Translate this page into:
Acral peeling skin syndrome: An underdiagnosed skin disorder
2 Department of Clinical and Transplant Pathology, Institute for Clinical and Experimental Medicine, Prague, Czech Republic
3 Department of Dermatovenereology, Second Faculty of Medicine, Charles University and Hospital Bulovka, Prague, Czech Republic
Correspondence Address:
Eva Sticova
Department of Clinical and Transplant Pathology, Institute for Clinical and Experimental Medicine, Videnska 1958/9, Prague 4 - Krc, 14021
Czech Republic
| How to cite this article: Sticova E, Květoň M, Dubská M, Kubátová A. Acral peeling skin syndrome: An underdiagnosed skin disorder. Indian J Dermatol Venereol Leprol 2019;85:316-318 |
Sir,
Acral peeling skin syndrome (OMIM #609796), first described in 1921 by Fox,[1] is an autosomal recessive cutaneous disorder caused by mutations in the transglutaminase-5 (TGM5) gene[2] and, less frequently, in the cystatin A (CSTA) gene.[3] Acral peeling skin syndrome is a rare disease with unknown prevalence and with dozens of cases described in the medical literature so far. Here we report a case of acral peeling skin syndrome in a young man confirmed histologically and by mutational analysis.
A 28-year-old man, a laboratory technician, was referred with a possible diagnosis of glove-related contact dermatitis as an occupational disease. However, the patient reported a life-long history of superficial skin peeling and vesiculation on the dorsal aspects of hands and feet, provoked by perspiration in gloves, prolonged soaking in water or exposure to heat and/or slight pressure, with a tendency to heal spontaneously within 48 hours. He also complained of a slight burning sensation at the site of skin eruptions.
Except for the skin disorder, the patient was generally healthy. He was unaware of any allergies and did not take any medication. Moreover, the patient's family history was unremarkable regarding skin diseases.
Clinical examination revealed flaccid bullae of size up to 20 mm on normal or slightly erythematous skin on the dorsal aspects of the patient's fingers [Figure - 1]. There was no evidence of bleeding, oozing, suppuration or scarring. Skin peeling was limited only to the acral parts of extremities, whereas other parts of the body and mucosal surfaces, as well as nails, hair and teeth remained unaffected. There were no constitutional symptoms associated. Blood tests including C-reactive protein level, full blood count and erythrocyte sedimentation rate were completely within the normal range.
 |
| Figure 1: Thin-walled blisters and erosions on dorsal aspect of fingers |
Microscopic examination of a punch biopsy revealed slightly acanthotic epidermis with splitting between the stratum granulosum and corneum and within the thickened horny layer. No spongiosis, acantholysis and/or inflammatory interface activity was discernible and there was no remarkable inflammatory infiltrate within the dermis [Figure - 2]. Direct immunofluorescence was completely negative.
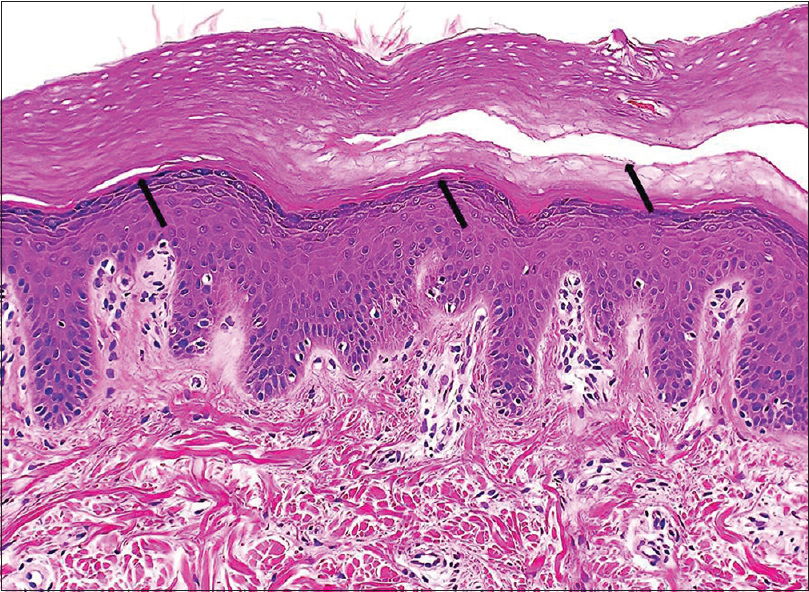 |
| Figure 2: Splitting between the stratum granulosum and corneum and within the horny layer of epidermis (arrows) (hematoxylin and eosin, ×200) |
Mutational analysis of the TGM5 gene by direct sequencing of genomic DNA extracted from peripheral leukocytes was performed to confirm the diagnosis of acral peeling skin syndrome at a molecular level. Exon 3 with the adjacent parts of the intronic sequences was amplified by polymerase chain reaction and the obtained sequence was compared with the reference sequence GenBank NM_004245.3. Analysis of the exon 3 of the TGM5 gene disclosed pathogenic homozygous missense mutation c.337G>T (p. Gly113Cys) and homozygous likely benign mutation c.326C>T (p. Thr109Met) [Figure - 3].
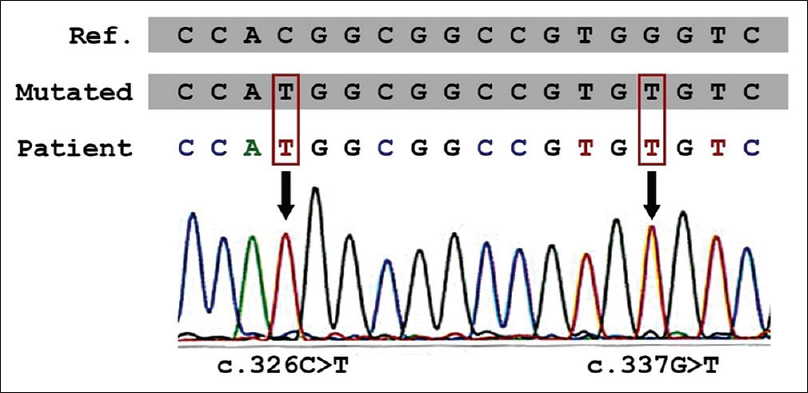 |
| Figure 3: Pathogenic homozygous missense mutation c.337G>T and homozygous likely benign mutation c.326C>T in TGM5 gene |
Therefore, the clinical picture, histopathologic examination and mutational analysis confirmed the diagnosis of acral peeling skin syndrome in this patient.
Acral peeling skin syndrome is a rare genodermatosis characterized by shedding of the superficial layers of the epidermis with blister formation.[1] The most important underlying genetic defect, homozygous or compound heterozygous mutation in TGM5 gene localized to chromosome 15q15, is responsible for inhibition of cross-linking activity of the transglutaminase-5 enzyme, the process essential for terminal differentiation of the epidermis to form the cornified cell envelope.[2],[4] Moreover, mutations in the CSTA gene localized to chromosome 3q21.1, encoding cystatin A, a protease inhibitor found in the cornified cell envelope, have been identified in several patients with acral peeling skin syndrome.[3]
The diagnosis of acral peeling skin syndrome is mainly based on personal history and clinical picture of superficial acral skin peeling and blistering, often exacerbated by heat, maceration and/or minor mechanical trauma.[1]
Histopathology of acral peeling skin syndrome usually reveals mild hyperkeratosis and splitting of the epidermis between the stratum granulosum and corneum or shows an intra-corneal split.[4]
The clinical differential diagnoses include other blistering and exfoliative diseases such as localized form of epidermolysis bullosa simplex, keratolytic winter erythema, keratolysis exfoliativa, tinea mannum, allergic contact dermatitis and dyshidrotic eczema (pompholyx).
The clinical picture of life-long acral skin peeling in a patient without history of atopy and/or preceding exposure to contact allergens or irritants, negative results of patch and microbiological tests, along with characteristic histopathology findings in a skin biopsy help to determine the correct diagnosis. Molecular genetics is a supportive method that may be helpful in complicated cases. Some authors consider acral peeling skin syndrome under-reported and frequently misdiagnosed, predominantly as a localized form of epidermolysis bullosa simplex.[5] Thus, when epidermolysis bullosa is not confirmed by mutations in corresponding genes in suspected cases, screening for TGM5 mutations is recommended.[5]
Treatment of acral peeling skin syndrome is mostly symptomatic and includes protection from heat, humidity and trauma, predominantly pressure and friction. Topical emollients and keratolytic agents may help some patients. Other treatment modalities such as methotrexate, ultraviolet B phototherapy, isotretinoin and corticosteroids seem to be ineffective.
Acknowledgement
The authors acknowledge gratefully the help of Mgr. Votypka with mutational analysis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
The work was supported by Ministry of Health, Czech Republic – conceptual development of research organization (“Institute for Clinical and Experimental Medicine – IKEM, IN 00023001”).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Fox H. Skin shedding (keratolysis exfoliativa congenital): Report of a case. Arch Dermatol 1921;3:202.
[Google Scholar]
|
| 2. |
Cassidy AJ, van Steensel MA, Steijlen PM, van Geel M, van der Velden J, Morley SM, et al. Ahomozygous missense mutation in TGM5 abolishes epidermal transglutaminase 5 activity and causes acral peeling skin syndrome. Am J Hum Genet 2005;77:909-17.
[Google Scholar]
|
| 3. |
Krunic AL, Stone KL, Simpson MA, McGrath JA. Acral peeling skin syndrome resulting from a homozygous nonsense mutation in the CSTA gene encoding cystatin A. Pediatr Dermatol 2013;30:e87-8.
[Google Scholar]
|
| 4. |
Pigors M, Kiritsi D, Cobzaru C, Schwieger-Briel A, Suárez J, Faletra F, et al. TGM5 mutations impact epidermal differentiation in acral peeling skin syndrome. J Invest Dermatol 2012;132:2422-9.
[Google Scholar]
|
| 5. |
Szczecinska W, Nesteruk D, Wertheim-Tysarowska K, Greenblatt DT, Baty D, Browne F, et al. Under-recognition of acral peeling skin syndrome: 59 new cases with 15 novel mutations. Br J Dermatol 2014;171:1206-10.
[Google Scholar]
|
Fulltext Views
23,822
PDF downloads
2,593





