Translate this page into:
Basal cell carcinoma overlying vitiligo attributable to phototherapy
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Somesh Gupta
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi
India
| How to cite this article: Bhari N, Sahni K, Verma KK, Khanna N, Arava S, Gupta S. Basal cell carcinoma overlying vitiligo attributable to phototherapy. Indian J Dermatol Venereol Leprol 2016;82:320-322 |
Sir,
A 54-year-old man with a 7 year history of vitiligo vulgaris presented with three pigmented plaques over pre-existing vitiliginous patches on his left shoulder and forehead [Figure - 1] and [Figure - 2].
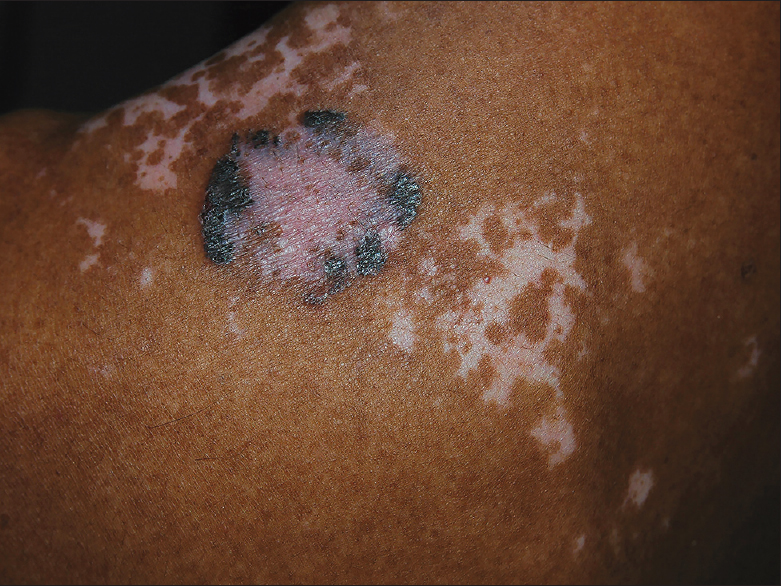 |
| Figure 1: Basal cell carcinoma over vitiligo patch on shoulder |
 |
| Figure 2: Basal cell carcinoma over vitiligo patches on forehead |
Five years prior to this presentation, he had received treatment with oral psoralen and ultraviolet-A radiation three times a week for 5 months for his vitiligo. The cumulative dose of psoralen plus ultraviolet-A could not be calculated as he had lost his medical records. One year following the psoralen and ultraviolet-A therapy, he developed an asymptomatic pigmented nodule on his left shoulder over a vitiligo patch [Figure - 1]. Three years later, he developed two similar lesions overlying pre-existing vitiliginous patches on the forehead [Figure - 2]. There was no history of prolonged sun-exposure, immunosuppression or occupational exposure to any carcinogenic agents such as arsenic. There was no family history of skin cancer.
A clinical diagnosis of pigmented basal cell carcinoma was made and was confirmed on skin biopsies which showed nodular aggregates of basaloid cells in the papillary dermis and the presence of melanophages in the aggregates as well as in the dermis [Figure - 3]a. For treatment, radioactive Re-188 patches were applied over the lesions on 5 alternate days for 80 minutes each. This was followed by erosion and crusting over the plaques which healed over 10 weeks. A hyperpigmented rim persisted. A follow-up biopsy at 12 weeks showed no evidence of malignancy [Figure - 3]b. The hyperpigmented area showed marked pigment incontinence. For the vitiligo, he was advised topical steroids with some improvement. There was no clinical recurrence of basal cell carcinoma at 1 year follow-up.
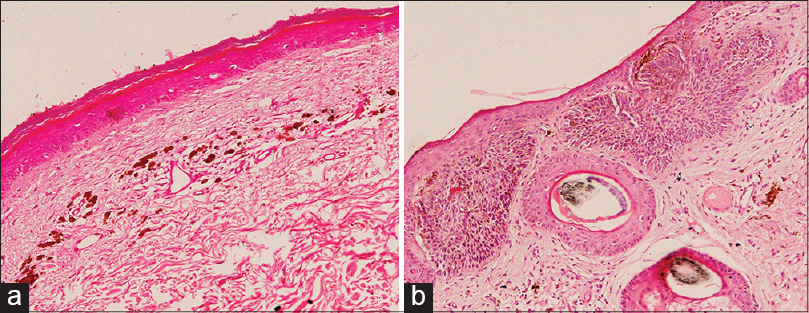 |
| Figure 3: Basal cell carcinoma: Histopathology before (a) and after treatment (b), (H and E, ×200) |
Patches of vitiligo are expected to be more vulnerable to ultraviolet light-induced phototoxicity and non-melanoma skin cancers due to the absence of melanin which protects against photodamage. However, this complication has been rarely noted even in long-standing cases. Overexpression of tumor suppressor gene P53 and its regulatory oncogene mouse double minute 2 (MDM2) homolog proteins in both normally pigmented and depigmented skin of patients with vitiligo is postulated to contribute to this protective effect.[1]
Squamous cell carcinoma and actinic keratosis have been previously reported on vitiliginous patches with prolonged sun-exposure. However, the development of basal cell carcinoma in these patches appears extremely rare; we were able to find only 3 previous reports.[2],[3],[4] In these patients, basal cell carcinomas appeared on vitiligo lesions over sun-exposed sites on the scalp, cheek and naso-labial fold. Two patients were Caucasian and one patient was Mexican-American. No specific predisposing factor could be demonstrated. Phototherapy was not given in any of these patients. Sun exposure or an unspecified spontaneous mutation were suspected as predisposing factors.
According to recent studies, psoralen and ultraviolet-A treatment is associated with a clearly dose-related increase in risk of non-melanoma skin cancer, mainly squamous cell carcinoma.[4] The risk of squamous cell carcinoma was significantly higher for patients exposed to high doses of psoralen plus ultraviolet-A (>200 sessions or 2000 J/cm 2). This dose relationship could not be established for basal cell carcinoma because of its rare occurrence. Ultraviolet radiation is the most important risk factor in the development of basal cell carcinoma. Ultraviolet light leads to the formation of thymine dimers and cumulative DNA damage resulting in various mutations. It also depresses the local immune system decreasing immune surveillance for new tumor cells.[5] This mechanism may explain phototherapy-induced basal cell carcinoma in vitiligo patients.
Multiple basal cell carcinomas are uncommon in the Indian population. In our patient, although inability to calculate the cumulative dose of psoralen plus ultraviolet-A makes its relationship with basal cell carcinomas speculative, localization of the tumour over vitiligo patches on sun exposed as well as non-sun exposed sites, the absence of any other known predisposing factor, as well as appearance 1 to 3 years after therapy raises the possibility that psoralen plus ultraviolet-A therapy was responsible. Other unknown factors such as spontaneous mutations may also play a role. Interestingly, the basal cell carcinomas in our patient were pigmented even though they developed over patches of vitiligo. Pigmented basal cell carcinoma contains melanin which is produced by melanocytes that colonize the tumor. These may have been derived from the mutation and proliferation of surviving epidermal melanocytes in the vitiligo patch and these tumor melanocytes may be resistant to the depigmenting factors present in that milieu.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Bakry OA, Hammam MA, Wahed MM. Immunohistochemical detection of P53 and Mdm2 in vitiligo. Indian Dermatol Online J 2012;3:171-6.
[Google Scholar]
|
| 2. |
Rustemeyer J, Günther L, Deichert L. A rare association: Basal cell carcinoma in a vitiliginous macula. Oral Maxillofac Surg 2011;15:175-7.
[Google Scholar]
|
| 3. |
Arnon O, Mamelak AJ, Goldberg LH. Basal cell carcinoma arising in a patient with vitiligo. J Drugs Dermatol 2008;7:1075-6.
[Google Scholar]
|
| 4. |
Hexsel CL, Eide MJ, Johnson CC, Krajenta R, Jacobsen G, Hamzavi I, et al. Incidence of nonmelanoma skin cancer in a cohort of patients with vitiligo. J Am Acad Dermatol 2009;60:929-33.
[Google Scholar]
|
| 5. |
Situm M, Buljan M, Bulat V, Lugović Mihić L, Bolanca Z, Simić D. The role of UV radiation in the development of basal cell carcinoma. Coll Antropol 2008;32 Suppl 2:167-70.
[Google Scholar]
|
Fulltext Views
2,124
PDF downloads
1,286





