Translate this page into:
Nonhealing ulcer on the fingertip
Corresponding author: Dr. Vishal Gupta, Department of Dermatology and Venereology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029, India. doctor. vishalgupta@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta V, Sharma A, Khanna N, Mahajan S, Mridha AR. Nonhealing ulcer on the fingertip. Indian J Dermatol Venereol Leprol 2022;88:207-9.
A 59-year-old farmer from north-east India presented to us with a painless gradually enlarging ulcer at the tip of his left little finger for the last 4 years. He recalled a history of penetrating trauma 3 months prior to the onset of ulcer. There was intermittent pus discharge which improved partially with repeated courses of antibiotics. His past medical history was noncontributory. Cutaneous examination revealed a round-to-oval, non-tender ulcer measuring around 1.5 × 1 cm on the left fifth finger hyponychium extending to the fingertip. The nail plate was elevated by erythematous fleshy eroded granulation tissue on the ulcer floor covered with slough, but there was no nail plate dystrophy [Figure 1]. The finger pulp was edematous and had dusky discoloration. There was no locoregional lymphadenopathy. A punch biopsy from the edge of the ulcer was performed [Figure 2].

- Round-to-oval ulcer with erythematous fleshy eroded granulation tissue present on the hyponychium extending to the fingertip (dorsal view)

- Round-to-oval ulcer with erythematous fleshy eroded granulation tissue present on the hyponychium extending to the fingertip (ventral view)

- Skin biopsy from the edge of the ulcer showing cohesive groups of keratinocytes infiltrating into the underlying dermis (H and E, ×100)
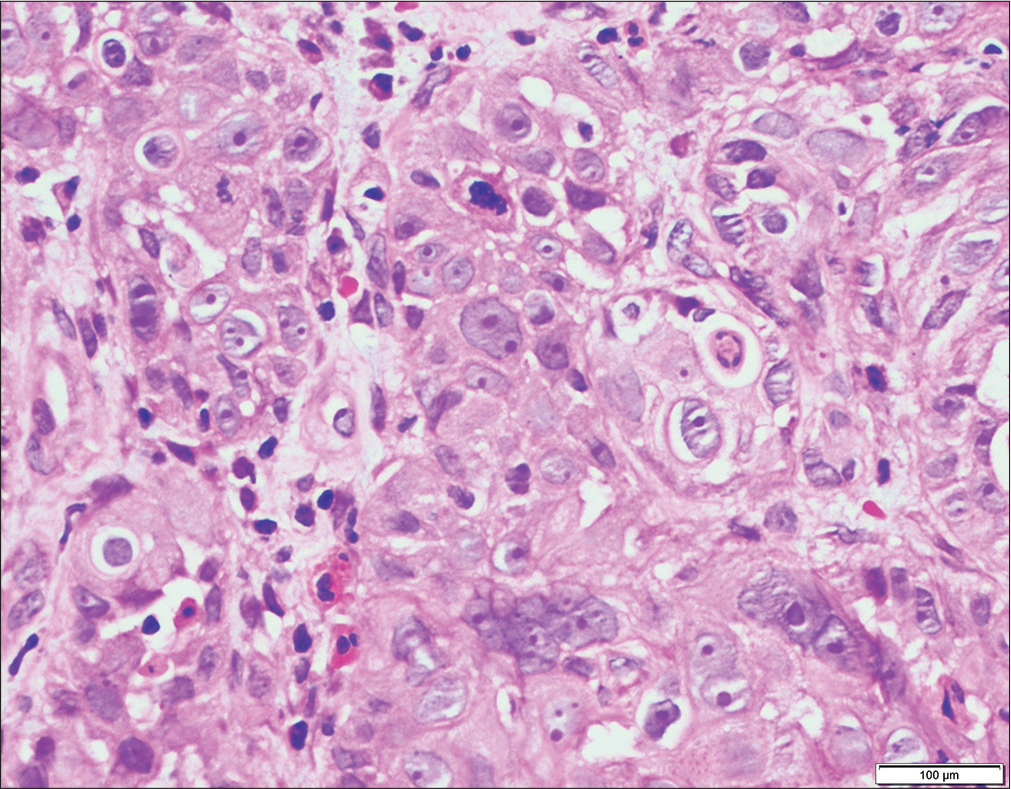
- Higher magnification shows that the cells are polygonal with pleomorphic vesicular nuclei, prominent eosinophilic nucleoli and a moderate amount of eosinophilic cytoplasm. Dyskeratotic keratinocytes and mitotic figures are also seen (H and E, ×400).
What is Your Diagnosis?
Diagnosis
Subungual squamous cell carcinoma.
Discussion
Stain for acid-fast bacilli and culture for mycobacteria and fungus from the pus were negative. Histopathology showed cohesive groups of keratinocytes having pleomorphic large vesicular nuclei with prominent nucleoli, and loss of polarity infiltrating into the underlying dermis. A few dyskeratotic keratinocytes and mitotic figures were also seen [Figure 2a and b]. Polymerase chain reaction was positive for human papillomavirus-16, 18 and 33 in the skin biopsy specimen. Radiograph showed erosion at the tip of the distal phalanx of the fifth digit [Figure 3]. The left fifth finger was disarticulated at the distal interphalangeal joint under ring block by the surgical oncology team, and adequate margins were confirmed on histopathology. The patient had no recurrence during the 1-year follow up period.

- X-ray of the left hand showing mild erosion of left 5th distal phalanx
Subungual squamous cell carcinoma is a rare entity. Typically, it presents as a warty growth affecting the nail bed and periungual areas with associated nail dystrophy. However, clinical presentations are varied and it often gets mistaken for benign entities such as verruca vulgaris, onychomycoses, chronic paronychia, cellulitis or other chronic infections.1 Because of protean manifestations, secondary infections, lack of visibility of the tumor beneath the nail plate coupled with a lack of awareness among clinicians, correct diagnosis of this entity is often delayed, by an average of 4–40 years.2-4 In our case also, the diagnosis of squamous cell carcinoma was not suspected clinically because of the non-characteristic morphology of the ulcer and its atypical location. Further, the history of trauma during farming work and partial improvement with antibiotics proved to be a red herring leading us to suspect an infectious etiology for the fingertip ulcer. Farmers are at risk of acquiring deep fungal or non-tubercular mycobacterial infections through a wood splinter injury or soil contamination of the wound. Sporotrichosis and atypical mycobacterial infections can present as non-healing ulcers on fingertips.5
Despite the initial delay in diagnosis, the prognosis for subungual squamous cell carcinoma is largely favorable. It is considered a low-grade malignancy and is less aggressive than squamous cell carcinoma at other anatomical locations. Underlying bone involvement has been reported in 16–66% of patients, and nodal involvement in about 2% of patients. Tumor resection is usually curative with a low risk of recurrence or metastases.1,2,6 Though the risk factors are poorly understood, exposure to known carcinogens such as arsenic, grease oil, radiation, repetitive trauma and friction, immunosuppressive states such as in a transplant recipient and human papillomavirus infection have been implicated. 1 Human papillomavirus-16 has been identified most commonly among the human papillomavirus-associated ungual and periungual squamous cell carcinomas.7 Infection with this and other high-risk types seems to have predisposed our patient to the development of squamous cell carcinoma. However, he did not have a history or presence of anogenital warts, suggesting that he may have been infected through a nongenital contact with someone having high-risk papillomavirus infection. The role of repetitive trauma as a contributing factor cannot be ruled out, given our patient’s occupation. To conclude, the diagnosis of subungual squamous cell carcinoma can be challenging. Dermatologists should be aware of this atypical location and should keep a high index of suspicion for squamous cell carcinoma for chronic recurrent or persistent nail unit lesions not responding to conventional treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal the identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Subungual squamous cell carcinoma: A case series. Indian J Dermatol. 2014;59:352-4.
- [CrossRef] [PubMed] [Google Scholar]
- Subungual squamous cell carcinoma masquerading as chronic common infection. J Med Assoc Thai. 2010;93:248-51.
- [Google Scholar]
- A diabetic elderly man with finger ulcer. Korean J Fam Med. 2018;39:126-9.
- [CrossRef] [PubMed] [Google Scholar]
- Mohs micrographic surgery of the nail unit and squamous cell carcinoma. Dermatol Surg. 2001;27:246-51.
- [CrossRef] [PubMed] [Google Scholar]
- Ungual and periungual human papillomavirus-associated squamous cell carcinoma: A review. J Am Acad Dermatol. 2011;64:1147-53.
- [CrossRef] [PubMed] [Google Scholar]





