Translate this page into:
Multifocal spindle cell hemangioma: Report of two cases
2 Department of Dermatology, Pontificia Universidad Católica de , Santiago, Chile
3 Department of Radiology, Clínica Alemana de Santiago, Santiago, Chile
4 Department of Pathology, Clínica Alemana de Santiago, Santiago, Chile
Correspondence Address:
Camila Downey
4686 Vicuña Mackenna Avenue, Santiago
Chile
| How to cite this article: Kramer D, Downey C, Vargas P, Castro A. Multifocal spindle cell hemangioma: Report of two cases. Indian J Dermatol Venereol Leprol 2016;82:93-95 |
Sir,
Spindle cell hemangioma, formerly known as spindle cell hemangioendothelioma was first described in 1986 and was initially considered to be a low-grade angiosarcoma. In 1996, its benign behavior was recognised and the name spindle cell hemangioma was proposed.[1] It is a rare vascular proliferation, with less than 200 reported cases. The tumor originates from blood vessels and recently, lymphatic origin has been suggested.[2] The standard treatment is wide local excision but the the tumor has a high recurrence rate. We present two cases of multifocal spindle cell hemangiomas. One case was successfully treated with sclerotherapy suggesting that this can be an alternative treatment which is less invasive and has better long-term results.
The first case was a 10-year-old girl with a 4-year history of multiple violaceous and reddish cutaneous and subcutaneous nodules on the right ankle and foot [Figure - 1]. Magnetic resonance imaging performed to determine the extent of the lesions showed multiple hypervascular deep nodules in the left foot and ankle with irregular bone resorption. She was treated with sclerotherapy. The nodules were punctured under ultrasound guidance. Under angiographic monitoring, injection of 2% etoxisclerol foam was performed [Figure - 2] which lead to significant reduction in the volume of the lesions. There were no adverse effects and patient was asymptomatic at 2 years of follow up.
 |
| Figure 1: Multiple violaceous and reddish cutaneous and subcutaneous nodules on the right foot |
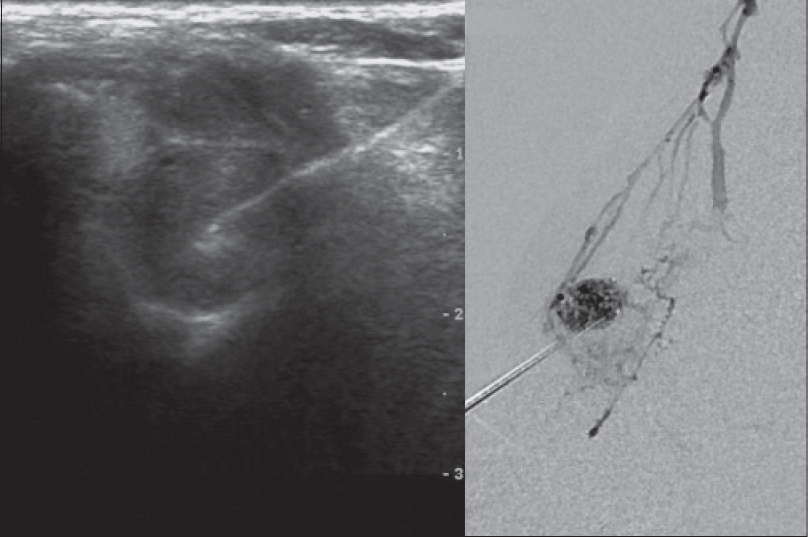 |
| Figure 2: Nodules were punctured under ultrasound guidance; and injection of 2% etoxisclerol foam was performed under angiographic visualisation |
The second case was an 18-year-old woman with multiple subcutaneous nodules located on the left upper extremity. Magnetic resonance imaging showed multiple hyperintense nodules on T2 in the left upper extremity and neck. Patient had undergone surgical removal of 12 nodules 4 years back, all of which had recurred in 18 months and new lesions continued to appear.
In both cases, no enchondromas were found in the affected bones ruling out Maffucci's syndrome. The histopathological findings in both patients showed nodular proliferation of thin-walled vascular structures lined by a single layer of endothelial cells with small nuclei of uniform appearance with some vessels showing dilation. Between the vascular spaces, fascicles of monomorphic spindle cells without nuclear atypia were present; these stained negatively for CD31 and positively for actin. Clusters of round cells with vacuolated cytoplasm positive for the CD31 were also seen [Figure - 3]. Immunohistochemistry for human herpes virus type 8 was negative ruling out Kaposi's sarcoma.
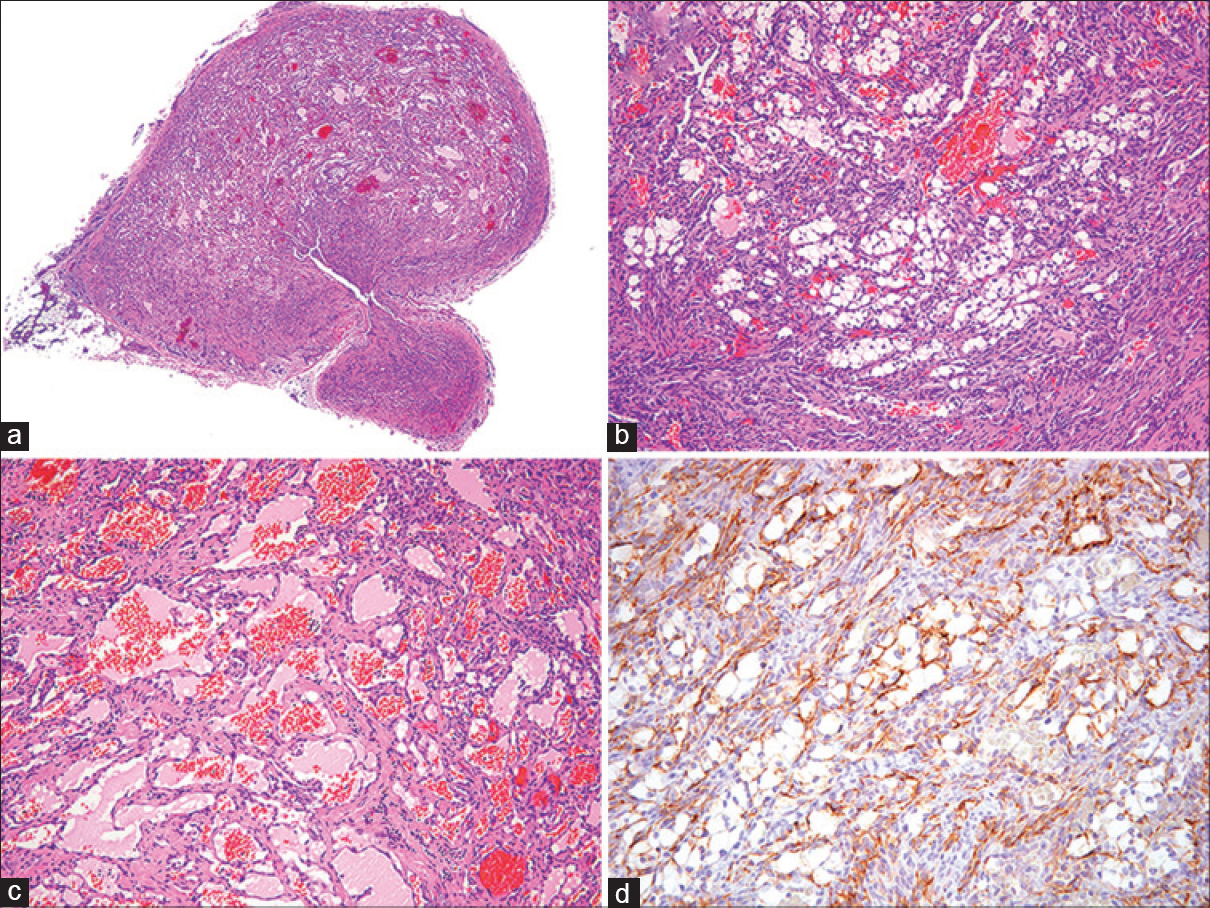 |
| Figure 3: (a) Well circumscribed nodule composed of dilated, thin-walled, blood vessels and fascicles of spindle cells (H and E; ×200) (b) The solid areas contain spindled cells with slit-like vascular spaces and plump rounded cells with vacuolated cytoplasm (H and E; ×100) (c) Vascular channels lined by a single layer of bland endothelial cells (H and E; ×200) (d) Endothelial cells and vacuolated rounded cells, but not spindled cells, stain for CD 31 (Immunostain; ×200) |
Spindle cell hemangioma is a rare, benign, vascular lesion which is more common in children and young adults, with no sex predilection. It presents mostly in the dermis and subcutaneous tissue of distal extremities. It has also been reported intramuscularly and exceptionally, it can affect the viscera such as the pancreas. Clinically it presents as a single, or sometimes multiple nodules that can be painful. These nodules are small, varying in size from 0.5 to 2.5 cm in diameter, skin colored or bluish, soft, firm in consistency and slow-growing. Multiple lesions have been associated with Maffucci's syndrome, a sporadically inherited genetic disorder where multiple spindle cell hemangiomas can be associated with phleboliths and multiple enchondromas.[3]
The histopathological findings show relatively well-circumscribed but non-encapsulated, dermal or subcutaneous nodules composed of thin-walled dilated vessels lined by flat endothelial cells, sometimes with thrombi or phleboliths in their lumina.[4] These areas alternate with areas of monomorphic spindle cells which are arranged in fascicles and have uniform, elongated, dark nuclei with eosinophilic cytoplasm. They do not show cytological atypia and mitotic figures are rarely found. There can be intravascular involvement. Variable numbers of epitheloid cells can also be present.
Immunohistochemistry shows that the cells lining the vascular spaces are positive for factor VIII-related antigen, CD31 and the hematopoietic progenitor cell antigen (CD34) markers. On the other hand, the spindle cells are negative for these markers and can be positive for actin supporting the mesenchymal origin of these cells.[4]
A recent study has shown the expression of homeobox transcription factor (Prox-1) and lymphatic endothelial cell marker podoplanin (D2-40) in these lesions, suggesting that these are proliferations of lymphatic origin.[2]
In the differential diagnosis, other vascular tumors should be considered such as epitheloid hemangiondothelioma, Kaposi's sarcoma and spindle cell angiosarcoma, among others.
The clinical course is typically indolent but in spite of its benign behavior, the development of new lesions in the same anatomical area after surgical treatment is >50%.[1] This phenomenon is considered by some authors not as recurrences but as new primaries.[1],[5] Successful treatment has also been reported with post-operative radiotherapy, low-dose intralesional interferon α-2b and intra-arterial administration of recombinant interleukin-2.[5]
It is important to recognize spindle cell hemangioma because aggressive treatment can be avoided. Even though the standard treatment is wide local excision, due to the high rate of recurrences, we propose sclerotherapy as an alternative management strategy that may provide satisfactory results.
Acknowledgment
The authors thank Carolina Whittle MD for her invaluable help with diagnostic imaging and reviewing of this manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Perkins P, Weiss SW. Spindle cell hemangioendothelioma. An analysis of 78 cases with reassessment of its pathogenesis and biologic behavior. Am J Surg Pathol 1996;20:1196-204.
[Google Scholar]
|
| 2. |
Wang L, Gao T, Wang G. Expression of Prox1, D2-40, and WT1 in spindle cell hemangioma. J Cutan Pathol 2014;41:447-50.
[Google Scholar]
|
| 3. |
Elston JB, Payne WG. Maffucci syndrome. Eplasty 2014;14:ic11. eCollection 2014.
[Google Scholar]
|
| 4. |
Tomasini C, Aloi F, Soro E, Elia V. Spindle cell hemangioma. Dermatology 1999;199:274-6.
[Google Scholar]
|
| 5. |
Tosios KI, Gouveris I, Sklavounou A, Koutlas IG. Spindle cell hemangioma (hemangioendothelioma) of the head and neck: Case report of an unusual (or underdiagnosed) tumor. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:216-21.
[Google Scholar]
|
Fulltext Views
4,560
PDF downloads
1,670





