Translate this page into:
Expression and correlation of interleukin-36γ, claudin-1 and claudin-7 in psoriasis
Correspondence Address:
Hong Fang
Department of Dermatology, The First Affiliated Hospital of Zhejiang University, Hangzhou, Zhejiang
China
| How to cite this article: Pan Y, Tang S, Xu L, Zheng S, Qiao J, Fang H. Expression and correlation of interleukin-36γ, claudin-1 and claudin-7 in psoriasis. Indian J Dermatol Venereol Leprol 2019;85:534-536 |
Sir,
Psoriasis is characterized by exaggerated and disordered epidermal cell proliferation and keratinization. The impaired epidermal barrier plays a role in the pathogenesis of psoriasis. Tight junctions form a barrier in the granular cell layer of the epidermis and are involved in proliferation, differentiation, cell–cell adhesion, and apoptosis of keratinocytes.[1] Claudin-1 and claudin-7 play crucial roles in the formation of these tight junctions and are associated with its strength, size, and ion specificity. The alteration of the tight junction proteins is an early event in psoriasis, with claudin-1 and claudin-7 being downregulated in the basal and uppermost layers of the epidermis.[2] The expression level of claudin-1 is lower in the psoriatic plaque, compared to the healthy or uninvolved skin.
Interleukin-36 (IL-36) belongs to the IL-1 family of cytokines and includes IL-36α, IL-36β, IL-36γ, and IL-36 receptor antagonist (Ra). All the forms of IL-36 are overexpressed in the psoriatic skin lesion. The hypothesis that the tight junctions and other skin barriers, including the immunological barrier, influence each other, was supported by a variety of experimental data. Watson et al. showed that IL-1β can downregulate the expression of tight junction proteins in the skin.[3] IL-36, a member of the IL-1 family of cytokines, might also influence the expression of these proteins. In this study, IL-36γ was selected in the lesional skin of psoriasis patients, as it is the only IL-36 cytokine constitutively expressed in the skin and may become a potential biomarker of psoriasis.[4] This study detected the expression of IL-36γ and tight junction proteins and revealed their correlation in psoriasis.
A total of 42 patients diagnosed with extensive psoriasis vulgaris, and 15 age- and gender-matched healthy controls, attending the Department of Dermatology of First Affiliated Hospital of Zhejiang University, Hangzhou, China, were included in the study. Skin biopsy was obtained from the lesion and immunohistochemistry was performed on it. None of the patients receive any systemic treatment for 3 months or any topical medication for 2 weeks prior to the biopsy. Patients with any other skin or systemic disorder were excluded. Psoriasis Area and Severity Index score was used to evaluate the severity of the disease.
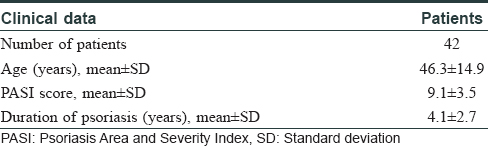
The age of the included patients ranged from 18 to 79 years, with a median age of 45 years. Clinical data are depicted in [Table - 1]. IL-36γ was found to be expressed, mainly in the cells of granular and adjacent spinous layers, while claudin-1 and claudin-7 were found in all the layers of the epidermis [Figure - 1]a. Statistical analysis revealed that the percentage of cells positive for IL-36γ in the psoriasis group was markedly higher than that in the control group (P = 0.022) [Figure - 1]b. On the contrary, the percentage of cells positive for claudin-1 and claudin-7 in the psoriasis group was lower than the control group (P = 0.001, 0.001 for claudin-1 and claudin-7, respectively) [Figure - 1]b. In addition, the expression level of IL-36γ was negatively correlated with that of claudin-1 (r = −0.344, P = 0.025) and claudin-7 (r = −0.320, P = 0.039). We implemented logistic analysis to negate the effects of the confounding factors. No correlation was observed between age, sex, claudin-1, claudin-7, and psoriasis (P = 0.929, 0.075, 0.623 and 0.006, respectively), while psoriasis was found to be related to IL-36γ expression level (P = 0.039) [Table - 2].
 |
| Figure 1 |
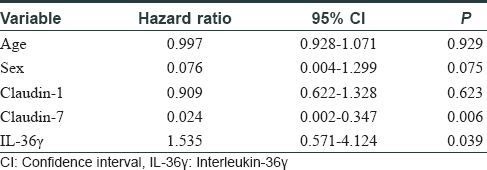
It is widely accepted that immune system plays an important role in the pathogenesis of psoriasis. Some recent studies have demonstrated IL-36 to be closely related to psoriasis. IL-36γ, in particular, was found to be raised in the lesional skin as well as in the blood, in patients having active psoriasis. Our study also showed that the expression level of IL-36γ was significantly higher in the psoriasis group compared to that in the control group (P = 0.022) [Figure - 1]b, and it played an important role in the activity of psoriasis [Table - 2]. The alterations in tight junction in the psoriatic skin occurs with respect to the distribution and expression levels of proteins, of which claudin-1 and claudin-7 are decreased. Our study revealed that the expression of claudin-1 and claudin-7 in the psoriatic skin was lower compared to that in the control group (P = 0.001) [Figure - 1]b. Studies have demonstrated that these alterations might be associated with the pathophysiological changes, which could lead to an attempt to repair the skin barrier. This may promote hyperproliferation of epidermis and further dysfunction of barrier.[5] We found significant negative correlations between the expression levels of IL-36γ and each of claudin-1 and claudin-7. We speculated that IL-36γ, like IL-1β, activates similar intracellular signalling pathways. This leads to decreased expression of claudin-1 and claudin-7, resulting in impaired skin barrier. It is suggested that treatments targeted to decrease IL-36 levels might restore the expression of claudin-1 and claudin-7, which will in turn improve the epidermal hyperproliferation and barrier dysfunction in psoriasis. However, further studies are necessary to prove this correlation and whether psoriasis patients could actually benefit from IL-36 inhibitors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Acknowledgment
We thank Bo Hong for helping with technical assistance.
Financial support and sponsorship
This work was supported by the National Natural Science Foundation of China (grant no. 81673045).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Bäsler K, Brandner JM. Tight junctions in skin inflammation. Pflugers Arch 2017;469:3-14.
[Google Scholar]
|
| 2. |
Kirschner N, Poetzl C, von den Driesch P, Wladykowski E, Moll I, Behne MJ, et al. Alteration of tight junction proteins is an early event in psoriasis: Putative involvement of proinflammatory cytokines. Am J Pathol 2009;175:1095-106.
[Google Scholar]
|
| 3. |
Watson RE, Poddar R, Walker JM, McGuill I, Hoare LM, Griffiths CE, et al. Altered claudin expression is a feature of chronic plaque psoriasis. J Pathol 2007;212:450-8.
[Google Scholar]
|
| 4. |
D'Erme AM, Wilsmann-Theis D, Wagenpfeil J, Hölzel M, Ferring-Schmitt S, Sternberg S, et al. IL-36γ (IL-1F9) is a biomarker for psoriasis skin lesions. J Invest Dermatol 2015;135:1025-32.
[Google Scholar]
|
| 5. |
Wolf R, Orion E, Ruocco E, Ruocco V. Abnormal epidermal barrier in the pathogenesis of psoriasis. Clin Dermatol 2012;30:323-8.
[Google Scholar]
|
Fulltext Views
3,625
PDF downloads
1,949





