Translate this page into:
Combined vitamin C sonophoresis and neodymium-doped yttrium aluminum garnet (NdYAG) laser for facial hyperpigmentation: An outcome observation study in Asian patients
2 Department of Plastic Surgery, Chiayi Chang Gung Memorial Hospital, Puzi; School of Medicine, China Medical University, Taichung, Taiwan; Institute of Imaging and Biomedical Photonics, National Chiao Tung University, Taiwan, ROC
3 Department of Ophthalmology, Tri-Service General Hospital, Taipei, Taiwan, ROC
4 Department of Ophthalmology, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan, ROC
5 Department of Dermatology, Chiayi Chang Gung Memorial Hospital, Puzi, Taiwan, ROC
6 Institute of Imaging and Biomedical Photonics, National Chiao Tung University; Department of Medical Research, Chi Mei Medical Center, Tainan, Taiwan, ROC
Correspondence Address:
Chang-Cheng Chang
Department of Plastic Surgery, Chiayi Chang Gung Memorial Hospital, No. 6, West Section, Chia-Pu Road, Puzi, Chiayi County 613, Taiwan, ROC. School of Medicine, China Medical University, No. 91, Hsueh-Shih Road, Taichung 40402, Taiwan, ROC. Institute of Imaging and Biomedical Photonics, National Chiao Tung University, Tainan 711, Taiwan
ROC
| How to cite this article: Chen YT, Chang CC, Hsu CR, Shen JH, Shih CJ, Lin BS. Combined vitamin C sonophoresis and neodymium-doped yttrium aluminum garnet (NdYAG) laser for facial hyperpigmentation: An outcome observation study in Asian patients. Indian J Dermatol Venereol Leprol 2016;82:587 |
Abstract
Background: The neodymium-doped yttrium aluminum garnet (NdYAG) laser therapy has been a popular technique for facial rejuvenation but certain adverse effects like post-inflammatory hyperpigmentation are issues of concern to Asian patients. Aims: To assess the outcome following combined treatment with vitamin C sonophoresis and NdYAG laser, in selected cases of facial hyperpigmentation. Methods: Twenty three women with dyschromia or melasma who had undergone five sessions of Q-switched NdYAG laser therapy followed by transdermal delivery of vitamin C via sonophoresis were selected after a retrospective review of case records. The objective and subjective clinical outcomes and the side effects, including erythema, scaling, pruritus, dryness and post-inflammatory hyperpigmentation were evaluated. Results: In both objective or subjective outcomes, 91.3% (21/23) of the patients showed an excellent or better outcome, while 8.7% (2/23) showed no change. A majority of the patients (73.9%, 17/23) experienced no post-inflammatory hyperpigmentation or had slight post-inflammatory hyperpigmentation which quickly resolved within 1 week. Only one (4.3%) patient had extreme post-inflammatory hyperpigmentation which lasted for over a month. Limitations: This was a retrospective study without a control group; a comparative study with a control group (patients treated with the laser alone, without vitamin C sonopheresis) is needed to determine the difference in the outcome. Conclusion: The use of vitamin C sonophoresis along with NdYAG laser may reduce the incidence of adverse effects in Asian patients. Patients experienced obvious improvement in hyperpigmentation and had lower chances of experiencing extreme or severe post-inflammatory hyperpigmentation.Introduction
In recent years, laser-based therapies have been steadily gaining in popularity as a useful intervention for skin rejuvenation due to their faster healing time, greater patient compliance and fewer potential complications.[1] Currently, the ablative class of lasers result in some degree of thermal damage in the dermis which results in dermal collagen changes and may lead to post-procedure complications like oozing, bleeding or infections. Besides, post-inflammatory pigmentation is also a potential complication, especially in Asian skin.[2] Hence, non-ablative lasers are preferred over the ablative ones for skin rejuvenation. The 532-/1064-nm Q-switched NdYAG laser has gained much attention in the treatment of hyperpigmentation. It has been also found to be effective in the treatment of rhytides, atrophic acne scars and refractory dermal melasma.[3],[4],[5],[6],[7],[8],[9] The mechanism of clinical improvement is proposed to be its ability to induce controlled dermal injury followed by a healing response and subsequent neocollagenesis.[10] It has also been postulated that the 532-/1064-nm Q-switched NdYAG laser can cause melanin granule dispersion and fragmentation without causing cellular destruction, using a sub-photothermolytic fluence.[11],[12] However, there are still reports of post-inflammatory hyperpigmentation occurring frequently following Q-switched NdYAG laser therapy and hence, further steps are required to minimize the incidence of this complication.[13],[14],[15],[16] This becomes especially important in Asian skin which is usually Fitzpatrick skin type IV and has a higher melanin content, where post-inflammatory hyperpigmentation is encountered more commonly following laser procedures.[17],[18]
Vitamin C is a popular component of many whitening and anti-ageing treatment regimens. It has the ability to inhibit melanogenesis (enzymatic conversion of tyrosine into melanin pigments) and also has an anti-oxidant effect and promotes collagen synthesis.[19],[20],[21],[22]
Sonophoresis is the method by which the energy of ultrasound waves is used to drive molecules into and across the skin. The acoustic cavitation generated by ultrasound waves and the subsequent collapse of these microbubbles on the surface of skin (stratum corneum) lead to increased skin permeability and is thought to play an essential role in ultrasound-assisted delivery.[23] Ultrasound-mediated transdermal drug delivery also has the dual advantage of being less invasive and less painful when compared to traditional drug injections.
It was postulated that vitamin C, with its inhibitory action on melanogenesis, may be a good agent to tackle post-inflammatory hyperpigmentation following laser skin rejuvenation and the delivery of vitamin C by sonophoresis may enhance treatment efficacy by increasing the permeability and absorption into the skin.[24],[25] Also, there have been reports of the effectiveness of vitamin C application immediately after NdYAG laser in preventing the side effects of the laser regimen. In this study, we have retrospectively reviewed the general outcome and incidence of post-inflammatory hyperpigmentation and other side effects in patients who received vitamin C sonophoresis immediately after five sessions of NdYAG laser treatment.
Methods
This retrospective study was approved by the Institutional Review Board Ethical Committee (Chang Gung Memorial Hospital Ethics Committee No. 101-2546B). We reviewed the clinical records of patients who underwent treatment with NdYAG laser therapy followed by transdermal delivery of vitamin C by sonophoresis in our aesthetic medicine center from October 2011 to December 2013. All patients were adults and had Fitzpatrick skin type IV. The patients who had no active skin lesions on the treatment area, no underlying skin disease and those who were not pregnant or lactating, were included in the study. Patients with a history of photosensitivity, abnormal scarring, poor wound healing, intake of oral contraceptive pills and hormone replacement therapy in the preceding one month were excluded. The underlying pigmentary disorder was classified as either dyschromia or melasma. Wood's lamp examination was used to determine the type of melasma.
The lesions were treated using sole (1064 nm) or dual wave (1064 nm and 532 nm) Q-switched NdYAG lasers (HELIOS II, Korea). The laser treatment was administered at monthly intervals, unless extreme post-inflammatory hyperpigmentation was observed. The parameters used for 1064 nm wavelength were: 7-mm spot size and energy fluence of 1.6–1.8 J/cm 2 and for 532 nm wavelength were: 3-mm spot size and energy fluence of 0.8–1.0 J/cm 2. The threshold fluence was different in each patient depending on the immediate response (the appearance of a mild erythema without petechiae) following laser irradiation. Subsequently, vitamin C (20% L-ascorbic acid gel) was delivered topically by sonophoresis with an ultrasound frequency of 1 MHz at an intensity of 1.2 W/cm 2 (Sonaderm 700, Japan). A well-trained technician conducted the sound head over the lesions and nearby areas for 12 min, in accordance with the protocol of the sonophoresis machine.
Standardized photographs (Canon EOS 550D, Canon, Tokyo, Japan) were obtained before and after the full course of the five-session treatment in a photography room with standardized fluorescent light, background and other conditions (same camera with fixed angle, flash and distance) with a fixed exposure time of 1/125 s and aperture f/8. Two independent specialists evaluated the clinical (objective) outcome and the post-laser side effects based on the photographic data. The clinical outcome of lesions were categorized as worse, bad, fair, better and excellent (score 1–5): worse (1), hyperpigmentation worse than baseline; bad (2), no change or <25% improvement; fair (3), 25–50% improvement; better (4), 50–75% improvement; excellent (5), >75% improvement. The patients were also asked to self-evaluate the outcome (subjective) with the same scoring at the end of the treatment. During the five sessions of treatment, post-inflammatory hyperpigmentation was documented according to the severity (0 = normal skin color without evidence of hyperpigmentation, 1 = slight hyperpigmentation, 2 = moderate hyperpigmentation, 3 = severe hyperpigmentation and 4 = extreme hyperpigmentation) and other post-laser minor side effects of the patients were also documented (e.g. scaling, dryness, erythema and pruritus), if noted. If severe post-inflammatory hyperpigmentation (score 3) was observed that did not resolve spontaneously in 1 month before the next session of laser treatment, it was classified as extreme post-inflammatory hyperpigmentation (score 4) and laser treatment was discontinued. Only monthly vitamin C sonophoresis and daily topical hydroquinone were prescribed in such patients until the post-inflammatory hyperpigmentation completely resolved. Patients were also asked to regularly apply broad-spectrum sunscreens with sun protection factor of 50 or above every 2 hours during any indoor or outdoor activity.
Statistical analysis
Data was analyzed using the SPSS Statistics (version 19; IBM, Armonk, NY, USA) software. The objective and subjective outcomes of the two groups (dyschromia and melasma) were compared using Mann–Whitney U-test. Chi-square test and Fisher's exact test were used to compare post-inflammatory hyperpigmentation and other side effects between the two groups, as the expected count was <5 in some cells. P < 0.05 was considered significant.
Results
A total of 23 Chinese women between the ages of 20 and 62 (mean age 38.6, standard deviation 10.4) were enrolled in the study. Eleven (47.8%) patients had dyschromia and twelve (52.2%) patients had mixed melasma [Table - 1]. Four patients had been previously treated by other lasers (ruby or erbium: yttrium aluminum garnet laser) with poor response. None of them had received any treatment in the 6 months preceding treatment with the NdYAG laser. All patients, except one who developed extreme post-inflammatory hyperpigmentation, underwent five sessions of NdYAG laser treatment and subsequent vitamin C sonophoresis.
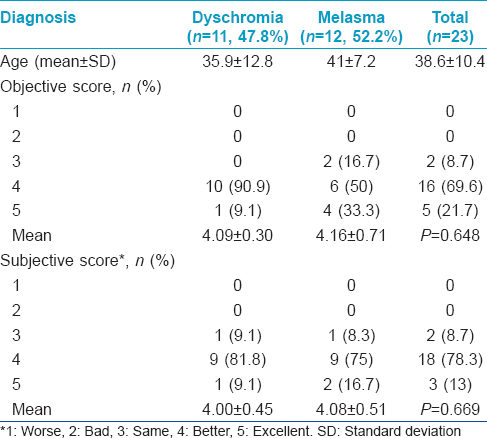
Assessment of objective clinical outcome by specialists showed that 21.7% (5/23) of the patients achieved an excellent outcome [Figure - 1]a and [Figure - 1]b, 69.6% (16/23) showed a better outcome and 8.7% (2/23) experienced no significant change. No deterioration was noted in any of the patients. Thirteen percent (3/23) of the patients self-evaluated the outcome as excellent, 78.3% (18/23) scored the outcome as better and 8.7% (2/23) scored the outcome as the same. Neither the objective scores nor the subjective scores were significantly different between the dyschromia group and the melasma group. Both groups had a mean score of over four points in objective (4.09 ± 0.30 and 4.00 ± 1.04) and subjective (3.90 ± 0.70 and 4.00 ± 0.73) outcomes [Table - 1].
 |
| Figure 1: (a) Pre-treatment photograph of a 27-year-old woman with melasma on bilateral cheeks before treatment. (b) After five sessions of treatment, excellent improvement of melasma was noted. The patient also self-evaluated the outcome as excellent. Area with significant improvement was marked with black arrowheads |
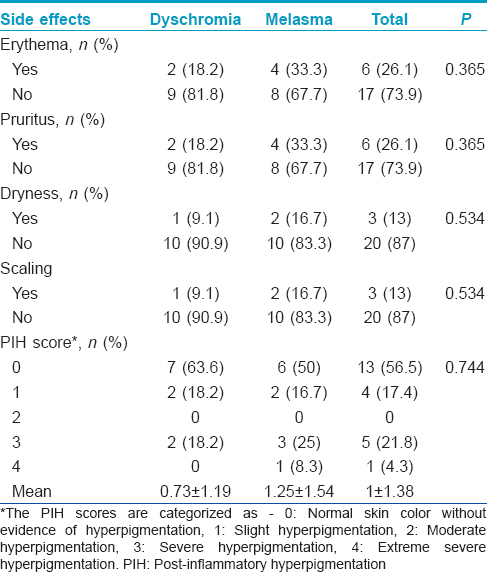
Twenty six percent (6/23) of the patients, including two patients in the dyschromia group and four patients in the melasma group developed erythema and the same percentage (6/23) also developed pruritus during the treatment sessions, whereas dryness and scaling was observed in 13% (3/23) of the patients in each group [Table - 2]. The majority (73.9%) of the patients had no evidence of post-inflammatory hyperpigmentation or had slight hyperpigmentation which quickly resolved within 1 week. Severe post-inflammatory hyperpigmentation which resolved in <4 weeks (score 3) [Figure - 2]a and [Figure - 2]b was seen in 21.8% (5/23) of the patients, including two patients in the dyschromia group and three patients in the melasma group. Only one (4.3%) patient had extreme post-inflammatory hyperpigmentation (score 4) that lasted for over 1 month, appearing 3 days after the first session of treatment. This patient discontinued the laser but continued vitamin C sonophoresis once a month and daily application of topical hydroquinone until the post-inflammatory hyperpigmentation resolved. There was also no significant difference in the incidence of post-inflammatory hyperpigmentation and other minor side effects between the two groups. All patients had a follow-up period of at least a year and recurrence of pigmentary changes in previously treated areas was noted in 21.7% (5/23) patients. The average time for the onset of recurrence after completing treatment was 4.4 months.
 |
| Figure 2: (a and b) Regular photograph of a 44-year-old woman with severe post-inflammatory hyperpigmentation. The laser course was stopped and vitamin C and hydroquinone induction was performed. The post-inflammatory hyperpigmentation resolved within 4 weeks. Area with significant improvement was marked with black arrowheads |
Discussion
The incidence of post-inflammatory hyperpigmentation following 1064-nm Q-switched NdYAG laser treatment is common in Asians ranging from 18% to 73% of the treated cases in various studies.[26],[27] The sublethal destruction or stimulation of hyperactive melanocytes during laser treatment may further increase melanin production, resulting in hyperpigmentation.[28] The 532-/1064-nm wavelength of Q-switched NdYAG laser is well-absorbed by melanosomes and pigmented cells.[29] This absorption has been shown to cause dermal and epidermal melanosome rupture, melanosome rupture in melanocytes and destruction of dermal melanophages at the appropriate threshold.[30],[31] Therefore, multiple subthreshold exposures to the 532-/1064-nm wavelength may stimulate melanogenesis in some areas and produce rebound hyperpigmentation, as was previously noted in the guinea pig model.[27],[31] Therefore, preoperative counseling, individualized treatment protocols and post-procedure care to reduce the incidence of post-laser adverse reactions are of paramount importance.
Previous studies have shown the benefits of vitamin C on wound healing, photoaging, skin discoloration and acne.[19], 20, [32],[33],[34] However, as the active form of vitamin C, L-ascorbic acid, is present as a hydrophilic, water-soluble molecule in most biological models, finding an efficient way to deliver vitamin C transdermally in high concentrations is important. Some studies demonstrated that only about 12.4% of ascorbic acid traverses the stratum corneum barrier in 72 h.[35] Taylor et al. has described a full-face iontophoresis mask of vitamin C as an effective short term treatment for melasma and post-inflammatory hyperpigmentation.[36] Other reports have mentioned the topical use of vitamin C for post-inflammatory hyperpigmentation following laser therapy, but time taken for complete resolution was 3-4 months.[37],[38] Even administration of intravenous vitamin C was proposed as a beneficial alternative for the treatment of post-inflammatory hyperpigmentation; however, a prolonged course of 18 months was needed.[39]
Stratum corneum being the outer skin layer that forms the rate-controlling diffusion barrier for most compounds, removal of this layer will increase the permeability of the skin to hydrophilic drugs. This is the reason why we chose to deliver vitamin C by sonophoresis immediately after the laser. There is increased absorption of vitamin C in high concentrations as there is a reversible destruction of the skin barrier by the laser.
Polnikorn et al. reported post-inflammatory hyperpigmentation in 39.4% (26/66) of the patients undergoing 1064-nm Q-switched-NdYAG laser treatments over 3 months.[26] In patients with melasma who were treated with 532-nm Q-switched-NdYAG laser, 28.5% (6/21) developed post-inflammatory hyperpigmentation.[40] On the contrary, in our study, with vitamin C sonophoresis immediately after laser therapy, only one person (4.3%) experienced extreme post-inflammatory hyperpigmentation (score 4) lasting for over a month. Moreover, other minor side effects such as erythema, pruritus, dryness and scaling were seen in less than one-third of the patients who underwent our protocol. This is important because, besides post-inflammatory hyperpigmentation, these minor complications may also make patients worried and influence their willingness to continue further laser therapy.
Recently, Lee et al. has also reported a marked improvement in outcome with the combination of vitamin C sonophoresis immediately after laser therapy in eight melasma patients in a split-face study and proposed the benefits of the combination in the treatment for melasma.[41] Even though the scoring scale used was different when compared to this study, a larger proportion of our patients experienced a >50% improvement. In our study, 92% (21/23) of the patients, irrespective of the groups, had felt that the lesions showed >50% improvement and only 8% (2/23) felt no difference. This may be attributed to the increased number of patients and laser sessions in our study. Furthermore, our study also showed that the outcome is long-lasting (only 21.7% of the patients had recurrence of mild pigmentation on the treated areas). This is notable in comparison to the results of the study by Wattanakrai et al., where only 1064-nm NdYAG laser was used to treat melasma in Asian patients. All the patients had recurrence at 12 weeks of follow-up, even though >50% improvement was achieved in 90.9% (20/22) patients post-treatment.[27]
Besides the good clinical outcome, this combination is also easy to administer. Administration of vitamin C by a trained therapist takes only 12 min and the need for other adjunctive topical agents is eliminated. Therefore, complications due to inadequate compliance with the post-laser care can also be reduced. The only post-laser care required as per our protocol was regular use of broad spectrum sunscreens.
The excellent clinical outcome in resolution of pigmentation when compared to other studies may be attributed to the synergic effect of vitamin C with laser treatment and also the appropriate time of administering vitamin C. Vitamin C was administered immediately after laser therapy (not before), when the pores were just opened by the thermal effect of laser and the thermal damage to the skin barrier caused increased absorption of vitamin C. Also, the increased blood circulation in the dermis due to the heating caused by the laser results in enhanced penetration of vitamin C by sonophoresis.[41] When compared to other methods, we believe that our method can provide high concentrations with a short time interval for onset of action and is a better alternative because of its safety, effectiveness and ease of administration.[36],[37],[38],[39]
There were limitations in this study. This was a retrospective cohort study without a control group, having the inherent limitations of this study design. A prospective randomized controlled study design to prove the specific effect of vitamin C sonophoresis would have provided a stronger level of evidence; however, it was difficult to recruit a control group due to the individual differences in patients' facial characteristics.[41]
In summary, the use of vitamin C sonophoresis after NdYAG laser therapy can have favorable outcomes in treating facial hyperpigmentation with less side effects in Asian patients who are at risk for post-inflammatory hyperpigmentation. Even if post-laser post-inflammatory hyperpigmentation occurred, the regression of pigmentation could be predicted within 1 month and the protocol could continue as devised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Goldberg DJ, Whitworth J. Laser skin resurfacing with the Q-switched Nd: YAG laser. Dermatol Surg 1997;23:903-6.
[Google Scholar]
|
| 2. |
Metelitsa AI, Alster TS. Fractionated laser skin resurfacing treatment complications: A review. Dermatol Surg 2010;36:299-306.
[Google Scholar]
|
| 3. |
Karabudak O, Dogan B, Baloglu H. Histologic evidence of new collagen formation using a Q-switched Nd: YAG laser in periorbital rhytids. J Dermatolog Treat 2008;19:300-4.
[Google Scholar]
|
| 4. |
Goldberg DJ, Silapunt S. Histologic evaluation of a Q-switched Nd: YAG laser in the nonablative treatment of wrinkles. Dermatol Surg 2001;27:744-6.
[Google Scholar]
|
| 5. |
Liu H, Dang Y, Wang Z, Chai X, Ren Q. Laser induced collagen remodeling: A comparative study in vivo on mouse model. Lasers Surg Med 2008;40:13-9.
[Google Scholar]
|
| 6. |
Friedman PM, Skover GR, Payonk G, Kauvar AN, Geronemus RG. 3D in-vivo optical skin imaging for topographical quantitative assessment of non-ablative laser technology. Dermatol Surg 2002;28:199-204.
[Google Scholar]
|
| 7. |
Friedman PM, Jih MH, Skover GR, Payonk GS, Kimyai-Asadi A, Geronemus RG. Treatment of atrophic facial acne scars with the 1064-nm Q-switched Nd: YAG laser: Six-month follow-up study. Arch Dermatol 2004;140:1337-41.
[Google Scholar]
|
| 8. |
Chan HH, Lam LK, Wong DS, Kono T, Trendell-Smith N. Use of 1,320 nm Nd: YAG laser for wrinkle reduction and the treatment of atrophic acne scarring in Asians. Lasers Surg Med 2004;34:98-103.
[Google Scholar]
|
| 9. |
Polnikorn N. Treatment of refractory dermal melasma with the MedLite C6 Q-switched Nd: YAG laser: Two case reports. J Cosmet Laser Ther 2008;10:167-73.
[Google Scholar]
|
| 10. |
Chan NP, Ho SG, Shek SY, Yeung CK, Chan HH. A case series of facial depigmentation associated with low fluence Q-switched 1,064nm Nd: YAG laser for skin rejuvenation and melasma. Lasers Surg Med 2010;42:712-9.
[Google Scholar]
|
| 11. |
Jeong SY, Shin JB, Yeo UC, Kim WS, Kim IH. Low-fluence Q-switched neodymium-doped yttrium aluminum garnet laser for melasma with pre-or post-treatment triple combination cream. Dermatol Surg 2010;36:909-18.
[Google Scholar]
|
| 12. |
Mun JY, Jeong SY, Kim JH, Han SS, Kim IH. A low fluence Q-switched Nd: YAG laser modifies the 3D structure of melanocyte and ultrastructure of melanosome by subcellular-selective photothermolysis. J Electron Microsc (Tokyo) 2011;60:11-8.
[Google Scholar]
|
| 13. |
Manaloto RM, Alster T. Erbium: YAG laser resurfacing for refractory melasma. Dermatol Surg 1999;25:121-3.
[Google Scholar]
|
| 14. |
Nouri K, Bowes L, Chartier T, Romagosa R, Spencer J. Combination treatment of melasma with pulsed CO2 laser followed by Q-switched alexandrite laser: A pilot study. Dermatol Surg 1999;25:494-7.
[Google Scholar]
|
| 15. |
Angsuwarangsee S, Polnikorn N. Combined ultrapulse CO2 laser and Q-switched alexandrite laser compared with Q-switched alexandrite laser alone for refractory melasma: Split-face design. Dermatol Surg 2003;29:59-64.
[Google Scholar]
|
| 16. |
Lipper GM, Anderson RR. Lasers in dermatology. In: Freedburg IM, Eisen AZ, Wolf K, Austen KF, Goldsmith LA, editors. Fitzpatrick's Dermatology in General Medicine. 6th ed. New York: McGraw Hill; 2003. p. 2493-515.
[Google Scholar]
|
| 17. |
Munnoch DA, Gorst CM, Hancock K. Post laser hyperpigmentation and occupational ultraviolet radiation exposure. Br J Plast Surg 2000;53:259-61.
[Google Scholar]
|
| 18. |
Chan HH. Effective and safe use of lasers, light sources, and radiofrequency devices in the clinical management of Asian patients with selected dermatoses. Lasers Surg Med 2005;37:179-85.
[Google Scholar]
|
| 19. |
Farris PK. Topical vitamin C: A useful agent for treating photoaging and other dermatologic conditions. Dermatol Surg 2005;31 (7 Pt 2):814-7.
[Google Scholar]
|
| 20. |
Ahn HH, Kim IH. Whitening effect of salicylic acid peels in Asian patients. Dermatol Surg 2006;32:372-5.
[Google Scholar]
|
| 21. |
Espinal-Perez LE, Moncada B, Castanedo-Cazares JP. A double-blind randomized trial of 5% ascorbic acid vs 4% hydroquinone in melasma. Int J Dermatol 2004;43:604-7.
[Google Scholar]
|
| 22. |
Humbert PG, Haftek M, Creidi P, Lapière C, Nusgens B, Richard A, et al. Topical ascorbic acid on photoaged skin. Clinical, topographical and ultrastructural evaluation: Double-blind study vs. placebo. Exp Dermatol 2003;12:237-44.
[Google Scholar]
|
| 23. |
Ueda H, Mutoh M, Seki T, Kobayashi D, Morimoto Y. Acoustic cavitation as an enhancing mechanism of low-frequency sonophoresis for transdermal drug delivery. Biol Pharm Bull 2009;32:916-20.
[Google Scholar]
|
| 24. |
Lee SH, Wang CM, Chung CJ, Hong HS. Sonophoresis with 20% L-Ascorbic acid and 2% kojic acid gel for the melasma patient. Dermatol Sin 2001;19:275-81.
[Google Scholar]
|
| 25. |
Heber G. Low frequency sonophoresis of retinol and L-ascorbic acid for photoageing: A controlled prospective pilot study. Australas J Cosmet Surg 2005;1:42-9.
[Google Scholar]
|
| 26. |
Polnikorn N, Tanrattanakorn S, Goldberg DJ. Treatment of Hori's nevus with the Q-switched Nd: YAG laser. Dermatol Surg 2000;26:477-80.
[Google Scholar]
|
| 27. |
Wattanakrai P, Mornchan R, Eimpunth S. Low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1,064 nm) laser for the treatment of facial melasma in Asians. Dermatol Surg 2010;36:76-87.
[Google Scholar]
|
| 28. |
Kang WH, Yoon KH, Lee ES, Kim J, Lee KB, Yim H, et al. Melasma: Histopathological characteristics in 56 Korean patients. Br J Dermatol 2002;146:228-37.
[Google Scholar]
|
| 29. |
Kaufmann R, Hartmann A, Hibst R. Cutting and skin-ablative properties of pulsed mid-infrared laser surgery. J Dermatol Surg Oncol 1994;20:112-8.
[Google Scholar]
|
| 30. |
Anderson RR. Laser-tissue interactions in dermatology. In: Arndt KA, Dover JS, Olbricht SM, editors. Lasers in Cutaneous and Aesthetic Surgery. Philadelphia: Lippincott-Raven; 1997. p. 25-32.
[Google Scholar]
|
| 31. |
Anderson RR, Margolis RJ, Watenabe S, Flotte T, Hruza GJ, Dover JS. Selective photothermolysis of cutaneous pigmentation by Q-switched Nd: YAG laser pulses at 1064, 532, and 355 nm. J Invest Dermatol 1989;93:28-32.
[Google Scholar]
|
| 32. |
Lee HS, Kim IH. Salicylic acid peels for the treatment of acne vulgaris in Asian patients. Dermatol Surg 2003;29:1196-9.
[Google Scholar]
|
| 33. |
Lima CC, Pereira AP, Silva JR, Oliveira LS, Resck MC, Grechi CO, et al. Ascorbic acid for the healing of skin wounds in rats. Braz J Biol 2009;69:1195-201.
[Google Scholar]
|
| 34. |
Traikovich SS. Use of topical ascorbic acid and its effects on photodamaged skin topography. Arch Otolaryngol Head Neck Surg 1999;125:1091-8.
[Google Scholar]
|
| 35. |
Kaplan DL, Moloney SJ, Troy WR, Dickens MS, Pinnell SR. A new stabilized ascorbic acid solution: Percutaneous absorption and effect on relative collagen synthesis. J Cutan Aging Cosmet Dermatol 1988;1:88-92.
[Google Scholar]
|
| 36. |
Taylor MB, Yanaki JS, Draper DO, Shurtz JC, Coglianese M. Successful short-term and long-term treatment of melasma and post-inflammatory hyperpigmentation using vitamin C with a full-face iontophoresis mask and a mandelic/malic acid skin care regimen. J Drugs Dermatol 2013;12:45-50.
[Google Scholar]
|
| 37. |
Waldorf HA, Kauvar AN, Geronemus RG. Skin resurfacing of fine to deep rhytides using a char-free carbon dioxide laser in 47 patients. Dermatol Surg 1995;21:940-6.
[Google Scholar]
|
| 38. |
Ho C, Nguyen Q, Lowe NJ, Griffin ME, Lask G. Laser resurfacing in pigmented skin. Dermatol Surg 1995;21:1035-7.
[Google Scholar]
|
| 39. |
Lee GS. Intravenous vitamin C in the treatment of post-laser hyperpigmentation for melasma: A short report. J Cosmet Laser Ther 2008;10:234-6.
[Google Scholar]
|
| 40. |
Kar HK, Gupta L, Chauhan A. A comparative study on efficacy of high and low fluence Q-switched Nd: YAG laser and glycolic acid peel in melasma. Indian J Dermatol Venereol Leprol 2012;78:165-71.
[Google Scholar]
|
| 41. |
Lee MC, Chang CS, Huang YL, Chang SL, Chang CH, Lin YF, et al. Treatment of melasma with mixed parameters of 1,064-nm Q-switched Nd: YAG laser toning and an enhanced effect of ultrasonic application of vitamin C: A split-face study. Lasers Med Sci 2015;30:159-63.
[Google Scholar]
|
Fulltext Views
5,064
PDF downloads
2,268





