Translate this page into:
Cognitive behavior therapy for psychosocial stress in vitiligo
2 Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
M Ramam
Department of Dermatology and Venereology, 4th Floor, Teaching Block, All India Institute of Medical Sciences, New Delhi
India
| How to cite this article: Jha A, Mehta M, Khaitan BK, Sharma VK, Ramam M. Cognitive behavior therapy for psychosocial stress in vitiligo. Indian J Dermatol Venereol Leprol 2016;82:308-310 |
Sir,
Vitiligo is associated with significant psychosocial burden and patients are likely to benefit from psychosocial interventions. In this study we utilized an intervention module based on cognitive behavior therapy to relieve the psychosocial stress in vitiligo patients and tried to assess its feasibility in general dermatology practice.[1]
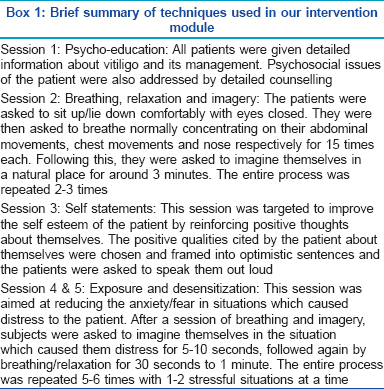
Approval of the institute ethics committee was obtained. The techniques used in our module were psychoeducation, relaxation/breathing with imagery, self-statements and exposure/desensitization as outlined in [Box 1]. It was administered to 13 vitiligo patients who were more than 12 years of age with moderate to severe psychosocial problems, based on subjective assessment. Five weekly sessions were given by a dermatology trainee (AJ) who had undergone training in the practical aspects of cognitive behavior therapy with a clinical psychologist (MM), and the first few sessions were conducted under the latter's supervision. Study subjects continued to receive their ongoing medical treatment for vitiligo. During therapy, patients maintained daily mood charts. Behavioral assessment and quality of life evaluation using the Dermatology Life Quality Index and Skindex-16 were done at baseline, at the end of 5 sessions and 7 weeks after therapy. Behavioral assessment is a qualitative questionnaire used to guide the psychosocial therapy in individual patients. It was carried out by the researcher, with patients mentioning positive and negative qualities about themselves, distressing situations, coping strategies and thoughts about self and illness. Clinical photographs of the skin lesions were taken at baseline and at the end of therapy. All the patients received individual psychosocial therapy.
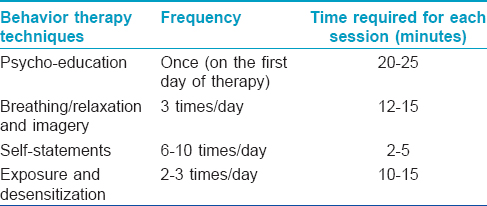
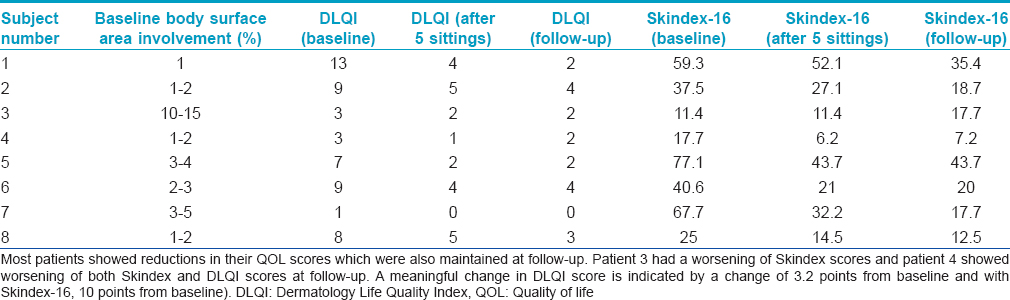
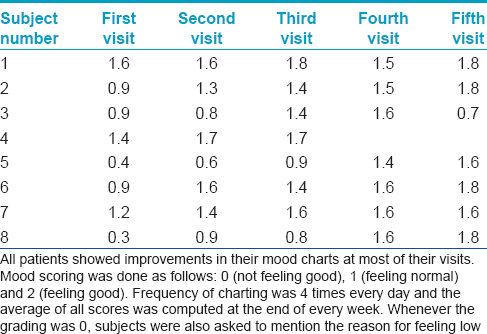
Nine men and 4 women of mean age 25.8 ± 6.3 years were studied. The frequency of, and time required for each behavioral intervention are outlined in [Table - 1]. All our patients experienced a feeling of relief and reduced anxiety following the first session of psychoeducation. Two (15.3%) patients were lost to follow-up after the first visit and three (22.8%) patients withdrew from the study. Eight (61.5%) patients completed the 5 sessions of psychosocial intervention and the additional 7 weeks of follow-up. All of them had a reduction in the Dermatology Life Quality Index scores at the end of 5 sessions. The reduction was maintained in 7 of these patients at follow-up at 12 weeks'. This reduction was meaningfully different in four patients at the end of 5 sittings and at follow-up at 12 weeks. For one patient, the decrease was meaningfully different at follow-up but not at the end of 5 sessions. One patient had a worsening of the score at follow-up compared to the score at the end of 5 sessions. Five of the eight patients who completed the treatment had significant/meaningful reductions in their Skindex-16 scores at the end of 5 sessions which was maintained at follow-up. In one patient, the score remained the same at the end of 5 sittings but worsened at 12 weeks. One patient showed a non-significant reduction in the score at the end of 5 sittings, with worsening at follow-up [Table - 2]. There was an overall improvement in the mood charts at the end of the fifth sitting in 7 patients. One patient had worsening of the mood scores at the fifth visit which she attributed to an increase in the number of skin lesions at this time [Table - 3]. Five patients were given topical steroids, 3 received topical tacrolimus and 2 received topical PUVAsol with topical steroids. One patient received oral steroids and 1 received oral PUVA with a topical steroid initially and was later changed to oral PUVAsol due to compliance issues. At the end of therapy, one patient (subject 7) had 20–30% repigmentation and one (subject 3) had a 6–8% increase in the lesions. The remaining subjects did not show any change in their skin lesions.
Cognitive behavior therapy is an intervention which focuses on changing the maladaptive ways of thinking, feeling and behaving. Previous studies have shown that patients with vitiligo could benefit from cognitive behavior therapy in terms of coping and living with vitiligo.[2] It also prevents recurrence of depression and helps in maintenance of self-esteem and mood elevation even after formal therapy has ended.[2],[3],[4] Previous studies on vitiligo used 8 sessions at weekly intervals, each session lasting 1 hour [2] and 1.5 hours.[5] Individual-centered counseling was reported to show better results than group cognitive behavior therapy in a study.[5] Previous studies have used a certified counseling psychologist,[2] a clinical psychologist and nursing staff [4],[6] for providing the behavior therapy in various skin disorders including vitiligo.
Five of our patients did not complete the therapy stating time constraints, inability to come weekly and inappropriateness of therapy. We attribute this significant dropout to the use of an intervention which did not include medications. The unwillingness of patients to engage in a non-medication, multi disciplinary approach was also noted by Fortune et al.[4] However, patients who completed the treatment were self-motivated and had a better understanding about their disease.
Rendering a psychosocial intervention in routine dermatology practice requires training the dermatologist and cognitive behavior therapy requires multiple, long sessions. The feasibility of such therapy would depend upon the willingness and ability of both the dermatologist and the patient to set aside the time required. Interventions with less frequent sessions of shorter duration may ensure better patient compliance. Our study suffers from the limitations of a small sample size and lack of a control group. In addition, though a significant number of vitiligo patients had psychosocial issues, only some chose to undergo cognitive behavior therapy because they lacked understanding about its usefulness, pointing to the need for education about the role of psychosocial treatment in routine clinical practice. We recommend that all vitiligo patients be given information about the disease as it reduces stress. Those having greater degrees of stress should be identified and may be provided cognitive behavior therapy, if they are motivated and willing to attend therapy sessions regularly.
Acknowledgement
Prof A.Y. Finlay and Prof M.M. Chren gave permission to use the DLQI and Skindex-16, respectively for this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Pahwa P, Mehta M, Khaitan BK, Sharma VK, Ramam M. The psychosocial impact of vitiligo in Indian patients. Indian J Dermatol Venereol Leprol 2013t;79:679-85.
[Google Scholar]
|
| 2. |
Papadopoulos L, Bor R, Legg C. Coping with the disfiguring effects of vitiligo: A preliminary investigation into the effects of cognitive-behavioural therapy. Br J Med Psychol 1999;72(Pt 3):385-96.
[Google Scholar]
|
| 3. |
Price ML, Mottahedin I, Mayo PR. Can psychotherapy help patients with psoriasis? Clin Exp Dermatol 1991;16:114-7.
[Google Scholar]
|
| 4. |
Fortune DG, Richards HL, Kirby B, Bowcock S, Main CJ, Griffiths CE. A cognitive-behavioural symptom management programme as an adjunct in psoriasis therapy. Br J Dermatol 2002;146:458-65.
[Google Scholar]
|
| 5. |
Papadopoulos L, Walker C, Anthis L. Living with vitiligo: A controlled investigation into the effects of group cognitive-behavioural and person-centred therapies. Dermatol Psychosom 2004;5:172-7.
[Google Scholar]
|
| 6. |
Fortune DG, Richards HL, Griffiths CE, Main CJ. Targeting cognitive-behaviour therapy to patients' implicit model of psoriasis: Results from a patient preference controlled trial. Br J Clin Psychol 2004;43(Pt 1):65-82.
[Google Scholar]
|
Fulltext Views
4,878
PDF downloads
1,755





