Translate this page into:
An open uncontrolled trial of topical 5-aminolevulinic acid photodynamic therapy for the treatment of urethral condylomata acuminata in male patients
2 Department of Dermatology, Shandong Provincial Hospital for Skin Disease, Shandong University; Department of Dermatology, Shandong Provincial Institute of Dermatology and Venereology, 250022, Jinan, Shandong, China
3 Department of Dermatology, Shandong Provincial Hospital for Skin Disease, Shandong University, 250022, Jinan, Shandong, China
4 Department of Dermatology, Shandong Clinical College of Skin Diseases, Anhui Medical University; Department of Dermatology, Shandong Provincial Hospital for Skin Disease, Shandong University; Department of Dermatology, Shandong Provincial Institute of Dermatology and Venereology, 250022, Jinan, Shandong, China
Correspondence Address:
Furen Zhang
Shandong Provincial Institute of Dermatology and Venereology, 27397 Jingshi Road, Jinan, Shandong Province, 250022
China
| How to cite this article: Shan X, Wang N, Li Z, Hou J, Zheng R, Tian H, Zhang F. An open uncontrolled trial of topical 5-aminolevulinic acid photodynamic therapy for the treatment of urethral condylomata acuminata in male patients. Indian J Dermatol Venereol Leprol 2016;82:65-67 |
Sir,
Condyloma acuminatum or genital wart, one of the most prevalent sexually transmitted diseases, is caused by human papillomavirus infection. Urethral lesions are common and have been reported in upto 30% of men with genital warts;[1] they are difficult to treat for anatomical reasons and are associated with a high rate of recurrence. Conventional treatment options include cryotherapy, electrotherapy and CO2 laser; these methods are usually accompanied by bleeding, ulceration, pain and the risk of stricture.
Topical photodynamic therapy with 5-aminolevulinic acid is a promising method for proliferative diseases like actinic keratosis, Bowen's disease, in situ squamous cell carcinoma and superficial basal cell carcinoma. By itself, 5-aminolaevulinic acid is not photosensitizing, but it can be metabolized to the active photosensitizer protoporphyrin IX, via the heme biosynthesis pathway. When protoporphyrin IX is activated by light, photodynamic reactions occur that lead to cell necrosis and apoptosis. Studies demonstrate that condylomata acuminata can selectively accumulate the photosensitizer after the topical application of 5-aminolevulinic acid. When irradiated with light, lesions can be selectively destroyed by the photodynamic effect.
Our study protocol was approved by the institute review board of Shandong Provincial Institute of Dermatology and Venereology, Jinan, China. The study was open and uncontrolled; men with urethral condylomata acuminata were enrolled, the nature of the treatment and possible benefits and side effects were carefully explained to each patient before obtaining written consent for inclusion in the trial. Patients who had been treated using other local methods within the previous one month period were excluded from the study.
A solution of 20% 5-aminolevulinic acid (Fudan Zhangjiang Bio-Pharm Co., Ltd., Shanghai, China) dissolved in 0.9% NaCl was prepared. A 2 cm long, thin cotton swab soaked in this solution was gently inserted into the urethra to make close contact with the urethral lesions. If the patient had multiple lesions with involvement of the external urethral orifice, cotton soaked in the solution was placed on the surface of lesions. Subsequently, preservative film was used to occlude the lesions for 3 hours. The lesions were irradiated with light of wavelength 635 nm emitted by a cylindrical semiconductor laser fiber; the fiber was gently inserted into the urethra and the lesion was treated for 20 minutes at 100 mW/cm 2 [Figure - 1]. Lesions involving the external urethral orifice were irradiated with a wavelength of 633 nm, emitted by a light emitting diode lamp, for 20 minutes at 100 mW/cm 2. No local anesthetics were used during treatment and patients were advised to drink a lot of water after treatment.
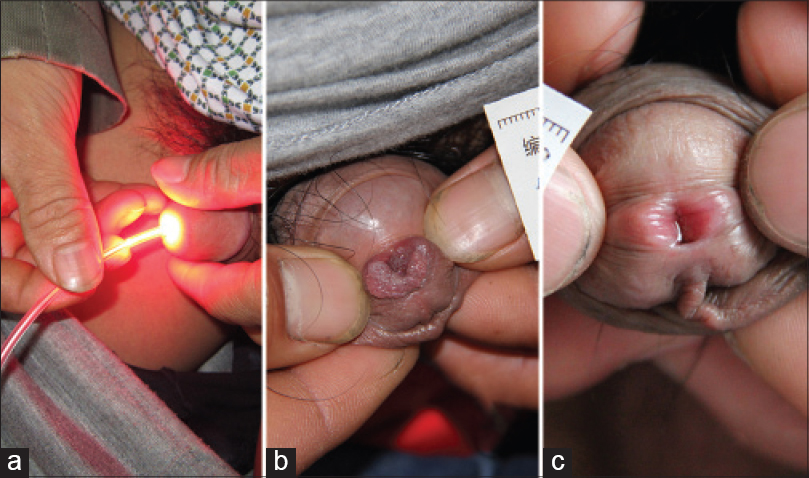 |
| Figure 1: (a) Insertion of cylindrical semiconductor laser fiber into the urethra to irradiate the lesions Urethral condylomata acuminata (b) before and (c) after four photodynamic therapy cycles |
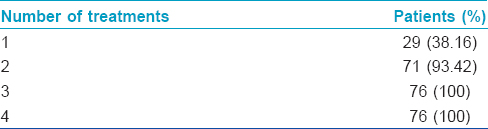
Patients were treated once every week for 4 weeks. The treatment response was evaluated one week after each treatment to determine whether or not the lesions were completely cleared. Patients were followed up for 3 months after the completion of treatment. A recurrence was defined as any reappearance of lesions after achieving complete remission. Any adverse events experienced by the patients during the study period were recorded by medical personnel.
A total of 76 men (16–65 years old, mean age 32.6) with urethral condylomata acuminata were enrolled in this study. These patients visited our sexually transmitted diseases clinic between 2012 and 2013 and none of them had any other concomitant sexually transmitted diseases including human immunodeficiency virus infection. Sexual partners of these patients were neither examined nor treated. All the studied patients had lesions inside the urethra that were 0.5–1.5 cm away from the external urethral orifice. Fifteen patients additionally had lesions located at the external urethral orifice. The duration of lesions ranged from 1 to 9 months (mean, 3.6 months). After three sessions of photodynamic therapy, complete clearance of condylomata acuminata was achieved in all patients [Table - 1]. Of these, 29 (38.2%) patients only needed one session of treatment, 42 (55.3%) patients needed two sessions and 5 (6.6%) patients needed three sessions for complete clearance. At the 3-month follow up, 5 (6.6%) patients relapsed. Three of the patients who relapsed received four more sessions of photodynamic therapy resulting in clearance of lesions without further recurrence during the subsequent follow up period of 3 months. The remaining two patients refused photodynamic therapy and opted for other treatments.
Adverse events were tolerable and transient. Almost all patients experienced mild burning/stinging sensation during irradiation; this discomfort persisted during urination for 1–2 days after treatment. Seven patients reported moderate pain, which was addressed by reducing the irradiance to 80 mW/cm 2; local anesthetics and sedatives were not required. No patient experienced any other complications such as bleeding, infection, ulcers, scarring or stricture.
Traditional treatment options for condylomata acuminata including cryotherapy, electrosurgery and CO2 laser are associated with high recurrence rates. Cryotherapy for condylomata acuminata is reported to have clearance rates of 44–75% and recurrence rates of 21–42%. Although electrosurgery and CO2 laser therapy have clearance rates approaching 100%, recurrence rates of 22% and 19–33%, respectively, have been reported.[2],[3] Moreoever, these treatments are associated with the risk of significant bleeding, ulceration and scarring.
Cells infected by human papillomavirus are proliferating rapidly and can selectively accumulate protoporphyrin IX unlike the surrounding non-infected cells. It has been shown that this selective photosensitization occurs not only in clinical lesions but also in subclinical infection.[4] When protoporphyrin IX is activated by light, reactive oxygen species are formed, especially singlet oxygen, which selectively induces necrosis and apoptosis of target cells.[5]
Similar observations and results have been reported by Li et al.[6] In their study, the complete clearance rate was 85.7% (48 of 56 patients) and the recurrence rate was 14.3% (8 of 56 patients) after 3 cycles of photodynamic therapy. To achieve a lower recurrence rate, in our study, we provided four treatment cycles to each patient regardless of clearance of lesions. Our approach was based on the premise that the high recurrence rate of condylomata acuminata stems from the unsuccessful clearance of virus from sites of subclinical and latent infection. Our results show that administering more treatment cycles could reduce the recurrence rate of genital warts in photodynamic therapy.
In patients infected with human immunodeficiency virus, genital warts usually grow more rapidly than in the immunocompetent and are often resistant to common therapeutic methods. Photodynamic therapy can be used in this scenario, too. Forty-one human immunodeficiency virus-infected patients with intra-anal warts were treated by a combination of CO2 laser and photodynamic therapy; after three treatment cycles, 39 cases showed no new or recurrent lesions and the remaining 12 (29%) had a recurrence by the end of the 6th month.[7]
The most common acute adverse effect encountered with photodynamic therapy is pain which, if severe, can make patients refuse treatment. It can be addressed by the use of low irradiance regimes or the use of cooling air and local anesthetics. As for long-term adverse effects, there is no definite proof that photodynamic therapy increases the risk of skin cancer. Our study shows that this technique is a simple, effective and safe therapeutic modality for urethral condylomata acuminata with the added advantage of a low recurrence rate.
| 1. |
Graverson PH, Bagi P, Rosenkildc P. Laser treatment of recurrent urethral condylomata acuminata in men. J Urol Nephrol 1990;24:163-5.
[Google Scholar]
|
| 2. |
Lacey CJ, Woodhall SC, Wikstrom A, Ross J. 2012 European guideline for the management of anogenital warts. J Eur Acad Dermatol Venereol 2013;27:e263-70.
[Google Scholar]
|
| 3. |
Blokker RS, Lock TM, de Boorder T. Comparing thulium laser and Nd:YAG laser in the treatment of genital and urethral condylomata acuminata in male patients. Lasers Surg Med 2013;45:582-8.
[Google Scholar]
|
| 4. |
Schneede P, Münch P, Wagner S, Meyer T, Stockfleth E, Hofstetter A. Fluorescence urethroscopy following instillation of 5-aminolevulinic acid: A new procedure for detecting clinical and subclinical HPV lesions of the urethra. J Eur Acad Dermatol Venereol 2001;15:121-5.
[Google Scholar]
|
| 5. |
Rai R. Phototherapy: An update. Indian J Dermatol Venereol Leprol 2009;75:634-7.
[Google Scholar]
|
| 6. |
Li J, Yi Y, Zhu W. Three stages of 5-aminolevulinic acid-photodynamic therapy for condyloma acuminatum of external urethral meatus. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2011;36:1115-9.
[Google Scholar]
|
| 7. |
Xu J, Xiang L, Chen J, He Q, Li Q, Li J, et al. The combination treatment using CO2 laser and photodynamic therapy for HIV seropositive men with intraanal warts. Photodiagnosis Photodyn Ther 2013;10:186-93.
[Google Scholar]
|
Fulltext Views
6,800
PDF downloads
1,418





