Translate this page into:
Metronidazole as a monotherapy in the management of granulomatous cheilitis
2 Gokuldham Medical Center, Mumbai, Maharashtra, India
3 Department of Dermatology, MGM Medical College and Hospital, Mumbai, Maharashtra, India
Correspondence Address:
Swagata Tambe
19/558, Udyan Society, Nehru Nagar, Kurla East, Mumbai - 400 024, Maharashtra
India
| How to cite this article: Tambe S, Patil P, Modi A, Jerajani H. Metronidazole as a monotherapy in the management of granulomatous cheilitis. Indian J Dermatol Venereol Leprol 2018;84:491-495 |
Sir,
Granulomatous cheilitis, also known as orofacial granulomatosis, comprises a group of diseases characterized by noncaseating granulomatous inflammation affecting the soft tissues of the oral and maxillofacial region.[1] It is characterized by a chronic and relapsing course. Intraoral sites such as tongue, gingiva and buccal mucosa can also be affected rarely.[2] Various treatment modalities have been tried with variable success rates. Combination therapy with intralesional triamcinolone and clofazimine or dapsone is one of the most commonly used treatment options.[3] Other reported treatments include prednisone, hydroxychloroquine, sulfasalazine, antihistamines, tetracyclines, metronidazole, macrolides, thalidomide and infliximab; all of these have limitations of their own.
We report two cases of granulomatous cheilitis managed with metronidazole as a monotherapy. Metronidazole is cheap and easily available and associated with minimal side effects, even if taken for a longer duration.
Two females, aged 30 years and 10 years, presented with complaints of swelling of lips for 1 year and 6 months, respectively. In the first case, the swelling involved both the lips and was associated with diffuse facial swelling. In the second case, swelling was localized to the upper lip and gums.
Both the patients did not give history of precipitating factors such as seasonal variation, premenstrual flare, drug ingestion or change of residence prior to appearance of lesions. There was no history of any systemic symptoms suggestive of allergic contact dermatitis, angioedema or diffuse facial edema due to renal involvement in the first case.
Cutaneous examination in the first case revealed macrocheilia of both upper and lower lips with diffuse facial edema [Figure - 1] and [Figure - 2], whereas examination of the second case revealed macrocheilia of the upper lip with gingival hyperplasia [Figure - 3] and [Figure - 4]. On palpation in both the cases, lips were rubbery in consistency and nontender. Features such as facial palsy and scrotal tongue seen in Melkersson–Rosenthal syndrome were absent in both patients. The rest of the oral cavity examination was normal. There was no evidence of lymphadenopathy.
 |
| Figure 1: Macrocheilia of both upper and lower lips with diffuse facial edema in first patient |
 |
| Figure 2: Macrocheilia of upper and lower lips with fissuring and scaling |
 |
| Figure 3: Macrocheilia of upper lip with mild erythema and scaling in the second patient |
 |
| Figure 4: Macrocheilia of upper lip with gingival hyperplasia |
With a provisional diagnosis of granulomatous cheilitis, we investigated the patients. Both the patients' hemogram, blood sugar levels, biochemistry profile and X-ray chest were normal. Angiotensin converting enzyme levels were 26 U/L (Normal, 8–52 U/L) in the first case and 34 U/L (Normal, 8–52 U/L)] in the second case. Biopsy of the first patient revealed irregular hyperplastic epidermis, dermal edema and diffuse granulomatous inflammatory infiltrate in the upper and mid dermis [Figure - 5] and [Figure - 6]. The inflammatory infiltrate consisted of lymphocytes, epithelioid cells and multiple Langhans and foreign body type giant cells, suggesting the diagnosis of granulomatous cheilitis. Biopsy of the second patient revealed hyperplastic epidermis with multiple well-defined edematous granulomata in the upper and mid dermis consisting of lymphocytes, epithelioid cells and giant cells [Figure - 7] and [Figure - 8]. Patch test was not done in either of the patients.
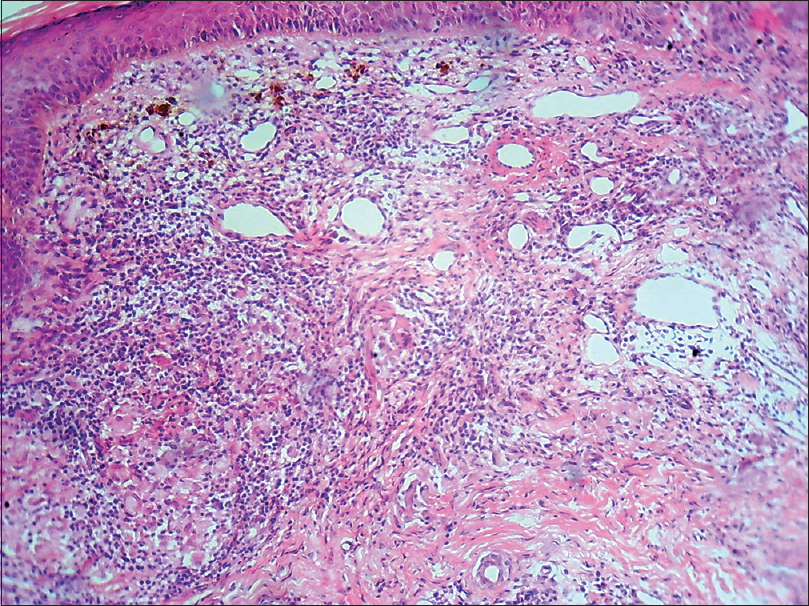 |
| Figure 5: Dermal edema and diffuse granulomatous inflammatory infiltrate in the upper and mid dermis consisted of lymphocytes, epithelioid cells and giant cells (Hematoxylin and Eosin, ×100) |
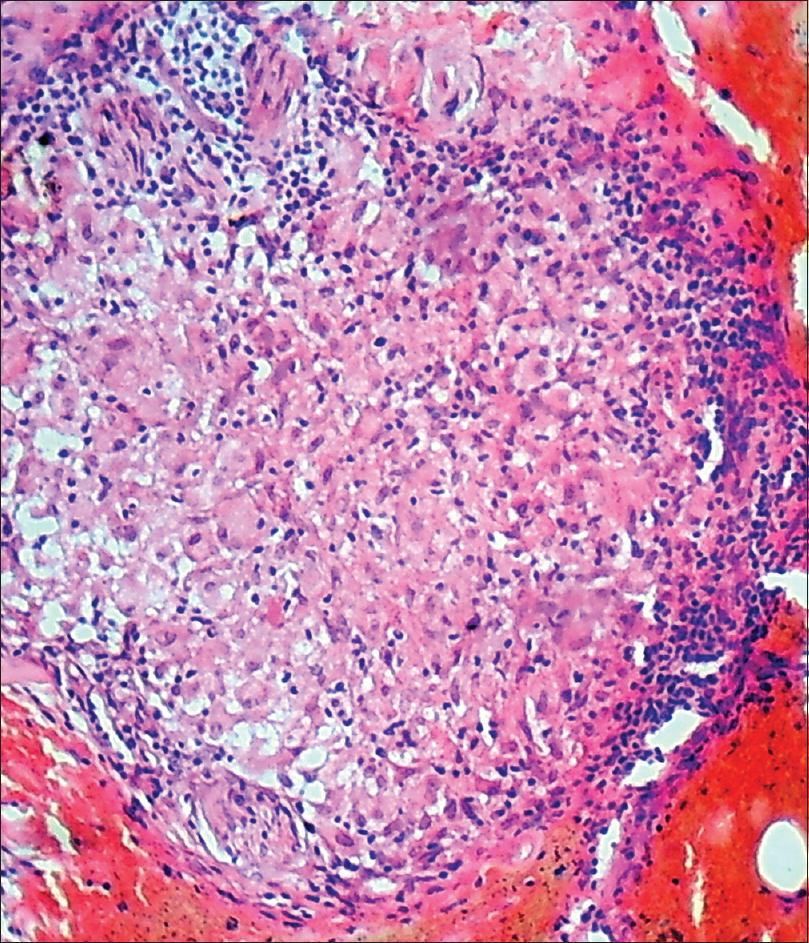 |
| Figure 6: Inflammatory infiltrate consisted of multiple giant cells, epithelioid cells and lymphocytes (Hematoxylin and Eosin, ×400) |
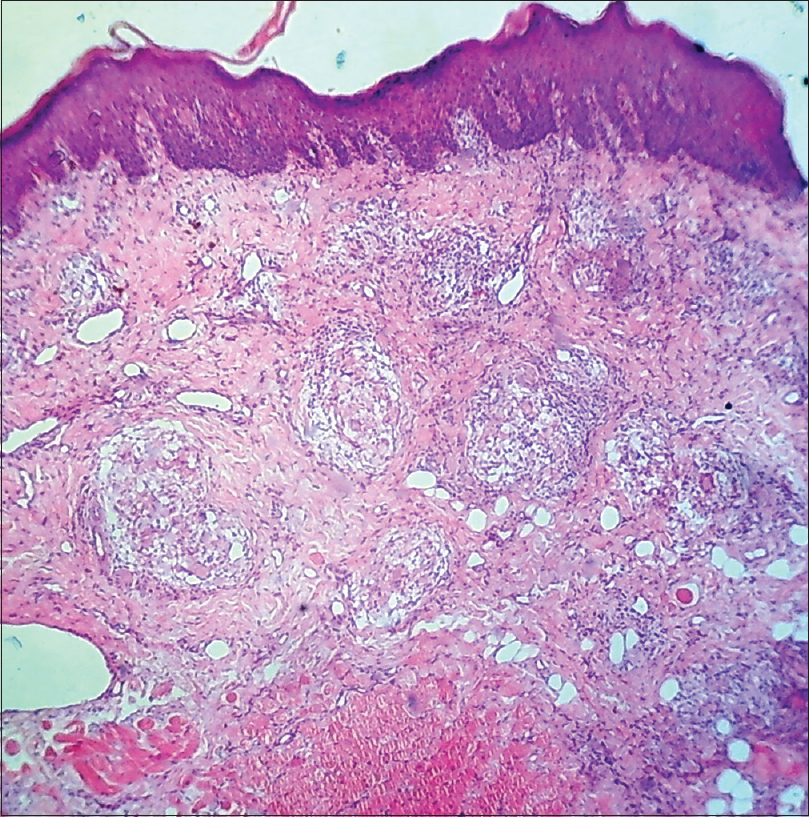 |
| Figure 7: Hyperplastic epidermis with multiple well-defined edematous granuloma in the upper and mid dermis (Hematoxylin and Eosin, ×400) |
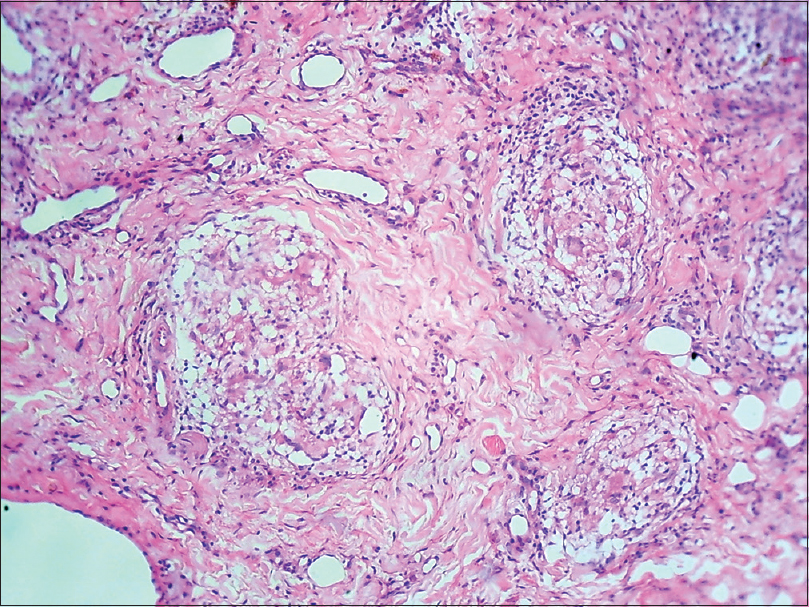 |
| Figure 8: Granuloma consisting of epithelioid cells, giant cells and lymphocytes (Hematoxylin and Eosin, ×100) |
Both patients were treated with metronidazole 400 mg three times a day for 2 months initially and then twice daily for 2 months and finally once daily for 2 months. The second patient underwent gingivoplasty in addition to oral metronidazole. Both patients showed excellent response to the treatment without side effects and recurrence, enabling us to stop the treatment completely [Figure - 9], [Figure - 10], [Figure - 11]. Both patients did not show any recurrence 8 months and 5 months after discontinuation of treatment, respectively.
 |
| Figure 9: Improvement after treatment in the first patient |
 |
| Figure 10: Improvement in lip swelling after treatment in the second patient |
 |
| Figure 11: Reduction in gingival hyperplasia in the second patient after treatment with metronidazole and gingivoplasty |
Granulomatous cheilitis, described by Meischer in 1945, is defined as a painless chronic recurrent swelling of the lips secondary to lymphatic obstruction by granulomatous proliferation. It is the most common monosymptomatic form of Melkersson–Rosenthal syndrome. Melkersson–Rosenthal syndrome is a rare disease characterized by the classical triad of edema of the lips and/or face, fissured tongue (lingua plicata) and relapsing peripheral facial nerve paralysis.[4]
The etiology of granulomatous cheilitis is poorly understood. Monoclonal lymphocytic expression secondary to chronic antigenic stimulation, cytokine production leading to granuloma formation and a cell-mediated hypersensitivity reaction have been suggested. Various factors such as genetic, allergic, infectious odontogenic foci, autoimmune mechanism and association of systemic diseases, such as Crohn's disease, sarcoidosis and Wegener's granulomatosis, have been implicated. Various substances such as chocolates, food additives, cinnamon compounds, benzoates, gold, mercury and nickel have been linked to the pathogenesis of the disease.[5]
Disease onset usually occurs in early adulthood with no sexual predilection. It is characterized by persistent, recurrent, diffuse, nontender, nonpitting, soft-to-firm swelling of one or both lips that eventually becomes permanent, leading to possible facial distortion. The typical course of granulomatous cheilitis is relapsing and remitting. Involvement of the upper lip is the most common, followed by the lower lip, cheeks, chin, periorbital region and eyelids. Involvement of the oral mucosa includes gingival hypertrophy, erythema, pain and erosions. The tongue may develop fissures, edema, paresthesia, erosions or taste alterations. Cobblestone appearance may be seen in the buccal mucosa, while papules, erosions and ulcers are seen on the palate.[6]
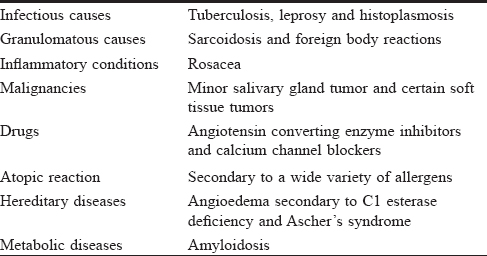
Histologically, the diagnosis lies in the demonstration of granuloma formation, consisting of collections of epithelioid histiocytes and Langhans giant cells. Differential diagnoses of granulomatous cheilitis are summarized in [Table - 1].[7]
Intralesional corticosteroids with or without immunomodulators are the first line of treatment followed by oral corticosteroids. However, relapses are common with the use of corticosteroids, and long-term treatment may be required. Second line treatment modalities include biologics (infliximab, adlimumab), clofazamine, oral corticosteroids with minocycline or metronidazole. Third line therapies include thalidomide, hydroxychloroquine, tranilast and danazol.[8] In severe or recalcitrant cases, cheiloplasty and radiotherapy are considered by some but are rarely needed.
In the first patient, we decided to start intralesional steroids and metronidazole but the patient was not willing to take intralesional steroids, hence, metronidazole was started as a monotherapy. As the patient showed significant improvement within 2 weeks of metronidazole monotherapy, oral and intralesional steroids were not added and metronidazole was continued. With this experience, the second patient was started on metronidazole monotherapy directly, and she also showed remarkable improvement.
Metronidazole is a nitroimidazole drug used as an antiprotozoal and antibacterial agent. Apart from its antimicrobial action, metronidazole has been found to have anti-inflammatory, immunosuppressive and anti-itching effects.[9] It induces a significant decrease in delayed-type hypersensitivity reaction, phagocytic activity (assessed by phagocytic capacity and phagocytic index) as well as tumor necrosis factor-alpha secretion by peritoneal macrophages. It has been used in chronic inflammatory conditions such as acne and rosacea. It has also been used in lichen planus with variable success, and has been suggested as an alternative therapy for cutaneous and oral lichen planus. Its effect in granulomatous cheilitis could be secondary to its anti-inflammatory effects.
Metronidazole has been found effective in granulomatous cheilitis in combination with oral steroids. This article highlights its effectiveness as a monotherapy which has not been mentioned before.[8] Considering the chronic nature of the disease, side effects of oral steroids and reluctance to taking intralesional steroids over lips and perioral area (as seen in our patients), monotherapy with metronidazole appears to be a good option.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sciubba JJ, Said-Al-Naief N. Orofacial granulomatosis: Presentation, pathology and management of 13 cases. J Oral Pathol Med 2003;32:576-85.
[Google Scholar]
|
| 2. |
Bansal M, Singh N, Patne S, Singh SK. Orofacial granulomatosis affecting lip and gingiva in a 15-year-old patient: A rare case report. Contemp Clin Dent 2015;6:S94-6.
[Google Scholar]
|
| 3. |
Sobjanek M, Michajłowski I, Zelazny I, Medrzycka-Dabrowska W, Włodarkiewicz A. What is the most effective treatment of cheilitis granulomatosa in Melkersson-Rosenthal syndrome? J Eur Acad Dermatol Venereol 2010;24:364-5.
[Google Scholar]
|
| 4. |
Muhammed K, Nandakumar G, Thomas S. Granulomatous cheilitis evolving into Melkersson-Rosenthal syndrome with bilateral facial palsy. Indian J Dermatol Venereol Leprol 2004;70:313-4.
[Google Scholar]
|
| 5. |
Muellegger RR, Weger W, Zoechling N, Kaddu S, Soyer HP, El Shabrawi-Caelen L, et al. Granulomatous cheilitis and Borrelia burgdorferi: Polymerase chain reaction and serologic studies in a retrospective case series of 12 patients. Arch Dermatol 2000;136:1502-6.
[Google Scholar]
|
| 6. |
Neville BW, Damm DD, Allen CM, Bouquot JE, editors. Oral and Maxillofacial Pathology. 2nd ed. Toronto, Canada: W.B. Saunders Company; 2002.
[Google Scholar]
|
| 7. |
Allen CM, Camisa C, Hamzeh S, Stephens L. Cheilitis granulomatosa: Report of six cases and review of the literature. J Am Acad Dermatol 1990;23:444-50.
[Google Scholar]
|
| 8. |
Lam C, Anderson BE. Granulomatous cheilitis. In: Lebwohl MG, Heymann WR, Berth-Jones J, Coulson I, editors. Treatment of Skin Disease e-Book: Comprehensive Therapeutic Strategies. 5th ed. China: Elsevier; 2018. p. 312-5.
[Google Scholar]
|
| 9. |
Nishimuta K, Ito Y. Effects of metronidazole and tinidazole ointments on models for inflammatory dermatitis in mice. Arch Dermatol Res 2003;294:544-51.
[Google Scholar]
|
Fulltext Views
9,040
PDF downloads
3,277





