Translate this page into:
Pulsed dye laser in the treatment of basal cell carcinoma: A single session versus two sessions – a randomized controlled trial
2 Department of Pathology, Faculty of Medicine, Tanta University, Tanta, Egypt
3 Department of Plastic and Reconstructive Surgery, Faculty of Medicine, Tanta University, Tanta, Egypt
Correspondence Address:
Nashwa Naeem El-Far
Department of Dermatology and Venereology, Faculty of Medicine, Tanta University, Tanta
Egypt
| How to cite this article: Abd El-Naby NM, El-Far NN, Al-Shenawy HA, Elshwadfy SE, Koura AA. Pulsed dye laser in the treatment of basal cell carcinoma: A single session versus two sessions – a randomized controlled trial. Indian J Dermatol Venereol Leprol 2019;85:475-480 |
Abstract
Background: Basal cell carcinoma is the most common form of skin cancer worldwide. It has a specialized microvasculature system that can be targeted by the pulsed dye laser using the theory of selective photothermolysis.
Objective: To evaluate the efficacy and safety of single session versus two sessions of pulsed dye laser in the treatment of basal cell carcinoma.
Methods: A total of 22 patients with basal cell carcinoma were collected in this randomized controlled trial. The patients were divided into two groups: Group I – 11 patients were treated by one session of pulsed dye laser, and Group II – 11 patients received two sessions of pulsed dye laser 2 weeks apart. The patients were assessed clinically and histopathologically after end of the treatment.
Results: There was a significant improvement of basal cell carcinoma clinically and histopathologically. Maximal histological clearance rate was achieved in superficial basal cell carcinoma type, small-sized basal cell carcinoma <0.7 cm and in cases with strong inflammatory response after laser treatment. Treatment of basal cell carcinoma with two sessions of pulsed dye laser was more effective than one session treatment.
Limitations: The small sample size of patients and the limited location of the lesions on the head compared with trunk and extremities. Also, the lack of adequate study power may prevent generalization of results.
Conclusion: Pulsed dye laser proved to be a safe, effective and noninvasive modality for the treatment of basal cell carcinoma that can be used as a monotherapy in small-sized lesions. Also, it can be used to debulk large-sized lesions before surgery.
Introduction
Basal cell carcinoma is a common malignant skin tumor in humans, and its incidence is increasing.[1],[2] In the United States, approximately one million new cases are annually diagnosed.[2] This cutaneous malignancy rarely metastasizes, but is locally destructive and invasive.[3],[4] Exposure to ultraviolet radiation is generally accepted as the major cause of basal cell carcinoma.[5]
To determine the optimal treatment for basal cell carcinoma, the location, size, type and number of tumors need to be evaluated. There are numerous options available to treat basal cell carcinomas, such as ablative procedures that carry high rates of efficacy but can be time-consuming, costly and may lead to infections and scarring.[6] Nonablative topical treatments such as chemotherapy and immunomodulators are unreliable when used by the patient at home and are limited by their use mainly in smaller superficial basal cell carcinomas and higher recurrence rates than surgical therapies.[7]
Pulsed dye laser is generally used to treat vascular skin lesions. Basal cell carcinomas are highly vascular tumors with clinically evident telangiectasias. Although the exact mechanism of action of pulsed dye laser basal cell carcinomas is unclear, the main hypothesis is the antiangiogenic effect, via specific targeting of the numerous dilated blood vessels found in basal cell carcinomas. Pulsed dye laser destroys the tumor's blood supply, leading to eventual clearing of the tumor.[8],[9]
In this study, we evaluated the efficacy and safety of single session versus two sessions of pulsed dye laser in the treatment of basal cell carcinoma.
Methods
In this randomized controlled trial, 22 newly diagnosed patients with different types of basal cell carcinoma (20 of them on the face and 2 on the scalp with skin phototype III and IV) were collected by care providers between May 2015 and May 2016 from the outpatient clinic of Dermatology Department, Tanta University Hospitals, Egypt. Patients were randomized (the method of randomization has not been mentioned); 11 patients for treatment with one stacked pulsed dye laser session (Group I) and 11 patients received two stacked pulsed dye laser session, 2 weeks apart (Group II).
Patients with history of wound healing abnormalities, other dermatological diseases, immunosuppressive diseases, currently undergoing chemical peeling, dermabrasion or radiotherapy, or with cutaneous bacterial or viral infection in the area to be treated were excluded.
The study was approved by the Research Ethics Committee (approval code 2951/12/4) and all participants signed an informed consent before participation in the study. The patients were simply randomized to each of the study groups using a computer-generated list. Allocation concealment was ensured by enclosing assignments in sequentially numbered, opaque-sealed envelopes, which only were opened when the study was started.
Therapeutic technique
Pulsed dye laser (SYNCHRO VASQ, QA3B2501, Italy) of 595 nm was used with handpiece 8, fluency 7 J/cm2, pulse width 20 ms, rate 1 Hz and cooling with 4 mm margins.
Local anesthesia was given for all patients 30 min before laser sessions and then the handpiece was held perpendicular to the lesion, directing the pulses to the whole lesion and to cover 4 mm safety margin all around. The pulses were of stack type and were given until bluish discoloration of the lesion was observed. A topical, broad spectrum antibiotic was applied 2–3 times daily for 1 week for all patients who were advised to avoid sun exposure and traumatizing the lesion.
Assessment of the efficacy of the therapeutic procedures
- Photographs were taken for the lesions at baseline, after the session of treatment and after the follow-up period (1 month)
- Clinical evaluation of patients was done by three physicians who were blinded to the mode of therapy, giving the grade of improvement as follows: Excellent: >75–100%, moderate: >50–75%, mild: >25–50% and no improvement: <25%. Safety and tolerability assessment were recorded
- Histopathological examination: 2 mm punch biopsy specimen was taken from the lesion at baseline to confirm the diagnosis of basal cell carcinoma, tumor type and inflammatory cells expression. After 1 month from the last laser treatment session, all patients were subjected to complete surgical excision of the tumor.
All the excisional biopsies were processed, embedded in paraffin blocks and cut at 4 μm sections; then stained by hematoxylin and eosin stains to be examined for pattern and type of growth, the margins, the inflammatory response (subjective measures as if weak+, moderate++, strong+++).
Efficacy was categorized into:[8]
- Complete response: if no histological evidence of basal cell carcinoma after standard sectioning of the tumor
- Incomplete response: if any residual histological evidence of basal cell carcinoma in the excised tumor
- No response: if the residual tumor was 100%.
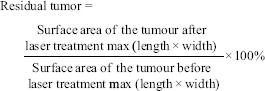
Histological clearance rate was measured as (100% − Residual tumor %).
Comparison between different groups regarding categorical variables was tested using χ2-test. When more than 20% of the cells have expected count < 5, correction for χ2 was conducted using Fisher's exact test or Monte-Carlo correction. Mann–Whitney U test was used for intragroup analysis. Significance test results are quoted as two-tailed probabilities. Significance of the obtained results was judged at the 5% level.
Results
Clinical results
There was no significant difference between both studied groups regarding their demographic data. Concerning the morphological types of basal cell carcinoma of the involved patients, there were 10 (45.5%) patients with nodular basal cell carcinoma, 7 (31.8%) patients with rodent ulcers (rodent ulcer is not a histological entity please explain), 3 (13.6%) patients with superficial basal cell carcinoma, 1 (4.5%) patient with pigmented basal cell carcinoma and 1 (4.5%) patient with cystic basal cell carcinoma. Twenty (90.9%) patients showed affection of the face and two (9.1%) patients showed affection of the scalp.
There was statistically significant difference between both groups as regards the clinical improvement (P-value = 0.005). In Group I, 1 (9.1%) patient showed excellent improvement, 2 (18.2%) patients showed moderate improvement, 2 (18.2%) patients showed mild improvement and 6 (54.5%) patients showed no improvement. In Group II, 7 (63.6%) patients showed excellent improvement, 3 (27.3%) patients showed moderate improvement and 1 (9.1%) patient showed mild improvement [Table - 1], [Figure - 1] and [Figure - 2].

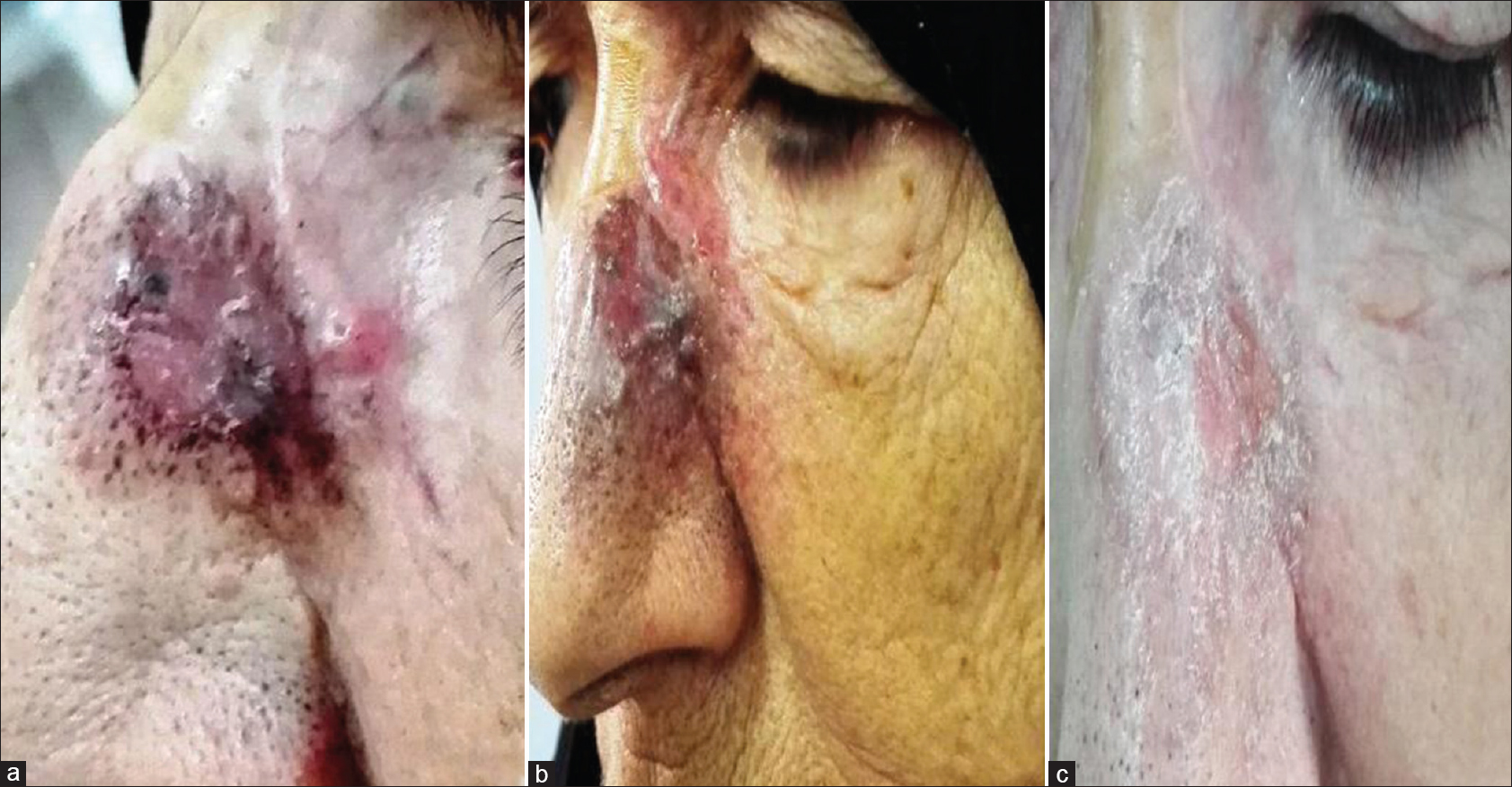 |
| Figure 1: (a) Superficial basal cell carcinoma (before treatment), (b) After one session of pulsed dye laser, (c) One month after two sessions with excellent improvement |
 |
| Figure 2: (a) Nodular basal cell carcinoma (before treatment), (b) After one session of pulsed dye laser, (c) One month after two sessions with excellent improvement |
There was statistically significant decrease in the tumor size after laser treatment in both groups (P-value = 0.005* and 0.012*, respectively). In Group I, before treatment, the mean surface area was (1.9 ± 2.9) cm2, although after treatment it became (1.2 ± 2.1) cm2. In Group II, before treatment, the mean surface area was (1.7 ± 1.8) cm2; although after treatment there was complete response of three patients, so the number of remaining patients became eight. Among the remaining patients, the mean surface area was (0.6 ± 0.5) cm2.
There was no statistically significant difference between the safety and tolerability of therapy in this study (<0.001). In Group I, only 2 (18.2%) patients had pain and ulcer. In Group II, 2 (18.2%) patients showed hyperpigmentation and 2 (18.2%) patients showed hypopigmented scar. There was no recurrence of basal cell carcinoma reported in the studied patients during follow-up period (6 months).
Histopathological results
There were 10 patients with nodular basal cell carcinoma [divided as 5 (45.5%) patients in Group I and 5 (45.5%) patients in Group II], in which 7 patients had rodent ulcers [divided into 3 (27.2%) patients of keratotic basal cell carcinomas in Group I and 4 (36.3%) patients of adenocystic basal cell carcinomas in Group II] and 3 patients had superficial basal cell carcinomas [divided as 2 (18.2%) patients in Group I and 1 (9.1%) patient in Group II] and 2 patients had pigmented basal cell carcinoma [1 (9.1%) patient in Group I and 1 (9.1%) patient in Group II].
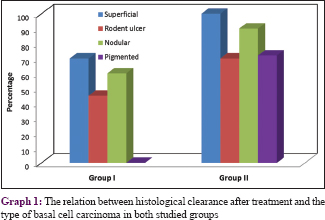
There was statistically significant difference between the two groups regarding histopathological evaluation of residual tumor cells after treatment (P = 0.005). In Group I, there was an incomplete response varied between 16 and 100% with a mean of (51.9 ± 22.3) of residual tumor tissue in 10 (90.9%) patients while 1 (9.1%) patient showed no response. Whereas in Group II, there were 2 (18.2%) patients showed complete response and 9 (81.8%) patients showed incomplete response varied between 0 and 53% with a mean of (24.1 ± 17.3) [Table - 1]. The maximal histological clearance rate was achieved in superficial basal cell carcinoma type in both groups [Graph 1].
By comparing the inflammatory response between the both groups before and after treatment, it was statistically significant only in Group II (P = 0.021). In Group I before treatment, plasma cells and lymphocytes were occasionally seen in the tumor specimen and variably expressed as seven patients had weak expression, three patients moderate expression and one patient strong expression. After treatment, the inflammatory infiltrate expressed by four patients were weak, four patients were moderate and three patients were strong expression.
In Group II before treatment, plasma cells and lymphocytes are occasionally seen in the tumor specimen and variably expressed as six patients had weak expression, three patients moderate and two patients showed strong expression. After treatment, the inflammatory infiltrate expressed as one patient was weak expression, two patients were moderate expression and eight patients were strong expression.
Maximal histological clearance rate was achieved in superficial basal cell carcinoma type [Graph 1]. There was a significant negative correlation between the histological clearance after laser treatment and duration of the lesion in Group I, while there was a significant positive correlation between the histological clearance after laser treatment and diameter and duration of the lesion in Group II [Table - 2].

Discussion
In the current study, in Group I, 3 (27.3%) patients showed moderate to excellent improvement, whereas 8 (72.7%) patients showed mild to no improvement. In Group II, 10 (90.9%) patients showed moderate to excellent improvement and only 1 (9.1%) patient showed mild improvement. According to clinical evaluation on patient's improvement, two sessions of treatment were significantly more effective than one session.
There was significant decrease in the tumor size after laser treatment in both groups. These results agreed with Shah et al., who reported that multiple treatments of basal cell carcinomas with pulsed dye laser resulted in dramatically reduced tumor mass.[8] Another study by Norman et al. found that the treatment reduces the size of the tumors, which was helpful for patients, particularly in cosmetically pertinent areas.[10]
The clinical appearance of basal cell carcinoma reflects its highly vascularized nature. Erythema and telangiectasias are commonly seen clinically in basal cell carcinomas.[2] Basal cell carcinomas possess a capillary plexus throughout the tumor.[11] Many of these vessels are abnormally enlarged.[12] Basal cell carcinomas, like many other solid tumors, rely on a specialized tumor-associated microvasculature for growth. Because of the interdependence of tumor cells and tumor vasculature, prolonged ischemia secondary to selective destruction of the tumor's blood supply could produce destruction of the tumor. Vascular targeting is a relatively new anticancer strategy which has as its goal the destruction of tumor vasculature.[11] The main hypothesis for the mechanism of action of pulsed dye laser is antiangiogenic, via specific targeting of the numerous dilated blood vessels found in basal cell carcinomas, and pulsed dye laser destroys the tumor's bloods supply, leading to eventual demise of the tumor.[8],[9]
The technique was tolerable and safe with minimal side effects for the majority of our patients. These results agreed with Tran et al. who reported mild scarring, eschar and hypopigmentation in their studied cases.[13] In addition, Konnikov et al. noted that there was hypopigmentation in laser treated areas.[9]
There was statistically significant better response in Group II than Group I regarding histopathological evaluation of residual tumor cells after treatment. These results matched with other studies, considering that with more sessions there will be more clearance and less residual tumor cell burden.[13],[14],[15]
There was statistically significant increase in the inflammatory response histopathologically after laser treatment in Group II only. This result agreed with Tran et al., who reported that by examination of the excisional biopsies after 1 month of pulsed dye laser session, there was fibrosis, vertically oriented bland appearing vessels, mild lymphohistiocytic inflammation and dermal edema.[13] Another study by Shah et al. revealed that the re-excision specimens that were examined histologically showed prominent vascularity and erythrocyte extravasation in the reticular dermis, which correlated with known laser-induced dermal changes.[8]
In our study, the maximal histological clearance rate was achieved in superficial basal cell carcinoma type, small-sized basal cell carcinoma < 0.7 cm and in cases with strong inflammatory response after laser treatment. These results agreed with other studies which reported that high clearance rate achieved in superficial basal cell carcinoma according to the type.[14],[16],[17],[18] Also other studies recorded that smaller basal cell carcinomas had a higher clearance rate compared to larger basal cell carcinomas.[8],[9],[15] This could be explained by the fact that smaller basal cell carcinomas are associated with vasculature may still be in a fragile, nascent phase of growth, and thus more susceptible to laser treatment.[8]
In general, various types of lasers are used in oncology to debulk tumors, using both selective and ablative methods.[19] Pulsed dye laser has been used to selectively target tumor vasculature with success in treating glottal dysplasia and squamous cell carcinoma in situ using 585 nm pulsed dye laser.[20],[21] Depending on fluence, 595 nm pulsed dye laser can penetrate skin to thicknesses ranging from 0.8 to 1.3 mm. This range of dermal penetration encompasses the depth of the vasculature that supports most basal cell carcinoma. Ectatic dermal blood vessels treated with 595 nm pulsed dye laser can undergo selective photothermolysis with minimal damage to the surrounding tissue structures.[22] Thus, targeting the blood supply of basal cell carcinomas may be effective for treating these tumors.[8]
Ibrahimi et al. conducted a case study on a patient with basal cell nevus syndrome and treated multiple superficial and nodular basal cell carcinomas with long-pulsed Alexandrite laser that also has vascular selectivity and deeper tissue penetration.[23] The clearance rate of this study was 83% with 7 months follow-up. Moskalik et al. performed treatment of facial 27 basal cell carcinomas using pulsed Neodymium laser and Nd:Yag laser with 2.2 and 3.1% recurrence rates, respectively, with mean follow-up of 13 months.[19] The efficacy of Nd:Yag laser was attributed to its deep photo-destructive mechanism of action that leads to thermal destruction and coagulation of the tissue. The treatment was performed under local anesthesia to minimize discomfort. The majority of the patients had good cosmetic results with minimal scarring.
It could be concluded that pulsed dye laser therapy was proved clinically and histopathologically to be safe, effective and noninvasive modality for treatment of basal cell carcinoma. The maximal histological clearance rate achieved in superficial basal cell carcinoma type, small-sized basal cell carcinoma < 0.7 cm and in cases with strong inflammatory response after laser treatment. Treatment of basal cell carcinoma with two sessions of pulsed dye laser was more effective than one session treatment that can be used as a monotherapy in small-sized lesions. Also, it could be used to debulk large-sized lesions before surgery.
The limitations in our study were small sample size of patients and the limited location of the lesions that were on the head compared with trunk and extremities. Also, the lack of adequate power may prevent generalization of results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Diffey BL, Langtry JA. Skin cancer incidence and the ageing population. Br J Dermatol 2005;153:679-80.
[Google Scholar]
|
| 2. |
Neville JA, Welch E, Leffell DJ. Management of nonmelanoma skin cancer in 2007. Nat Clin Pract Oncol 2007;4:462-9.
[Google Scholar]
|
| 3. |
Shriner DL, McCoy DK, Goldberg DJ, Wagner RF Jr. Mohs micrographic surgery. J Am Acad Dermatol 1998;39:79-97.
[Google Scholar]
|
| 4. |
Nagler RM, Laufer D. Invading basal cell carcinoma of the jaw: An under-evaluated complex entity. Anticancer Res 2001;21:759-64.
[Google Scholar]
|
| 5. |
Gallagher RP, Hill GB, Bajdik CD, Fincham S, Coldman AJ, McLean DI. Sunlight exposure, pigmentary factors, and risk of nonmelanocytic skin cancer. I. Basal cell carcinoma. Arch Dermatol 1995;131:157-63.
[Google Scholar]
|
| 6. |
Tierney EP, Hanke CW. Cost effectiveness of Mohs micrographic surgery: Review of the literature. J Drugs Dermatol 2009;8:914-22.
[Google Scholar]
|
| 7. |
Lien MH, Sondak VK. Nonsurgical treatment options for basal cell carcinoma. J Skin Cancer 2011;2011:571734.
[Google Scholar]
|
| 8. |
Shah SM, Konnikov N, Duncan LM, Tannous ZS. The effect of 595 nm pulsed dye laser on superficial and nodular basal cell carcinomas. Lasers Surg Med 2009;41:417-22.
[Google Scholar]
|
| 9. |
Konnikov N, Avram M, Jarell A, Tannous Z. Pulsed dye laser as a novel non-surgical treatment for basal cell carcinomas: Response and follow up 12-21 months after treatment. Lasers Surg Med 2011;43:72-8.
[Google Scholar]
|
| 10. |
Minars N, Blyumin-Karasik M. Treatment of basal cell carcinomas with pulsed dye laser: A case series. J Skin Cancer 2012;2012:286480.
[Google Scholar]
|
| 11. |
Grunt TW, Lametschwandtner A, Staindl O. The vascular pattern of basal cell tumors: Light microscopy and scanning electron microscopic study on vascular corrosion casts. Microvasc Res 1985;29:371-86.
[Google Scholar]
|
| 12. |
Moskalik K, Kozlov A, Demin E, Boiko E. The efficacy of facial skin cancer treatment with high-energy pulsed neodymium and Nd: YAG lasers. Photomed Laser Surg 2009;27:345-9.
[Google Scholar]
|
| 13. |
Snipes CJ, Sniezek PJ, Walling HW. Basal cell carcinoma responding to systemic 5-fluorouracil. J Am Acad Dermatol 2006;54:1104-6.
[Google Scholar]
|
| 14. |
Allison KP, Kiernan MN, Waters RA, Clement RM. Pulsed dye laser treatment of superficial basal cell carcinoma: Realistic or not? Lasers Med Sci 2003;18:125-6.
[Google Scholar]
|
| 15. |
Ballard CJ, Rivas MP, McLeod MP, Choudhary S, Elgart GW, Nouri K. The pulsed dye laser for the treatment of basal cell carcinoma. Lasers Med Sci 2011;26:641-4.
[Google Scholar]
|
| 16. |
Campolmi P, Troiano M, Bonan P, Cannarozzo G, Lotti T. Vascular based non conventional dye laser treatment for basal cell carcinoma. Dermatol Ther 2008;21:402-5.
[Google Scholar]
|
| 17. |
Karsai S, Friedl H, Buhck H, Jünger M, Podda M. The role of the 595-nm pulsed dye laser in treating superficial basal cell carcinoma: Outcome of a double-blind randomized placebo-controlled trial. Br J Dermatol 2015;172:677-83.
[Google Scholar]
|
| 18. |
Campolmi P, Mavilia L, Bonan P, Cannarozzo G, Lotti TM. 595 nm pulsed dye laser for the treatment of superficial basal cell carcinoma. Lasers Med Sci 2005;20:147-8.
[Google Scholar]
|
| 19. |
Moskalik K, Kozlow A, Demin E, Boiko E. Powerful neodymium laser radiation for the treatment of facial carcinoma: 5 year follow-up data. Eur J Dermatol 2010;20:738-42.
[Google Scholar]
|
| 20. |
Zeitels SM, Franco RA Jr., Dailey SH, Burns JA, Hillman RE, Anderson RR. Office-based treatment of glottal dysplasia and papillomatosis with the 585-nm pulsed dye laser and local anesthesia. Ann Otol Rhinol Laryngol 2004;113:265-76.
[Google Scholar]
|
| 21. |
Britton JE, Goulden V, Stables G, Stringer M, Sheehan-Dare R. Investigation of the use of the pulsed dye laser in the treatment of Bowen's disease using 5-aminolaevulinic acid phototherapy. Br J Dermatol 2005;153:780-4.
[Google Scholar]
|
| 22. |
Pikkula BM, Chang DW, Nelson JS, Anvari B. Comparison of 585 and 595 nm laser-induced vascular response of normal in vivo human skin. Lasers Surg Med 2005;36:117-23.
[Google Scholar]
|
| 23. |
Ibrahimi OA, Sakamoto FH, Tannous Z, Anderson RR. 755 nm alexandrite laser for the reduction of tumor burden in basal cell nevus syndrome. Lasers Surg Med 2011;43:68-71.
[Google Scholar]
|
Fulltext Views
4,195
PDF downloads
1,701





