Translate this page into:
Nail changes in psoriatic children
Correspondence Address:
Marjorie Uber
Av. Paraná, 1030, Apto 1103, Cabral, CEP 80.035-130, Curitiba, Paraná
Brazil
| How to cite this article: Uber M, Abagge KT, Robl R, Carvalho VO, Marinoni LP. Nail changes in psoriatic children. Indian J Dermatol Venereol Leprol 2016;82:314-316 |
Sir,
Nail abnormalities in children with psoriasis range from mild to extensive and severe, causing both functional and esthetic problems Their prevalence in children and adolescents with psoriasis and their relation to disease severity is poorly understood. We describe nail alterations found in 47 children with psoriasis.
This was an analytic cross-sectional study with prospective data collection. We included patients below 18 years of age with psoriasis who attended the outpatient pediatric dermatology clinic of Hospital de Clínicas in South Brazil from August 2013 to May 2014. The study was approved by the Ethics Committee on Human Research of the institute and informed consent was obtained from parents/guardians of each participant. All subjects were clinically assessed by the same investigator who performed a complete physical examination to determine the clinical form of the disease and calculated the Psoriasis Area and Severity Index (PASI). All 20 nails of each patient were evaluated, photographically documented and the Nail Psoriasis Severity Index score was calculated.
Statistical analysis was performed by Statistica software, Statsoft ® and JMP - SAS ® using Spearman correlation test for continuous variables and Mann–Whitney test for categorical variables. A correlation coefficient of 1.0 was indicative of perfect linear correlation and values were considered strong when situated between 0.80 and 1.00, moderate when between 0.50 and 0.80 and weak between 0.50 and 0.10.
Forty seven patients were included with a female: male ratio of 1.2:1. The median age was 10.4 years (range: 2.7– 16.1 years) and the median age at onset of symptoms was 5 years (range: 1 month–13.6 years). On clinical examination, the disease was classified as plaque psoriasis in 27 (57.4%) patients, guttate in 9 (19.1%), inverse in 8 (17%), erythrodermic in 3 (6.4%), nevoid in 2 (4.2%), palmoplantar in 2 (4.2%) and generalized pustular psoriasis in one (2.1%) patient. The scalp was involved in 35 (74.5%) patients while two (4.2%) patients showed psoriatic arthritis. Family history of psoriasis was reported in 14 (29.8%) cases. The median Psoriasis Area and Severity Index (PASI) score was 1.6 (0–18.7) and six patients had a score ≥5.0, considered indicative of systemic treatment, according to the National Psoriasis Foundation Consensus.[1] Two patients had a PASI score >10 of which one patient had erythroderma.
All patients had at least one type of nail change [Figure - 1]. Pitting was the most common change observed in 39 (83%) patients, followed by leukonychia in 26 (55.3%) and Beau's lines in 25 (53.2%) [Figure - 2]. Other changes such as longitudinal ridges, subungual hyperkeratosis and splinter hemorrhages [Figure - 2] occurred less frequently.
 |
| Figure 1: Prevalence of nail abnormalities in patients with psoriasis |
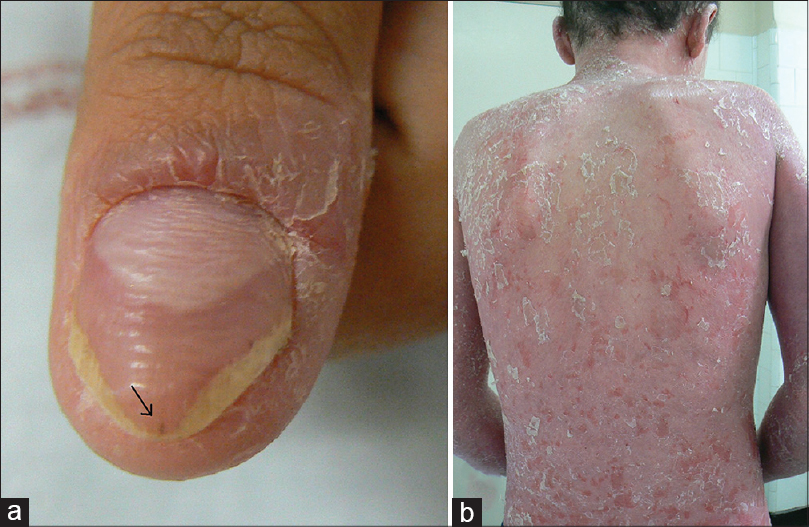 |
| Figure 2: (a) Beau's lines, splinter hemorrhage (arrow), hyperkeratosis and periungual desquamation. (b) Clinical lesion of the patient with severe erythrodermic psoriasis |
The median number of affected nails in each patient was 12 (range: 2–20) and the median Nail Psoriasis Severity Index score was 9 (range: 0–86). There was weak correlation between PASI score and the number of affected nails (correlation coefficient of 0.30) and between PASI score and Nail Psoriasis Severity Index (correlation coefficient of 0.39) [Figure - 3].
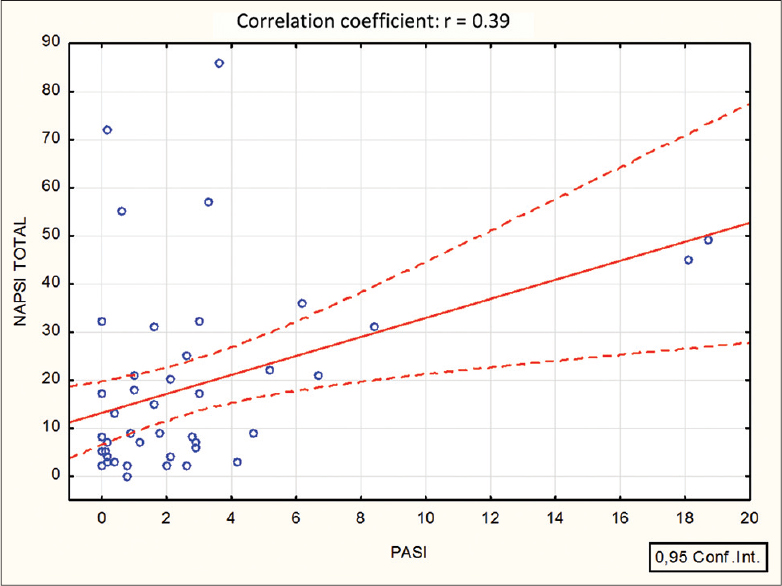 |
| Figure 3: Spearman correlation coeffi cient between Psoriasis Area and Severity Index and Nail Psoriasis Severity Index |
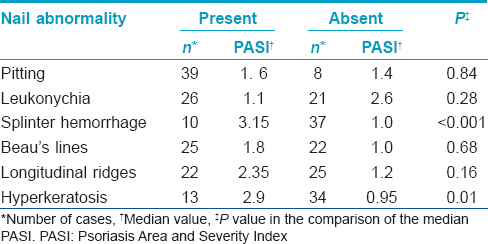
The relationship between the type of nail change and PASI score, by Mann–Whitney test, demonstrated that hyperkeratosis and splinter hemorrhages were found more frequently in patients with more severe disease (P = 0.01 and P < 0.001, respectively) [Table - 1].
In previous retrospective and questionnaire based studies, prevalence of nail involvement in children with psoriasis has been found to vary between 17% and 39%.[2],[3],[4],[5] In the present study, nail changes were found in all patients, stressing the importance of active evaluation and treatment of nail abnormalities in psoriatic patients.
The correlation coefficients between PASI and Nail Psoriasis Severity Index scores or between PASI and the number of affected nails were both weak. In a previous study, Al-Mutairi et al. also found no relation between the severity of nail changes and the extent or duration of illness.[5] Likewise, Mercy et al. assessed the severity of psoriasis through the physician's global assessment tool and also could not find any relation to the severity of nail changes.[2] In our study, hyperkeratosis and splinter hemorrhages were found to correlate positively with the severity of psoriasis and these findings should be corroborated by other studies.
Nail Psoriasis Severity Index as a tool for assessing the severity of psoriatic nail lesions has been used in adults but we were unable to find any previous reports of its use in children. In our study, the median Nail Psoriasis Severity Index score was 9. It is important to understand that Beau's lines and longitudinal ridges, which are common nail changes in children with psoriasis, are not included in Nail Psoriasis Severity Index score and some modification in the index may be necessary for this population. In pediatric populations, it is also necessary to determine which nail abnormalities are in fact due to psoriasis and relevant for diagnosis and which would be the best method for evaluating them since factors such as trauma or nail biting (common in children) can cause similar nail alterations.
Furthermore, other non-invasive and inexpensive tools such as dermoscopy and histopathology analysis of the nail clipping may be evaluated as adjuncts to clinical examination alone in further defining nail changes in pediatric psoriasis.
Limitations of our study include the small sample size, the absence of a control group and the evaluation method of nails by Nail Psoriasis Severity Index which is not adapted to children.
However, this study contributes to the scarce data found in the literature regarding nail alterations in childhood psoriasis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Pariser DM, Bagel J, Gelfand JM, Korman NJ, Ritchlin CT, Strober BE, et al. National Psoriasis Foundation clinical consensus on disease severity. Arch Dermatol 2007;143:239-42.
[Google Scholar]
|
| 2. |
Mercy K, Kwasny M, Cordoro KM, Menter A, Tom WL, Korman N, et al. Clinical manifestations of pediatric psoriasis: Results of a multicenter study in the United States. Pediatr Dermatol 2013;30:424-8.
[Google Scholar]
|
| 3. |
Kumar B, Jain R, Sandhu K, Kaur I, Handa S. Epidemiology of childhood psoriasis: A study of 419 patients from northern India. Int J Dermatol 2004;43:654-8.
[Google Scholar]
|
| 4. |
Tollefson MM, Crowson CS, McEvoy MT, Maradit Kremers H. Incidence of psoriasis in children: A population-based study. J Am Acad Dermatol 2010;62:979-87.
[Google Scholar]
|
| 5. |
Al-Mutairi N, Manchanda Y, Nour-Eldin O. Nail changes in childhood psoriasis: A study from Kuwait. Pediatr Dermatol 2007;24:7-10.
[Google Scholar]
|
Fulltext Views
3,807
PDF downloads
2,756





