Translate this page into:
Onychomycosis: A study of self-recognition by patients and quality of life
Correspondence Address:
Charussri Leeyaphan
Department of Dermatology, Faculty of Medicine, Siriraj Hospital, Mahidol University, 2 Prannok Road, Bangkoknoi, Bangkok 10700
Thailand
| How to cite this article: Bunyaratavej S, Pattanaprichakul P, Leeyaphan C, Chayangsu O, Bunyaratavej S, Kulthanan K. Onychomycosis: A study of self-recognition by patients and quality of life. Indian J Dermatol Venereol Leprol 2015;81:270-274 |
Abstract
Background: Onychomycosis accounts for approximately half of all nail disorders and is usually asymptomatic. Objectives: To evaluate patients' recognition of fungal nail disease, concomitant fungal skin diseases, complications, and quality of life. Methods: Patients from the fungal nail clinic were enrolled between May 2011 and April 2012. Patients' awareness of diseased nails was evaluated and the Dermatology Life Quality Index (DLQI) questionnaire was used to evaluate the impact of dermatologic disease on quality of life. Results: A total of 110 patients with onychomycosis were enrolled in the study, of which 64 (58.2%) were female and the mean age was 60.8 years. The number of patients who were able to recognize the presence of onychomycosis was 71 (64.5%), while 32 (29.1%) and 7 (6.4%) were diagnosed by a dermatologist and other physicians, respectively. Multivariate analysis showed that patient recognition of the disease was significantly associated with female sex and young age. The mean DLQI score was 3.6. Limitation: Patient recall bias including the duration of fungal nail infection, long-term past history and previous treatment was a limitation of this study that affected DLQI scores. Conclusion: About half of onychomycosis patients, especially elderly males, could not recognize the disease by themselves. It is important for physicians to educate patients with risk factors for onychomycosis to recognize this condition early to prevent concomitant infection and complications, and to improve patients' well-being.INTRODUCTION
Onychomycosis is responsible for about 50% of all nail diseases and 30% of all cutaneous fungal infections. [1] The prevalence of onychomycosis in various populations has ranged from 2-14%. [2],[3],[4],[5],[6],[7]
Predisposing factors for onychomycosis have been reported in many previous studies and may be classified into host features and environmental factors. [2],[5],[6],[8],[9],[10],[11] Because of the slowly progressive and asymptomatic nature of disease, most patients do not visit the hospital early for investigation and treatment. Delayed treatment may contribute to concomitant fungal skin infections such as tinea pedis [12],[13] and can lead to serious complications such as acute bacterial cellulitis. The association between fungal foot infection and cellulitis has been reported and the incidence of cellulitis was found to be increased in patients with fungal infection of feet. There were about 82% of patients who had fungal infection at several sites coincident with cellulitis. This report also found that patients with multiple sites of fungal infection were at high risk for development of concurrent cellulitis (odds ratio [OR]: 2.4; P < 0.001). [13],[14],[15]
Fungal nail infection can significantly affect the physical, psychological, and social aspects of life of a patient. [1],[16],[17],[18],[19],[20] The Dermatology Life Quality Index (DLQI) questionnaire was used to evaluate the impact of dermatologic disease on quality of life (QoL). [21],[22]
We found a single previous study reporting on patients′ self-recognition of onychomycosis. [9] The aims of this study were to evaluate patients′ awareness of onychomycosis, concomitant fungal skin infection, complications, and predisposing factors of fungal nail infection, as well as determine the quality of life in this group of patients during their follow-up visits.
METHODS
Population and study design
This was a cross-sectional descriptive study approved by Siriraj Hospital Institutional Review Board (SIRB). Patients of the fungal nail outpatient clinic of department of dermatology, Siriraj Hospital, Bangkok, Thailand who satisfied the following criteria were enrolled between May 2011 and April 2012: age above 18 years, literate, with a diagnosis of onychomycosis on both clinical and mycological examination including direct microscopic examination and fungal culture. Patients with other nail abnormalities such as psoriatic nails were excluded.
Patients′ demographic data, duration and symptoms of onychomycosis such as pain and pruritus, the presence of concomitant fungal skin diseases, other underlying diseases, predisposing factors, onychomycosis-related complications and the disease recognition process (self-diagnosis and diagnosis by a doctor) were documented in an interview conducted by physicians and were recorded in the case record form. All patients were asked to complete the validated DLQI questionnaire in Thai without receiving aid from others. [21],[22]
Statistical analysis
Descriptive statistics were used to describe the demographic and clinical data of the patients in this study. The patients were categorized into two groups: self-diagnosed and diagnosed by a physician. Pearson′s Chi-square test was used to test the association between two categorical variables. Independent sample t-test was applied to compare the mean DLQI scores of the two groups, and multiple logistic regression was performed to test the association between recognition of onychomycosis and multiple patient factors simultaneously. All statistical analyses were performed using PASW statistics 18.0 (IBM Corporation, New York, USA). A P value < 0.05 was considered to be statistically significant.
RESULTS
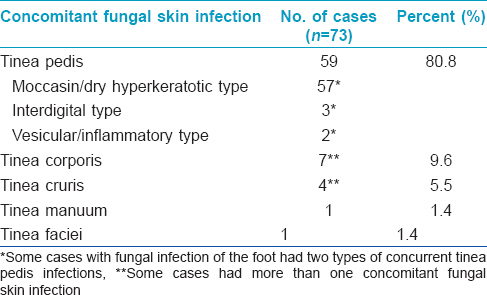
Out of 110 patients, 64 (58.2%) were female and the mean age was 60.8 ± 13.6 years. The mean duration of onychomycosis was 4.6 ± 5.2 years. The most common site was the great toenail. Demographic data, predisposing factors, duration and sites of onychomycosis are shown in [Table - 1]. Concomitant fungal skin infection was observed in 48 (56.4%) patients; the most common co-infection was moccasin-type tinea pedis [Table - 2].

Eleven (10%) patients had complications from onychomycosis during the study period. The most common complication was paronychia in 10 (9.1%) cases. Only one patient developed acute bacterial cellulitis.
The proportions of cases with self-recognition of onychomycosis, diagnosis by a dermatologist, and diagnosed by other physicians were 71 (64.5%), 32 (29.1%) and 7 (6.4%) respectively. In the group of patients who were diagnosed by a dermatologist, 17 (53.1%) cases presented with fungal skin infection and 10 (31.2%) cases presented with eczema. Among the patients who were diagnosed by other physicians, two (28.6%) cases each sought medical attention for diabetes mellitus and coronary heart disease, respectively. Multivariate analysis demonstrated that female and young patients were more likely to self-diagnose [Table - 3].
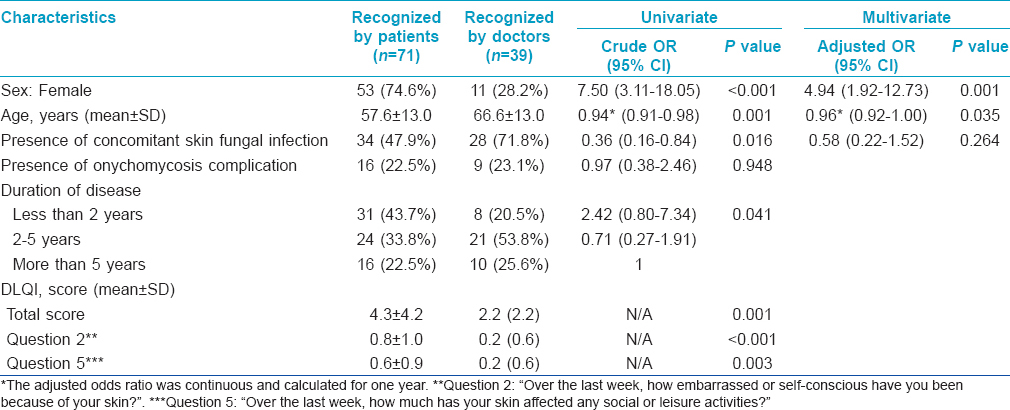
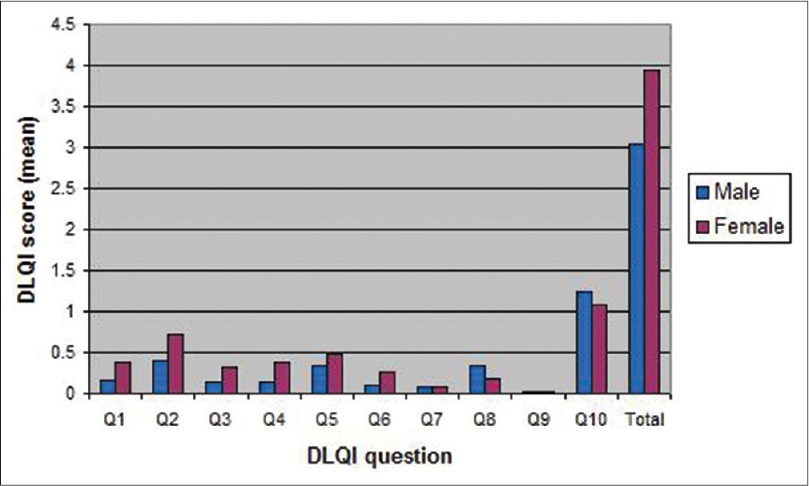
The mean of the total DLQI score in this study was 3.6 ± 3.75 (range 0-20). The mean score for each question is shown in [Figure - 1]. Question 10 on treatment difficulties had the highest mean DLQI score in this cohort and question 9 on sexual activities had the lowest score. The score on questions on symptoms and daily activities was significantly associated with female sex [Figure - 2]. A more significant impact on symptoms, feeling and daily activity was noted in patients aged less than 60 years [Figure - 3].
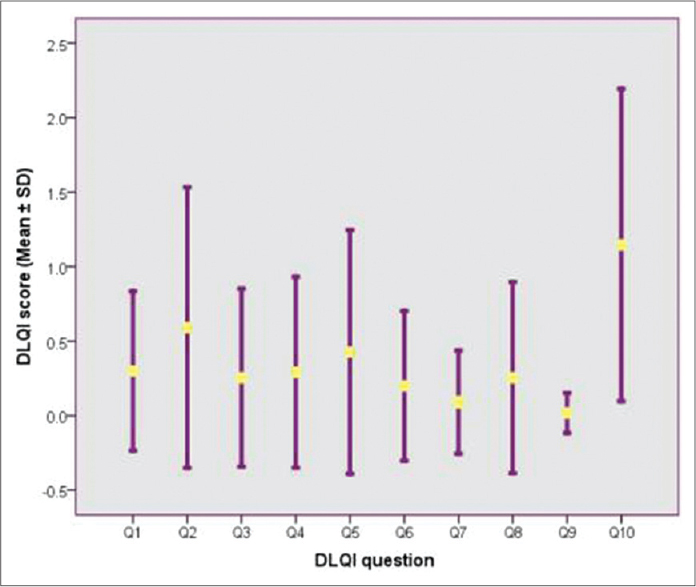 |
| Figure 1: Mean ± SD of DLQI score for each question (n=110) |
 |
| Figure 2: Mean DLQI score and associated P-value (shown on the top of the bar) for each question categorized by sex (n=110) |
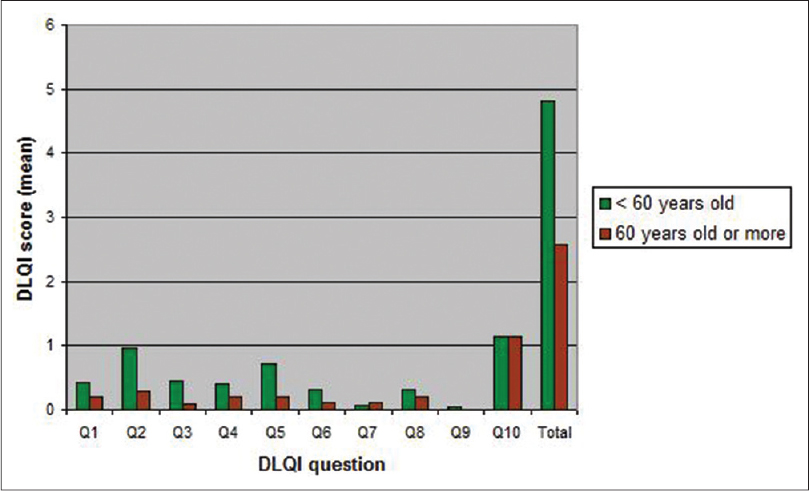 |
| Figure 3: Mean DLQI score and associated P-value (shown on the top of the bar) for each question categorized by age group (n=110) |
Moreover, we observed that the mean DLQI scores for questions 2 and 5 of patients who recognized the disease by themselves were statistically higher than those who were diagnosed by physicians. The detailed DLQI questionnaire is shown in [Figure - 4].
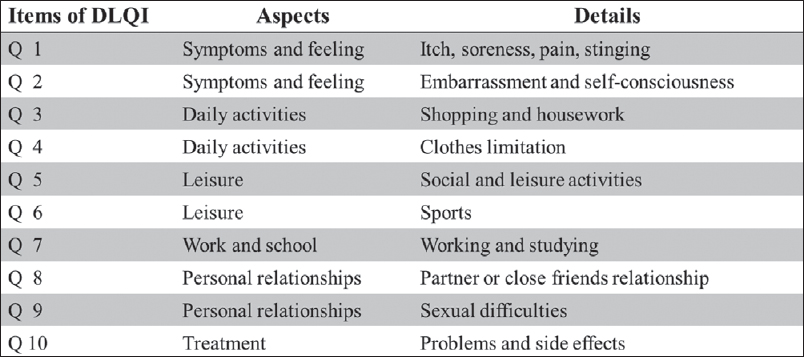 |
| Figure 4: Different aspects associated with quality of life impairment in the Dermatology Life Quality Index (DLQI): Q1-Q10 |
DISCUSSION
Most patients were female and the mean age was around 60 years, which was concordant with previous studies showing that onychomycosis was common in the elderly. [3],[23] This is attributed to nail trauma and slow nail growth. More than half the patients were obese, which is also a documented risk factor for fungal nail infection. [1],[11],[24],[25] Obesity possibly contributes to increased risk of onychomycosis due to suboptimal health, physical inactivity, and inability to maintain good hygiene.
The mean duration of onychomycosis in our cohort was 4.6 years, which was less compared to a previous study which had a mean duration of 9.5 years. [19]
Most patients were able to recognize the fungal nail disease from changes in nail color and thickness. Most of the physicians in this study diagnosed onychomycosis based on nail thickening or hyperkeratosis, which is consistent with the finding of a previous study from Mexico. [9]
This study demonstrated that most cases were asymptomatic. Patients were more likely to self-diagnose as a result of itching or pain due to complications like paronychia. This may imply that recognition by some patients was delayed until complications arose. Patients should be educated about onychomycosis to enhance recognition of the disease and prevent complications.
According to the results of multiple logistic regression, young patients and women were most likely to be aware of their onychomycosis . This implies that physicians should pay more attention to men and the elderly, especially the neglected or physically impaired. This study revealed that the cases recognized by doctors were significantly associated with concomitant cutaneous fungal infection. It is important to identify onychomycosis in patients with fungal skin infections as if untreated, onychomycosis may be responsible for recurrent skin infections.
In the present study, the most common concomitant fungal skin infection was tinea pedis with a prevalence of 89 (81%) cases, which is much higher than the 33.8% in a previous report from Poland. [12] The most common type of tinea pedis found in onychomycosis in the present study was moccasin or hyperkeratotic type (101 cases, 92%), which is similar to the findings of a previous report from Japan. [10] Fungal infection of the foot was more common than other fungal skin infections in our patients. This may be due to the close proximity of the foot skin to the toenail.
A previous case-control study showed that strong risk factors for cellulitis of the leg were interdigital and plantar type of tinea pedis, onychomycosis, disruption of skin barrier, previous history of cellulitis, and chronic venous insufficiency and leg edema. [13] In our study, the only patient who developed acute bacterial cellulitis of the leg had concomitant interdigital and plantar tinea pedis.
The validated Thai version DLQI questionnaire was used to measure quality of life in our study. [22] Though nail QoL may be a better tool to assess quality of life in patients with nail diseases, there is no validated Thai-version of nail QoL at this moment.
A previous study assessing quality of life in patients with nail disorders found that quality of life was significantly more affected in patients with onychomycosis than in other nail disorders, especially those having multiple nails involved, women, and in people aged 60-79 years. [16] Another study revealed that patients with toenail onychomycosis had low self-esteem and were less pleased to participate in social activities. [26] In this study, higher DLQI score on symptoms and daily activities was significantly associated with the female sex. DLQI score of nail diseases was less compared to other skin disorders such as acne, pigmentary disorders, or psoriasis. [26] This could either reflect the asymptomatic nature of onychomycosis or patients′ ignorance of disease. The results of our study may not be representative of disease at initial presentation as the DLQI questionnaire was completed at follow up visits by which time patients had had partial improvement of the disease with treatment. Another limitation of this study is potential patient recall bias. It is also important to keep in mind that the cohort in this study was patients from the fungal nail clinic; hence, they might be more concerned about the disease than general patients, and this may influence the DLQI score.
CONCLUSION
Despite the fact that onychomycosis has a small impact on QoL, all physicians should recognize its importance, and educate their patients, especially male and elderly, to notice this condition early. This will prevent concomitant infections and further complications as well as improve patients′ well-being.
ACKNOWLEDGMENT
In other respects, the authors would like to thank Assistant Professor Dr. Chulaluk Komoltri for her advice about statistical analysis. All authors have neither conflicts of interest nor financial support from the pharmaceutical companies. This study is supported by Routine to Research Management Fund, Faculty of Medicine, Siriraj Hospital, Mahidol University.
| 1. |
Elewski BE. Onychomycosis. Treatment, quality of life, and economic issues. Am J Clin Dermatol 2000;1:19-26.
[Google Scholar]
|
| 2. |
Perea S, Ramos MJ, Garau M, Gonzalez A, Noriega AR, del Palacio A. Prevalence and risk factors of tineaunguium and tineapedis in the general population in Spain. J Clin Microbiol 2000;38:3226-30.
[Google Scholar]
|
| 3. |
Ghannoum MA, Hajjeh RA, Scher R, Konnikov N, Gupta AK, Summerbell R, et al. A large-scale North American study of fungal isolates from nails: The frequency of onychomycosis, fungal distribution, and antifungal susceptibility patterns. J Am Acad Dermatol 2000;43:641-8.
[Google Scholar]
|
| 4. |
Elewski BE, Charif MA. Prevalence of onychomycosis in patients attending a dermatology clinic in northeastern Ohio for other conditions. Arch Dermatol 1997;133:1172-3.
[Google Scholar]
|
| 5. |
deBerker D. Clinical practice. Fungal nail disease. N Engl J Med 2009;360:2108-16.
[Google Scholar]
|
| 6. |
Cheng S, Chong L. A prospective epidemiological study on tineapedis and onychomycosis in Hong Kong. Chin Med J (Engl) 2002;115:860-5.
[Google Scholar]
|
| 7. |
Ungpakorn R, Lohaprathan S, Reangchainam S. Prevalence of foot diseases in outpatients attending the Institute of Dermatology, Bangkok, Thailand. Clin Exp Dermatol 2004;29:87-90.
[Google Scholar]
|
| 8. |
Elewski BE. Onychomycosis: Pathogenesis, diagnosis, and management. Clin Microbiol Rev 1998;11:415-29.
[Google Scholar]
|
| 9. |
Arenas R, Bonifaz A, Padilla MC, Arce M, Atoche C, Barba J, et al. Onychomycosis. A Mexican survey. Eur J Dermatol 2010;20:611-4.
[Google Scholar]
|
| 10. |
Ogasawara Y, Hiruma M, Muto M, Ogawa H. Clinical and mycological study of occult tineapedis and tineaunguium in dermatological patients from Tokyo. Mycoses 2003;46:114-9.
[Google Scholar]
|
| 11. |
Tosti A, Hay R, Arenas-Guzman R. Patients at risk of onychomycosis - risk factor identification and active prevention. J Eur Acad Dermatol Venereol 2005;19:13-6.
[Google Scholar]
|
| 12. |
Szepietowski JC, Reich A, Garlowska E, Kulig M, Baran E. Factors influencing coexistence of toenail onychomycosis with tineapedis and other dermatomycoses: A survey of 2761 patients. Arch Dermatol 2006;142:1279-84.
[Google Scholar]
|
| 13. |
Roujeau JC, Sigurgeirsson B, Korting HC, Kerl H, Paul C. Chronic dermatomycoses of the foot as risk factors for acute bacterial cellulitis of the leg: A case-control study. Dermatology 2004;209:301-7.
[Google Scholar]
|
| 14. |
Bristow IR, Spruce MC. Fungal foot infection, cellulitis and diabetes: A review. Diabet Med 2009;26:548-51.
[Google Scholar]
|
| 15. |
Vanhooteghem O, Szepetiuk G, Paurobally D, Heureux F. Chronic interdigital dermatophytic infection: A common lesion associated with potentially severe consequences. Diabetes Res Clin Pract 2011;91:23-5.
[Google Scholar]
|
| 16. |
Belyayeva E, Gregoriou S, Chalikias J, Kontochristopoulos G, Koumantaki E, Makris M, et al. The impact of nail disorders on quality of life. Eur J Dermatol 2013;23:366-71.
[Google Scholar]
|
| 17. |
Milobratović D, Janković S, Vukičević J, Marinković J, Janković J, Railić Z. Quality of life in patients with toenail onychomycosis. Mycoses 2013;56:543-51.
[Google Scholar]
|
| 18. |
18. Tejada CS, Mendoza-Sassi RA, Almeida HL, Figueiredo PN, Tejada VF. Impact on the quality of life of dermatological patients in southern Brazil. An Bras Dermatol 2011;86:1113-21.
[Google Scholar]
|
| 19. |
Drake LA, Scher RK, Smith EB, Faich GA, Smith SL, Hong JJ, et al. Effect of onychomycosis on quality of life. J Am Acad Dermatol 1998;38:702-4.
[Google Scholar]
|
| 20. |
20. Szepietowski JC, Reich A, Pacan P, Garlowska E, Baran E. Evaluation of quality of life in patients with toenail onychomycosis by Polish version of an international onychomycosis-specific questionnaire. J Eur Acad Dermatol Venereol 2007;21:491-6.
[Google Scholar]
|
| 21. |
21. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)-a simple practical measure for routine clinical use. Clin Exp Dermatol 1994;19:210-6.
[Google Scholar]
|
| 22. |
22. Kulthanan K, Jiamton S, Wanitphakdeedecha R, Chantharujikaphong S The validity and reliability of Dermatology Life Quality Index (DLQI) in Thais. Thai J Dermatol 2004;20:113-23.
[Google Scholar]
|
| 23. |
23. Thomas J, Jacobson GA, Narkowicz CK, Peterson GM, Burnet H, Sharpe C. Toenail onychomycosis: An important global disease burden. J Clin Pharm Ther 2010;35:497-519.
[Google Scholar]
|
| 24. |
24. Campbell AW, Anyanwu EC, Morad M. Evaluation of the drug treatment and persistence of onychomycosis. ScientificWorldJournal 2004;4:760-77.
[Google Scholar]
|
| 25. |
25. Sigurgeirsson B, Steingrimsson O. Risk factors associated with onychomycosis. J Eur Acad Dermatol Venereol 2004;18:48-51.
[Google Scholar]
|
| 26. |
26. Reich A, Szepietowski JC. Quality of Life in Toenail Onychomycosis. Handbook of Disease Burdens and Quality of Life Measures. New York: Springer; 2010. p. 3837-50.
[Google Scholar]
|
Fulltext Views
5,012
PDF downloads
3,367





