Translate this page into:
Giant cell tumor of tendon sheath in children
Correspondence Address:
Swagata Arvind Tambe
Department of Dermatology, Topiwala National Medical College and B. Y. L. Nair Hospital, Mumbai, Maharashtra
India
| How to cite this article: Ansari SM, Tambe SA, Nayak CS. Giant cell tumor of tendon sheath in children. Indian J Dermatol Venereol Leprol 2019;85:496-498 |
Sir,
Giant cell tumor of tendon sheath is the second most common soft tissue tumor of the hand after ganglion cyst. It originates in the flexor sheath synovium. In the hand, it typically occurs adjacent to the distal interphalangeal joint of the index or long finger. It is more frequent in the 20–50 years age group with rare occurrence in children. We report three cases of this tumour in children.
Case 1: A 9-year-old girl presented with an asymptomatic nodule on the left index finger of 6 months' duration without preceding trauma. Cutaneous examination revealed a 1.5 cm × 1.5 cm, skin-colored, dome-shaped, nontender, nonmobile, firm to hard nodule on the palmar and lateral aspect of the left index finger [Figure - 1]. High-frequency ultrasonography showed a well-defined hypoechoic mass in the dermis.
 |
| Figure 1: Case 1: A single, well-defined, skin-colored, firm to hard, smooth surfaced nontender, fixed nodule, 1.5 cm × 1.5 cm, on palmar and lateral aspect of left index finger |
Case 2: A 3-year-old girl presented with a painless nodule of 2–3 months' duration on the right index finger without preceding trauma. Cutaneous examination revealed a well-defined, 1 cm × 0.5 cm, nontender, nonmobile, firm to hard nodule, not adherent to overlying skin on the palmar and lateral aspect of the right index finger [Figure - 2]. Magnetic resonance imaging showed a well-defined soft tissue mass.
 |
| Figure 2: Case 2: A single, well-defined, skin-colored, firm to hard, smooth surfaced nontender, fixed nodule, 1.5 cm × 1.5 cm, on palmar and lateral aspect of right index finger |
Case 3: A 13-year-old girl presented with a painful nodule on the right thumb of 2 months' duration with history of preceding trauma. Clinical examination revealed a well-defined, 1 cm × 1 cm, skin-colored, dome-shaped, tender, nonmobile, firm to hard nodule, on the dorsal aspect of the right thumb near distal interphalangeal joint [Figure - 3]a. High-frequency ultrasonography showed a well-defined hypoechoic mass with internal echoes arising from the tendon over the joint capsule on the extensor aspect of the distal interphalangeal joint of the right thumb [Figure - 3]b.
 |
| Figure 3 |
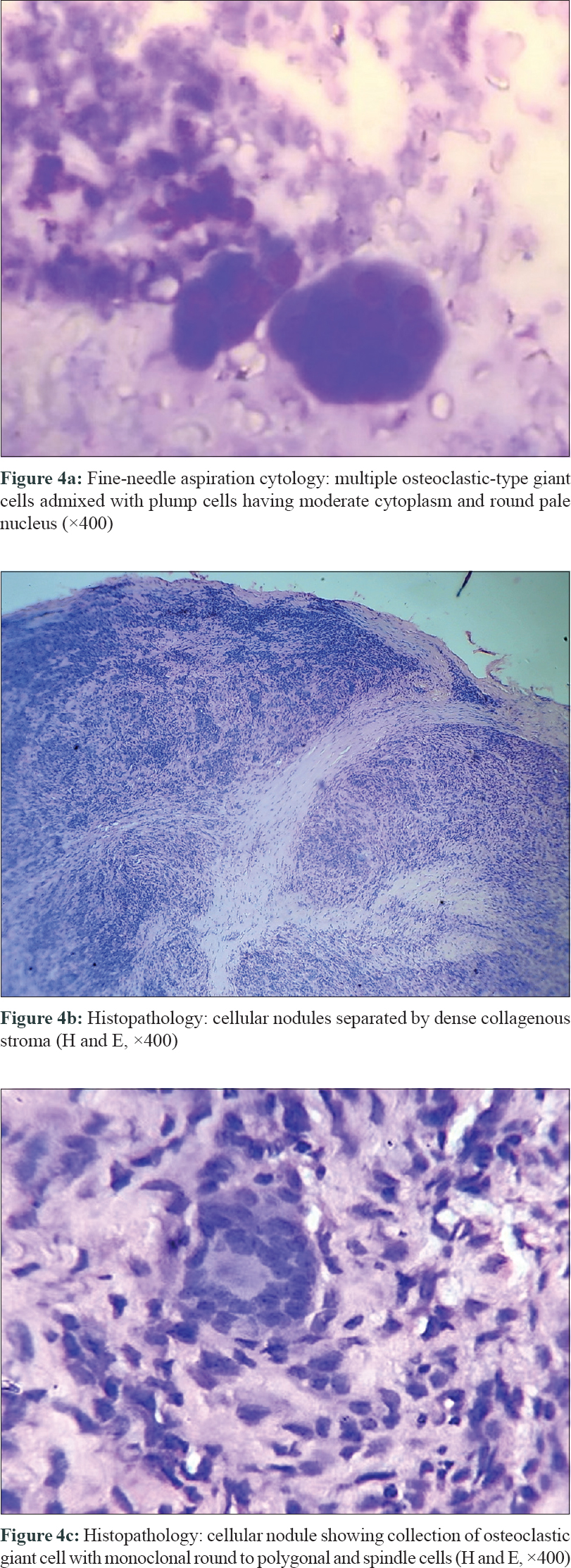
Radiograph showed soft tissue swelling without bony erosion. Fine-needle aspiration cytology (FNAC) revealed the presence of multiple osteoclastic type of giant cells admixed with plump cells having moderate cytoplasm and round nucleus [Figure - 4]a, features suggestive of giant cell tumor of tendon sheath in all the three cases.
 |
| Figure 4 |
Complete excision was done under local anesthesia, and the histopathological examination of excised specimen in all the three cases revealed cellular nodules separated by collagenous stroma. The nodules were composed of histiocytes with abundant eosinophilic cytoplasm, multinucleated giant cells of osteoclastic type, and monoclonal round to polygonal and spindle cells [Figure - 4]b and [Figure - 4]c.
The first and the third patients did not have any recurrence for 3 years and 1 year, respectively. The second patient was lost to follow-up after surgery [Figure - 5]a and [Figure - 5]b.
 |
| Figure 5 |
Giant cell tumor of tendon sheath is the second most common soft tissue tumor of the hand, which usually originates in the synovium of the flexor sheath.[1],[2],[3] It is a gradually developing, painless soft tissue tumor that contains a circumscribed proliferation of synovial cells accompanied by multinucleate giant cells, foam cells, siderophages, and inflammatory cells.[4] It was first defined as a fibrous xanthoma by Chassaignac in 1952.[5] It is also known as a fibrous histiocytoma of synovium, pigmented nodular tenosynovitis, tenosynovial giant cell tumor, localized nodular tenosynovitis, benign synovioma, and fibrous xanthoma of synovium.
It is uncommon in children under 10 years of age with incidence of upto 4.3%.[6] In three different studies evaluating prevalence of hand tumors in children, the incidence of Giant cell tumor of tendon sheath was 0%, 17%, and 3%, respectively.[7],[8],[9] The female-to-male ratio - is 3:2.[10]
The tumor is of two types: diffuse and localized. The localized type is morecommon as compared to the diffuse type which is larger in size and may lead to restriction of joint movements.
It presents as a firm, nontender, nonfluctuant nodule in a digit of the hand. The most common site is the index finger (26%) followed by the middle finger, thumb, ring finger, and littlefinger. The tumor is predominantly palmar, although Ushijima et al. reported dorsal tumors to be more prevalent.[10]
FNAC can be used as a primary diagnostic aid for definitive diagnosis. It helps in preoperative planning to prevent recurrence.
The differential diagnoses include myxoid cyst, rheumatoid nodule, foreign body granuloma, tendinous xanthoma, subcutaneous granuloma annulare, infantile myofibromatosis, fibroma of tendon sheath, infantile digital fibromatosis, and melorheostosis.
Treatment for giant cell tumor of tendon sheath is local excision with careful preservation of flexor and extensor tendons, digital arteries, and nerves. Because of the usual presence of a pseudocapsule, the tumor can often be removed en bloc. With recurrence rates of up to 45% reported, careful attention must be paid while excising these tumors. To prevent recurrences, satellite lesions and connections should be excised, and if bony erosion is present, cortical shell should be curetted.[5]
We report these three girls with giant cell tumor of tendon sheath as its occurrence is rare in children.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Suresh SS, Zaki H. Giant cell tumor of tendon sheath: Case series and review of literature. J Hand Microsurg 2010;2:67-71.
[Google Scholar]
|
| 2. |
Al-Qattan MM. Giant cell tumours of tendon sheath: Classification and recurrence rate. J Hand Surg Br 2001;26:72-5.
[Google Scholar]
|
| 3. |
Darwish FM, Haddad WH. Giant cell tumour of tendon sheath: Experience with 52 cases. Singapore Med J 2008;49:879-82.
[Google Scholar]
|
| 4. |
Somerhausen NS, Dal Cin P. Giant cell tumour of tendon sheath. In: Fletcher CD, Krishnan Unni K, Mertens F, editors. Pathology and Genetics of Tumours of the Soft Tissues and Bones (World Health Organization Classification of Tumours). Lyon: IARC Press; 2002. p. 110-1.
[Google Scholar]
|
| 5. |
Adams EL, Yoder EM, Kasdan ML. Giant cell tumor of the tendon sheath: Experience with 65 cases. Eplasty 2012;12:e50.
[Google Scholar]
|
| 6. |
Gholve PA, Hosalkar HS, Kreiger PA, Dormans JP. Giant cell tumor of tendon sheath: Largest single series in children. J Pediatr Orthop 2007;27:67-74.
[Google Scholar]
|
| 7. |
Woods JE, Murray JE, Vawter GF. Hand tumors in children. Plast Reconstr Surg 1970;46:130-9.
[Google Scholar]
|
| 8. |
Azouz EM, Kozlowski K, Masel J. Soft-tissue tumors of the hand and wrist of children. Can Assoc Radiol J 1989;40:251-5.
[Google Scholar]
|
| 9. |
Colon F, Upton J. Pediatric hand tumors. A review of 349 cases. Hand Clin 1995;11:223-43.
[Google Scholar]
|
| 10. |
Ushijima M, Hashimoto H, Tsuneyoshi M, Enjoji M. Giant cell tumor of the tendon sheath (nodular tenosynovitis). A study of 207 cases to compare the large joint group with the common digit group. Cancer 1986;57:875-84.
[Google Scholar]
|
Fulltext Views
9,732
PDF downloads
1,737





