark red, dome-shaped pedunculated growth within a congenital, Diffuse pale red patch extending irregularly over the left upper thigh. [Figure - 1]a and [Figure - 1]b. The growth was non-pruritic with occasional episodic spontaneous bleeding. Our presumptive diagnosis was pyogenic granuloma or an infected acrochordon over a nevus flammeus. The lesion recurred two times despite excision. The excised lesion was sent to National Institute of Pathology for histopathology. Microscopic examination showed a vascular lesion surrounded by hyperplastic epithelium with parakeratosis and focal ulceration. Dermis revealed lobules of variably sized capillaries in a fibromyxoid matrix with admixed inflammatory cells. Some vessels were congested and lined by plump endothelial cells [Figure - 2]. A diagnosis of pyogenic granuloma was rendered, which. is a rapidly growing, hypervascular, hemorrhagic lesion that presents as a painless, reddish purple, pedunculated, or sessile mass. The size can vary in different patients but usually never exceeds 2 cm.[1] Clinically there has been no recurrence four months post surgery. Most of these lesions arising on nevus flammeus/port wine stain are located outside the distribution of the trigeminal nerve like neck, trunk, or extremities.[2] The pathogenesis of most sporadic pyogenic granulomas and those arising on nevus flammeus remains elusive. Pyogenic granuloma, a reactive vascular tumor and nevus flammeus, a vascular malformation arise via different processes with complex regulatory mechanisms that are under study. Both are vascular lesions and despite having distinct clinical, histopathological, and biological characteristics, these are rarely associated with one another.[4] Our association could be explained by the development of pyogenic granuloma in microscopic arteriovenous anastomoses in vascular lesions, and also by its association with arteriovenous hemangiomas. Another hypothesis says that since pyogenic granulomas are noninfectious, purulent lesions, they develop as reactive inflammatory masses of blood vessels and fibroblasts within the dermis. With the etiology not being fully understood, an unknown stimulus triggers endothelial cell proliferation and angiogenesis leading to a rapidly growing lesion.[1] More recently, few studies have indicated that abnormalities in embryonic vasculogenesis leads to vascular malformations such as nevus flammeus/port wine stain and may further predispose to the development of vascular hyperplasias or tumors.[2] Chemical mediators like inducible nitric oxide synthase have also been implicated in their formation.[2] A study reported 10 pyogenic granulomas secondarily arising over a port wine stain; 8 cases showing BRAF mutation, one case NRAS mutation and GNAQ mutation each. Similar mutations were identified in both the lesions indicating their common origin.[5]
 |
| Figure 1: |
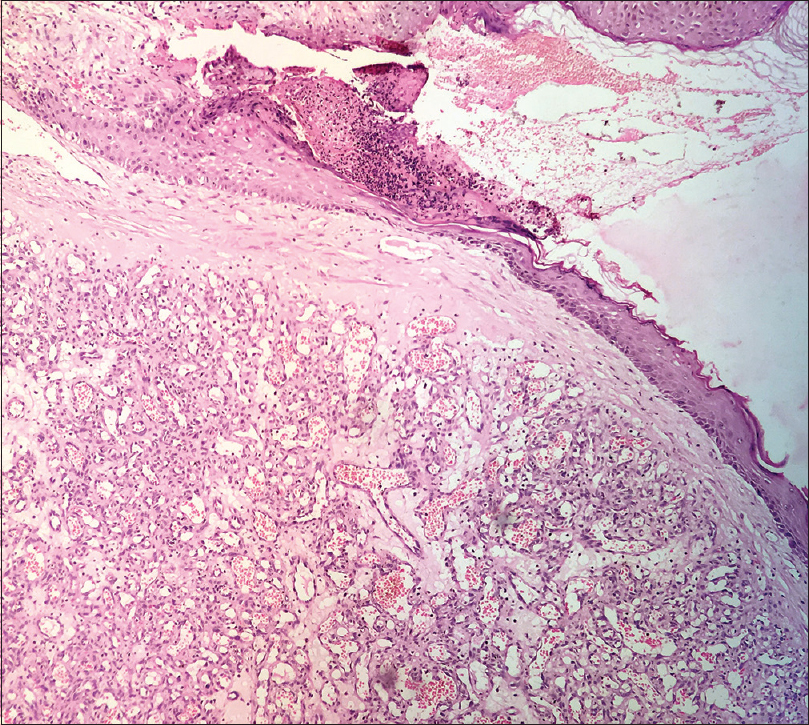 |
| Figure 2: Vascular lesion lined by hyperplastic epithelium with focal parakeratosis and ulceration. Dermis reveals lobules of small capillaries (H&E, 100×) |
There are several methods for treating pyogenic granuloma but recurrence is a major problem for patients. Various therapeutic modalities include excision, curettage, sclerotherapy, radiotherapy, electrocautery, and use of lasers.[1],[2] In the present case, only excisional biopsy was performed for treatment and was not followed by cautery or laser therapy. A recent clinical report presented the successful use of a sclerosing agent ethanolamine for treatment of recurrent pyogenic granuloma associated with port wine stain.[6]
In our case pyogenic granuloma developed de novo, in the absence of any predisposing factor, probably resulting from an underlying arteriovenous anastomosis associated with nevus flammeus. This occurrence offers unique insight into the pathogenesis of these poorly understood but commonly encountered entities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Akbulut F, Akbulut T, Kucukdurmaz F, Sonmezay E, Simsek A, Gurbuz G, et al. Huge pyogenic granuloma of the penis. Case Rep Urol 2015;2015:263168.
[Google Scholar]
|
| 2. |
Sheehan DJ, Lesher JL Jr. Pyogenic granuloma arising within a port-wine stain. Cutis 2004;73:175-80.
[Google Scholar]
|
| 3. |
da Silva AD, Silva CA, de Camargo Moraes P, Thomaz LA, Furuse C, de Araújo VC, et al. Recurrent oral pyogenic granuloma in port-wine stain. J Craniofac Surg 2011;22:2356-8.
[Google Scholar]
|
| 4. |
Aghaei S. Pyogenic granuloma arising in port-wine stain after cryotherapy. Dermatol Online J 2003;9:16.
[Google Scholar]
|
| 5. |
Groesser L, Peterhof E, Evert M, Landthaler M, Berneburg M, Hafner C, et al. BRAF and RAS mutations in sporadic and secondary pyogenic granuloma. J Invest Dermatol 2016;136:481-6.
[Google Scholar]
|
| 6. |
Deore GD, Gurav AN, Patil R, Shete AR, NaikTari RS, Khiste SV, et al. Sclerotherapy: A novel bloodless approach to treat recurrent oral pyogenic granuloma associated with port-wine stain. Ann Vasc Surg 2014;28:1564.e9-14.
[Google Scholar]
|
Fulltext Views
4,023
PDF downloads
2,294





