Translate this page into:
Linear basal cell carcinoma: Report of three cases with dermoscopic findings
2 Department of Pathology, Hospital Universitario Reina Sofía, Córdoba, Spain
Correspondence Address:
Carmen Mar�a Alc�ntara-Reifs
Avenida Menéndez Pidal s/n, 14004 Córdoba
Spain
| How to cite this article: Alc�ntara-Reifs CM, Salido-Vallejo R, Gonz�lez-Menchen A, Garc�a-Nieto AV. Linear basal cell carcinoma: Report of three cases with dermoscopic findings. Indian J Dermatol Venereol Leprol 2016;82:708-711 |
Sir,
Linear basal cell carcinoma was first described as a new clinical subtype in 1985 by Lewis. We were able to find published reports of only 43 other cases since then. Certain unique clinical and histological characteristics differentiate it from other basal cell carcinomas hence, some authors consider it as a different clinical entity.[1],[2] Herein, we report three cases of linear basal cell carcinoma.
Patient 1 was an 86-year-old woman referred for the evaluation of a linear pigmented lesion on the right side of the neck. The lesion was first noticed 10 months previously; there was no evidence of trauma or any other trigger at that site. On physical examination, we observed a linear pigmented macule aligned along the relaxed skin tension lines, measuring 10 mm × 1 mm [Figure - 1]a. Dermoscopy highlighted the absence of a pigmented network pattern and the presence of three of the six criteria for pigmented basal cell carcinoma according to Menzies: maple leaf-like areas, spoke-wheel areas and large blue-gray ovoid nests [Figure - 1]b.[3] Patient 2 was an 84-year-old man who consulted us for an asymptomatic, 16 mm × 4 mm lesion on his upper chest which had slowly enlarged in a linear fashion in the last 2 years [Figure - 2]a. Dermoscopy showed maple leaf-like areas, spoke-wheel areas, large blue-gray ovoid nests, ulceration and arborizing telangiectasias [Figure - 2]b. Patient 3 was a 77-year-old woman who presented with a 13-month history of an asymptomatic lesion on her face. We observed a non-palpable, linear pigmented lesion measuring 14 mm × 2 mm [Figure - 3]a. Dermoscopic findings included maple leaf-like areas, spoke-wheel areas, large blue-gray ovoid nests and slight ulceration [Figure - 3]b. In our three patients, the tumor region was completely excised with a 3-mm safety margin with primary closure of the wound. The histological findings confirmed the diagnosis of basal cell carcinoma; the surgical margins were free of tumor cells in all cases. Histologically, in patient 1 and 2, the tumour nests mainly appeared in a nodular arrangement [Figure - 1]c and [Figure - 2]c, so nodular subtype of basal cell carcinoma was diagnosed. In patient 3, the histological analysis of the lesion was diagnostic of the superficial variant of basal cell carcinoma [Figure - 3]c.
 |
| Figure 1a: Linear pigmented macule aligned along the relaxed skin tension lines |
 |
| Figure 1b: Dermoscopic appearance: absence of a pigmented network pattern, maple leafl ike areas, spoke wheels areas and large blue-gray ovoid nests |
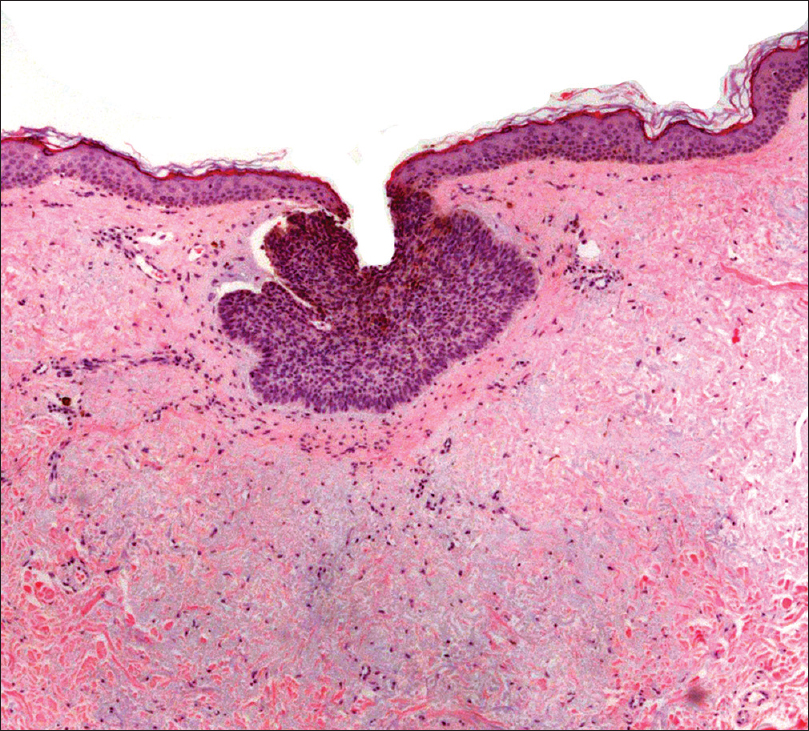 |
| FIgure 1c: Nodular and pigmented basal cell carcinoma (H and E, ×200) |
 |
| Figure 2a: Linear pigmented lesion with eroded surface |
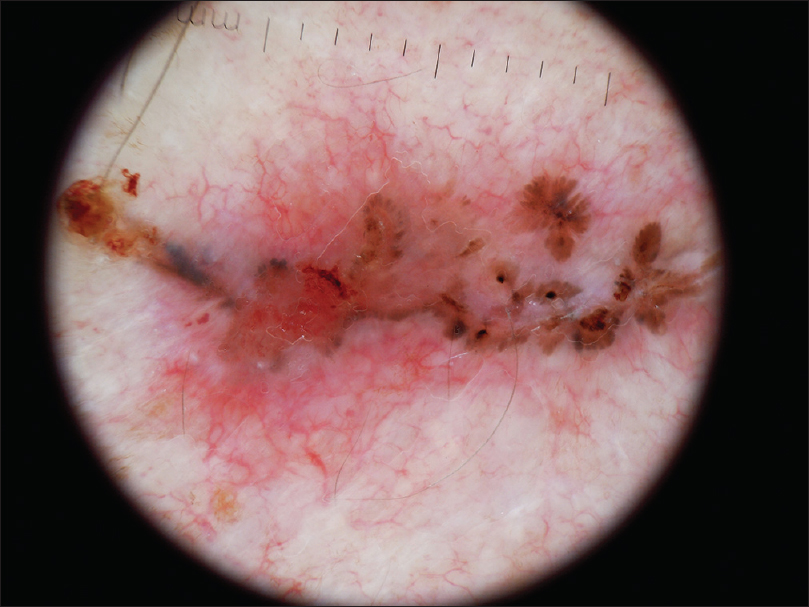 |
| Figure 2b: Dermoscopic appearance: maple leaflike areas, spoke wheels areas, large blue-gray ovoid nests, ulceration and telangiectasias |
 |
| Figure 2c: Nodular and pigmented basal cell carcinoma (H and E, ×200) |
 |
| Figure 3a: Linear pigmented tumor with erythema and slight ulceration |
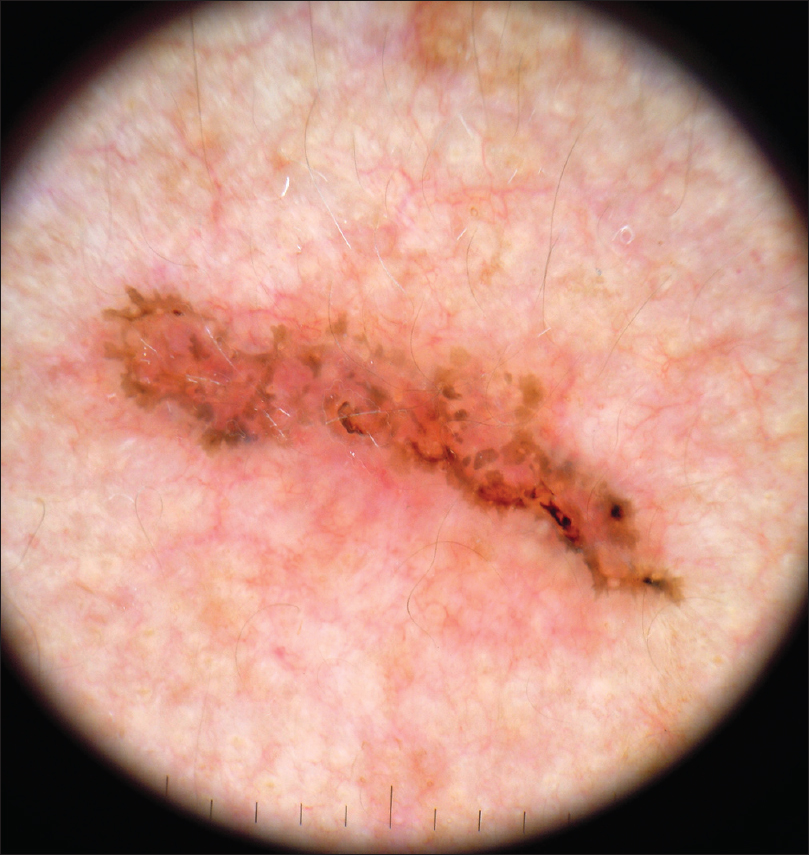 |
| Figure 3b: Dermoscopic appearance: maple leafl ike areas, spoke wheels areas, large blue-gray ovoid nests and slight ulcerations |
 |
| Figure 3c: Superficial and pigmented basal cell carcinoma (H and E, ×200) |
Linear basal cell carcinoma extends preferentially in one direction resulting in the characteristic morphology of a linear lesion with straight edges and a length-to-width ratio of at least 3:1.[4] Some of the mechanisms that have been suggested to explain this mode of growth include limitation of lateral spread of the lesion by dermal fibrosis or interaction of the stroma with Langer's lines since basal cell carcinomas depend on stromal interactions for progression and growth. Focal trauma is an established risk factor in the development of basal cell carcinoma so the possibility of Koebnerisation has also been proposed to explain the linear pattern and its orientation along the tension lines of the skin.[1],[2] In the largest histological series, the proportion of basal cell carcinoma containing pigment ranges from 6.7% to 8.5%.[5] In our cases, 100% of the tumors were pigmented and showed maple leaf-like areas and spoke wheel areas on dermoscopy, two uncommon but highly specific diagnostic criteria. Among the reported cases, the most common histological subtype was nodular.[2] However, Al-Niaimi and Lyonfound that 32% of linear basal cell carcinoma had an aggressive histological subtype such as micronodular, infiltrative or morpheaform; a percentage much greater than expected in the general population.[1] In addition, some authors have described the potential for wider subclinical extension in this variant of basal cell carcinoma. Therefore, Mohs micrographic surgery is preferred as the treatment of choice.[2] In our three patients, the histological findings did correlate with the clinical appearance of the lesions and conventional surgery was curative. We think this clinical subtype of basal cell carcinoma should not determine the surgical approach. Conventional surgery can be a suitable first-line treatment and Mohs micrographic surgery should be reserved as an alternative in the following scenarios: anatomical regions where large resection margins are not practicable, recurrent forms of basal cell carcinoma, when unexpected positive margins occur after recent excision, primary aggressive histological forms of the tumor: morpheaform, infiltrating, perineural, metatypical or micronodular, or high-risk areas of body: area H and area M. We believe this entity is under-reported due to its under-recognition. Further investigation of linear basal cell carcinoma in a larger series of patients is needed to elucidate the histological aggressiveness of this clinical subtype, the proportion of linear basal cell carcinomas containing pigment and the best surgical approach for these patients. Undoubtedly, dermoscopy is an essential tool in the diagnosis of this entity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Al-Niaimi F, Lyon CC. Linear basal cell carcinoma: A distinct condition? Clin Exp Dermatol 2011;36:231-4.
[Google Scholar]
|
| 2. |
Mavrikakis I, Malhotra R, Selva D, Huilgol SC, Barlow R. Linear basal cell carcinoma: A distinct clinical entity. J Plast Reconstr Aesthet Surg 2006;59:419-23.
[Google Scholar]
|
| 3. |
Menzies SW. Dermoscopy of pigmented basal cell carcinoma. Clin Dermatol 2002;20:268-9.
[Google Scholar]
|
| 4. |
Ichinokawa Y, Ohtuki A, Hattori M, Sadamasa H, Hiruma M, Matumoto T. Linear basal cell carcinoma: A case report. Case Rep Dermatol 2011;3:142-6.
[Google Scholar]
|
| 5. |
Maloney ME, Jones DB, Sexton FM. Pigmented basal cell carcinoma: Investigation of 70 cases. J Am Acad Dermatol 1992;27:74-8.
[Google Scholar]
|
Fulltext Views
3,430
PDF downloads
2,163





