Translate this page into:
Myelodysplasia in a psoriasis patient receiving etanercept: Cause or coincidence?
2 Department of Hematology, Al Hada Armed Forces Hospital, Taif, Kingdom of Saudi Arabia
3 Department of Clinical Pathology, Faculty of Medicine, Menoufia University, Menoufia, Egypt
4 Department of Clinical Pharmacy, Faculty of Pharmacy, Cairo University, Giza, Egypt
Correspondence Address:
Noha Mohammed Dawoud
Department of Dermatology, Al Hada Armed Forces Hospital, Taif 21944, PO Box 1347, Kingdom of Saudi Arabia
| How to cite this article: Dawoud NM, Ayoub OH, Essa ES, Dawoud DM. Myelodysplasia in a psoriasis patient receiving etanercept: Cause or coincidence?. Indian J Dermatol Venereol Leprol 2018;84:463-465 |
Sir,
Myelodysplastic syndrome comprises hemopoietic insufficiency, often associated with cytopenias of one or more cell lineages that may lead to leukemic transformation.[1] Here, we report a case of myelodysplastic syndrome in a psoriatic patient following therapy with tumour necrosis factor-α blocking agent (etanercept).
A 76-year-old male patient presented with psoriasis vulgaris since the last 20 years without any arthritis. He was treated with subcutaneous etanercept, 50 mg twice a week for 6 months followed by once a week for another 6 months, to achieve psoriasis area and severity index 90 (PASI90) at 6 months. Prior to etanercept, he had been treated with topical steroids, topical vitamin D analogues, 6-month course of narrow-band-ultraviolet-B and 1-year acitretin without any appreciable benefit.
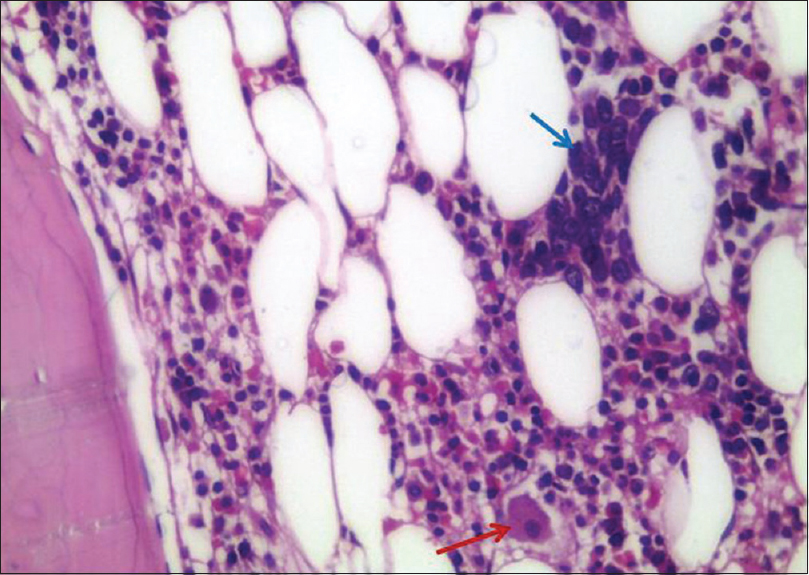
After one year of etanercept therapy, the patient presented to our emergency unit with spontaneous bluish bruising (ecchymosis) and recurrent epistaxis. A complete blood count recorded critically low platelet count (23 × 109/L), anemia (11.7 g/dl) and normal leukocyte count (6.6 × 109/L), with 0.5 × 109/L monocytes and 2% blasts. Reticulocyte count was 136 × 103 cells/mm 3, 3.4% (N = 0.8–2.5%) with low reticulocyte index, serum ferritin was 1280 ng/ml (N = 21.8–274.7 ng/ml) and folate was low at 1.7 ng/ml (N = 7–31.4 ng/ml), which indicated ineffective erythropoiesis [Table - 1].
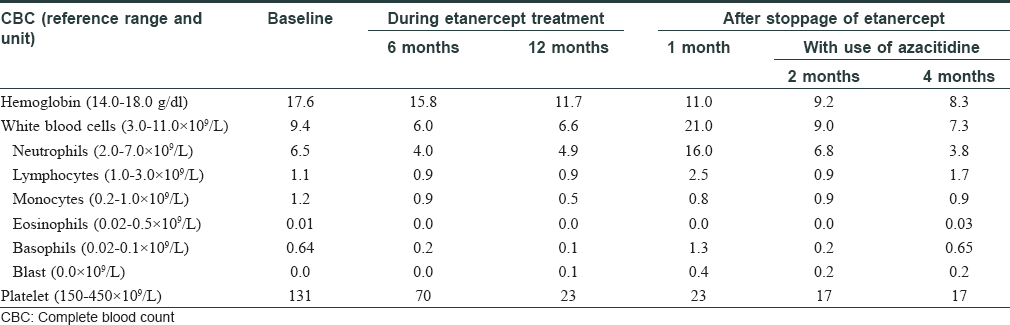
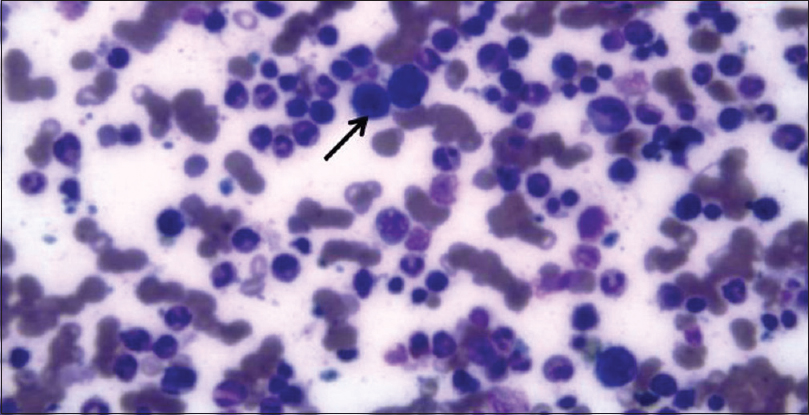
Bone marrow aspirate [Figure - 1] and biopsy [Figure - 2] revealed hypercellularity. Blast cells accounted for almost 8% of the total nucleated marrow cells. The majority of neutrophils were hypogranular. Hypolobulated megakaryocytes were observed. Reticulin fibres were not increased.
 |
| Figure 1: Bone marrow smear showing hypercellular bone marrow with hypolobated megakaryocytes (arrow) (×40) |
 |
| Figure 2: Bone marrow trephine biopsy showing hypolobated megakaryocyte (red arrow) and a cluster of abnormal localization of immature precursors (blue arrow) (×40) |
Peripheral blood also revealed bicytopenia, blasts and 0.5 × 109/L monocytes. Bone marrow showed 8% trilineage dysplasia and blasts. A diagnosis of myelodysplastic syndrome with excess blasts-1 was made based on the hematologic picture.
We stopped etanercept treatment and administered two cycles of azacitidin and folic acid supplementation, with almost no response and even worsening of platelet count (17 × 109/L) and hemoglobin (8.3 g/dl). While he was waiting for the third cycle, he was admitted to the emergency unit suffering from lower gastrointestinal bleeding, epistaxis and shock. The patient expired eventually due to cardiopulmonary arrest.
Immune dysregulation and altered T-cell hemostasis are essential factors for the development of myelodysplastic syndrome. Several authors have reported a higher risk of myelodysplastic syndrome in patients suffering from autoimmune disorders, resulting from chronic overproduction of apoptosis inducing cytokines like tumor necrosis factor-alpha. It has been proven that accelerated apoptosis of bone marrow cells accounts for the disturbed hemopoiesis and peripheral blood cytopenias leading to myelodysplastic syndrome, despite the presence of hypercellular bone marrow.[1] In addition, nonspecific activation and proliferation of T lymphocytes seen in myelodysplastic syndrome has been documented to promote epidermal growth in genetically susceptible psoriasis patients.[2]
Myelodysplastic syndrome may be associated with psoriasis in about 7% of cases.[3] Özbek et al. reported a 3.5-year-old girl with psoriasis, hypogammaglobulinemia and pancytopenia who developed myelodysplastic syndrome-excess blasts that progressed to acute myeloid leukemia.[2] Moreover, Maleszka et al. noted increased incidence of leukemia and laryngeal cancer among families of psoriasis patients.[4] In addition, there are some reported cases of leukemia that developed in psoriasis patients receiving systemic immunosuppressives (cyclosporine, methotrexate and etanercept). However, the association of leukemia and psoriasis is not well-investigated.[4]
Etanercept may induce various hematological side effects including pancytopenia and aplastic anaemia, as reported by the US Food and Drug Administration.[5] Tumor necrosis factor-alpha enforces apoptosis of tumor cells and promotes different antitumor activities like activation of natural killer cells, stimulation of CD8 cells and acceleration of camptothecan and etoposide antitumor effect. Loss of such activities may mediate tumor growth in acute and chronic myeloid leukemia.[6]
Tumor necrosis factor-alpha is also inhibitory to hematopoietic stem cells. Studies have shown increased levels of tumor necrosis actor-alpha in myelodysplastic syndrome marrow. Thus, antagonizing it significantly enhances in-vitro hematopoietic colony formation. Deeg et al. tried to treat myelodysplastic syndrome with etanercept as a pilot trial.[7] However, their study found limited favorable response in some patients and worsening of blood cell counts in others. The findings of Deeg et al. and the contradictory effects of tumor necrosis factor-alpha on dysplastic bone marrow suggest that tumor necrosis factor-alpha is only partially accountable for the dysregulated hemopoiesis in myelodysplastic syndrome; thus there are various other pathomechanisms for myelodysplastic syndrome.[7]
Only three cases of myelodysplastic syndrome have been reported till date in psoriasis patients following etanercept therapy, ours being the 4th case. Nair et al. reported the case of a 57-year-old man with psoriatic arthritis who developed myelodysplasia that progressed to acute myeloid leukemia after 6 months of etanercept treatment.[6] Bachmeyer et al.[8] and Knudson et al.[9] reported the cases of 40 and 43-year-old psoriatic males who were diagnosed with myelodysplastic syndrome after 4 and 14 months of etanercept therapy, respectively. The case reported by Knudson et al. had progressed to acute myeloid leukemia followed by death.[9] In addition to the aforementioned cases, another case was reported by Bakland and Nossent where a 31-year-old female with ankylosing spondylitis developed acute myeloid leukemia 4 months after etanercept treatment.[5] In our case, myelodysplasia with excess blasts developed 1 year after initiating etanercept therapy.
Taken together, the current case adds to the growing evidence that suggests a link between myelodysplastic syndrome and etanercept treatment in psoriasis patients. Pre-treatment thrombocytopenia was seen in our patient (131 × 109/L) and the patient reported by Knudson et al. (126 × 109/L)[9], while mild leucopenia (3.6 × 109/L) was reported by Bakland and Nossent before initiation of etanercept.[5] More studies are needed to clarify whether this was an accidental association or etanercept may aggravate myelodysplasia in all susceptible patients.
Although progressive and critical worsening of blood counts following etanercept treatment may demonstrate its aggressive hematologic and myelodysplastic adverse events, the susceptibility of psoriasis patients to myelodysplasia cannot be ruled out. Therefore, the present case and literature review support the need for pharmacovigilance, prospective cohort or retrospective case-control studies to prove or disprove this association.
In conclusion, psoriatic patients being treated with etanercept should be considered at dual risk of developing myelodysplastic syndrome – therapy-related and autoimmunity-associated. Hence, we recommend that psoriatic patients who are receiving etanercept should be followed regularly by routine blood counts and it should be discontinued upon onset of any cytopenias.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his clinical information to be reported in the journal. The patient understand that name and initials will not be published.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Voulgarelis M, Giannouli S, Ritis K, Tzioufas AG. Myelodysplasia-associated autoimmunity: Clinical and pathophysiologic concepts. Eur J Clin Invest 2004;34:690-700.
[Google Scholar]
|
| 2. |
Özbek N, Yazal Erdem A, Arman Bilir Ö, Karaca Kara F, Yüksek M, Yaralı N, et al. Achild with psoriasis, hypogammaglobulinemia, and monosomy 7-positive myelodysplastic syndrome. Turk J Haematol 2015;32:87-8.
[Google Scholar]
|
| 3. |
Komrokji RS, Kulasekararaj A, Al Ali NH, Kordasti S, Bart-Smith E, Craig BM, et al. Autoimmune diseases and myelodysplastic syndromes. Am J Hematol 2016;91:E280-3.
[Google Scholar]
|
| 4. |
Maleszka R, Paszkowska-Szczur K, Soczawa E, Boer M, Różewicka-Czabańska M, Wiśniewska J, et al. Psoriasis vulgaris and familial cancer risk- a population-based study. Hered Cancer Clin Pract 2013;11:6.
[Google Scholar]
|
| 5. |
Bakland G, Nossent H. Acute myelogenous leukaemia following etanercept therapy. Rheumatology (Oxford) 2003;42:900-1.
[Google Scholar]
|
| 6. |
Nair B, Raval G, Mehta P. TNF-alpha inhibitor etanercept and hematologic malignancies: Report of a case and review of the literature. Am J Hematol 2007;82:1022-4.
[Google Scholar]
|
| 7. |
Deeg HJ, Gotlib J, Beckham C, Dugan K, Holmberg L, Schubert M, et al. Soluble TNF receptor fusion protein (etanercept) for the treatment of myelodysplastic syndrome: A pilot study. Leukemia 2002;16:162-4.
[Google Scholar]
|
| 8. |
Bachmeyer C, Thiolière B, Khosrotehrani K, Cattan E. Acute myelogenous leukemia in a patient receiving etanercept for psoriasis. J Am Acad Dermatol 2007;56:169-70.
[Google Scholar]
|
| 9. |
Knudson RM, Tefferi A, Pittelkow MR, Davis MD. Development of myelodysplastic syndrome evolving to acute myeloid leukemia in a patient receiving etanercept for psoriasis. J Am Acad Dermatol 2011;65:673-4.
[Google Scholar]
|
Fulltext Views
2,654
PDF downloads
1,847





