Translate this page into:
Eosinophilic dermatoses (exaggerated insect bite-like reaction) associated with hematological malignancy: Report of three cases
Correspondence Address:
Norma Cameli
Department of Dermatology, San Gallicano Institute, IRCCS, Via Elio Chianesi, 53, 00144 Roma
Italy
| How to cite this article: Mariano M, Cavallotti C, Muscardin L, Cameli N. Eosinophilic dermatoses (exaggerated insect bite-like reaction) associated with hematological malignancy: Report of three cases. Indian J Dermatol Venereol Leprol 2018;84:93-95 |
Sir,
Exaggerated insect bite-like reaction, which is a synonym of eosinophilic dermatoses of hematological malignancy,[1] is a rare, disturbing and nonspecific skin condition often associated with hematoproliferative disorders. Skin lesions are characterized by itchy papules and often painful lesions, predominately on the limbs, which sometimes become bullous and often recur. The typical clinical–pathological findings include papules, plaques, vesiculo-bullous lesions, and a dense eosinophil-rich infiltrate mainly in the dermis. These eruptions have been described in patients with chronic lymphocytic leukemia, B cell lymphoproliferative diseases, and occasionally in acute lymphoblastic leukemia and mantle cell and large cell lymphoma.[2]
We present three cases of exaggerated bite-like eruptions in patients affected with malignant hematologic neoplasms. All three patients were females and had been referred to our outpatient department at San Gallicano Dermatological Institute of Rome from January through April 2016.
The first patient (75-year-old) had a non-Hodgkin's lymphoma. Eight weeks after chemotherapy, she developed bullous, itchy lesions, between 1 and 5 cm in diameter, with serous content on the lower limbs [Figure - 1].
 |
| Figure 1: Large bullae on the heel in a 75-year-old patient with a non-Hodgkin lymphoma |
The second patient (73-year-old), suffering from chronic lymphocytic leukemia, developed itchy serous bullous lesions on the lower limbs and hands. These were less than 4 cm in diameter and were prone to spontaneous rupture 2 months after the start of chemotherapy.
The third patient had a chronic lymphocytic leukemia too, and developed itchy papules and vesiculo-bullous eruptions, between 0.5 and 4 cm in diameter, localized to the lower limbs [Figure - 2].
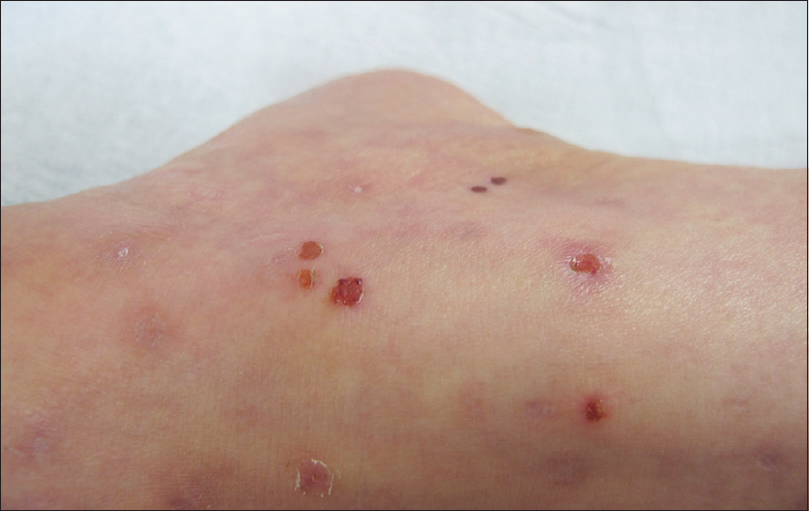 |
| Figure 2: Excoriated erythematous papules and vesicles on the lower leg in a patient with chronic lymphocytic leukemia |
Laboratory tests revealed a moderate peripheral eosinophilia (900 cells/μl) only in the first patient. Antibodies against desmoglein 1 and 3, the bullous pemphigoid antigen, and direct immunofluorescence were negative in all the samples. Histological examination showed subepidermal edema and superficial and deep perivascular and interstitial inflammatory infiltrates composed of numerous eosinophils in all the skin specimens [Figure - 3]. A diagnosis of eosinophilic dermatoses (exaggerated insect bite-like reaction) associated with hematological malignancy was made.
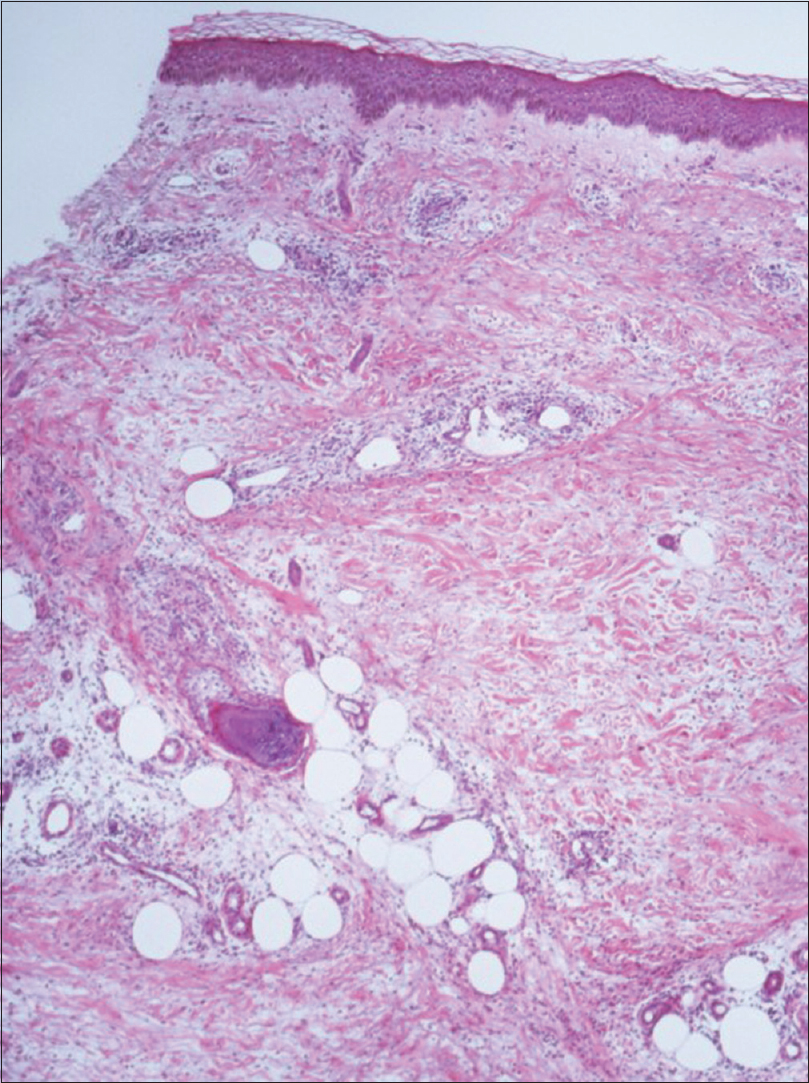 |
| Figure 3: Subepidermal edema and superficial, deep, and interstitial perivascular inflammatory infiltrates (H and E, ×400) |
Exaggerated insect bite-like reaction was first described by Weed in 1965[3] as a condition presenting with lesions >20 mm in diameter and characterized by erythema, edema, and intense pruritus at the site of a known mosquito bite or with evidence of a central punctum. These lesions usually occur in association with or preceding chronic lymphocytic leukemia, but cases have been described in other hematological malignancies, like B cell lymphoproliferative diseases and occasionally in acute lymphoblastic leukemia and mantle cell and large cell lymphoma.[2] Bite reactions have been described in other conditions causing immune dysregulation, such as human immunodeficiency virus infection and congenital agammaglobulinemia.[4]
Skin lesions usually appear months to years after the diagnosis of leukemia or less frequently may precede it, and are unrelated to laboratory findings, disease course, or therapy. In most cases the bites were thought to be from mosquitoes, but reported cases in literature have revealed that most patients did not remember being bitten and were avoiding any outdoor activity or were using an insect repellent.[2],[4] Besides, the reported lesions were not restricted to exposed sites and did not have any seasonal variation showing the possibility that many lesions were not triggered by a bite. So it has been proposed that this condition should be named “insect bite-like reaction or eosinophilic eruption of hematological malignancy.”[2] In our three cases, the patients did not recall being bitten by insects and the lesions had started to appear during wintertime and were localized to non-exposed areas. The pathogenesis is unclear, but an altered immune response stimulating the development of eosinophilic skin infiltrates is postulated.
Occasionally, the clinical and histological presentation could be similar to Wells syndrome.[5] Wells syndrome may be induced by a broader variety of stimuli including parasitic, fungal and streptococcal infections, insect bites, and is occasionally associated with hematological malignancies. It clinically presents as an acute edematous erythema resembling cellulitis with spontaneous morphea-like resolution, occasionally nodules or blisters, and may be accompanied by arthralgia, malaise, and fever.
In our patients, the clinical and histological findings were consistent with exaggerated bite-like reactions; no morphea-like resolution was observed, and on histology, the presence of vasculitis and the absence of flame figures were not characteristic of Wells syndrome. Differential diagnosis was also made of specific cutaneous lesions of chronic lymphocytic leukemia, bullous pemphigoid, and pemphigus vulgaris.
Systemic steroid (prednisone 40 mg/day or more) together with oral antihistamine was a successful mode of therapy for all our patients.
Knowing the clinical and histological aspects of exaggerated insect bite-like reactions is important for a proper and early diagnosis and could be helpful in detecting associated hematologic malignancies if not yet been diagnosed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Farber MJ, La Forgia S, Sahu J, Lee JB. Eosinophilic dermatosis of hematologic malignancy. J Cutan Pathol 2012;39:690-5.
[Google Scholar]
|
| 2. |
Dodiuk-Gad RP, Dann EJ, Bergman R. Insect bite-like reaction associated with mantle cell lymphoma: A report of two cases and review of the literature. Int J Dermatol 2004;43:754-8.
[Google Scholar]
|
| 3. |
Weed RI. Exaggerated delayed hypersensitivity to mosquito bites in chronic lymphocytic leukemia. Blood 1965;26:257-68.
[Google Scholar]
|
| 4. |
Barzilai A, Shpiro D, Goldberg I, Yacob-Hirsch Y, Diaz-Cascajo C, Meytes D, et al. Insect bite-like reaction in patients with hematologic malignant neoplasms. Arch Dermatol 1999;135:1503-7.
[Google Scholar]
|
| 5. |
Misago N, Okwa T, Tanaka M, Narisawa Y. Eosinophilic cellulitis (Wells' syndrome) and an insect bite-like reaction in a patient with non-Hodgkin B cell lymphoma. Eur J Dermatol 2011;21:422-3.
[Google Scholar]
|
Fulltext Views
5,057
PDF downloads
3,722





