Translate this page into:
Linear arrangement of neutrophils along the basal layer in a case of bullous pemphigoid
Correspondence Address:
Chang Jian-Min
Department of Dermatology, Beijing Hospital, No. 1 Dahua Road, Dongdan, Beijing 100730
China
| How to cite this article: Min Y, Xiao-Man G, Jian-Min C. Linear arrangement of neutrophils along the basal layer in a case of bullous pemphigoid. Indian J Dermatol Venereol Leprol 2015;81:416-418 |
Sir,
Bullous pemphigoid is the most common autoimmune subepidermal bullous disease and often presents as generalized bullae accompanied by severe pruritus. Histopathological findings include subepidermal bullae and an admixture of inflammatory cells with a predominance of eosinophils, varying amounts of mononuclear cells and occasional infiltration of neutrophils into the bullae and superficial dermis, extending some times to the mid-dermis. We report a case of bullous pemphigoid with typical clinicopathologic features and a unique presentation of neutrophils arranged linearly along the basal layer.
A 71-year-old man presented with a 3-month history of recurring edematous and erythematous plaques over the trunk and extremities and also complained of severe itching. Although he was initially diagnosed with eczema, for which treatment had been given, his symptoms persisted and he experienced repeated relapses with varying degrees of severity. In the week before his hospital visit, blisters which crusted after rupture occurred on both normal appearing and erythematous areas.
Examination revealed edematous, erythematous plaques scattered over the trunk and extremities and multiple vesicles and bullae with erosions and crusts on the erythematous macules [Figure - 1]. A biopsy of an edematous erythematous plaque with a central vesicle was taken and the histopathological findings revealed a subepidermal blister containing eosinophils, lymphocytes and a limited number of neutrophils. Focal and dense infiltrates of eosinophils and lymphocytes were noted around the superficial and mid-dermal vessels [Figure - 2]a. In addition some neutrophils were arranged linearly along the basal layer [Figure - 2]b and c. Direct immunofluorescence revealed linear deposition of IgG and C3 along the basement membrane [Figure - 3]a and b. ELISA screening showed BP180 levels of 30.99 U/mL, which is well above the established limit for positivity (≥9 U/mL). Based on the clinicopathological findings and the results of the immunofluorescence examination, a diagnosis of bullous pemphigoid was made.
 |
| Figure 1: Erythematous, edematous plaques, multiple vesicles and bullae scattered over the right upper extremity, accompanied by erosions and scabs on the erythematous skin |
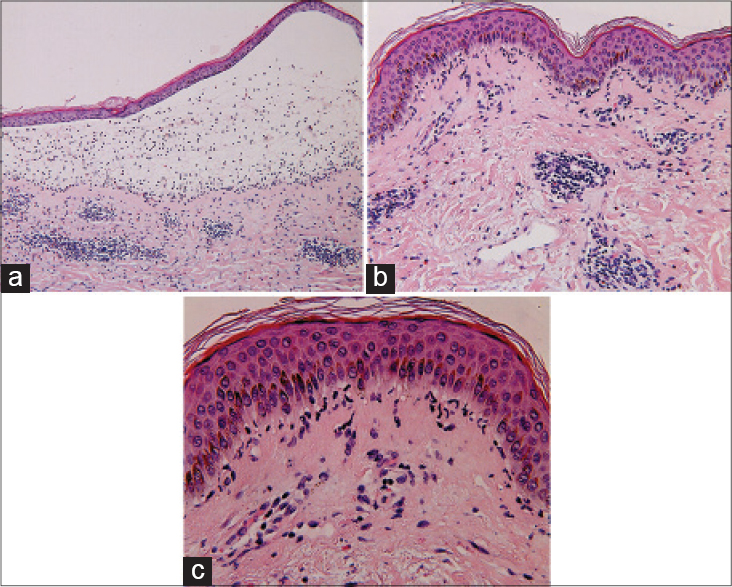 |
| Figure 2: (a) Subepidermal blisters. The blister cavity contains sporadic eosinophils, lymphocytes and occasional neutrophils. Infiltrates of eosinophils and lymphocytes are noted around the superficial and mid-dermal vessels (H and E, ×100). (b and c) Linear arrangement of neutrophils along the basal layer (H and E, ×200) and (H and E, ×400), respectively |
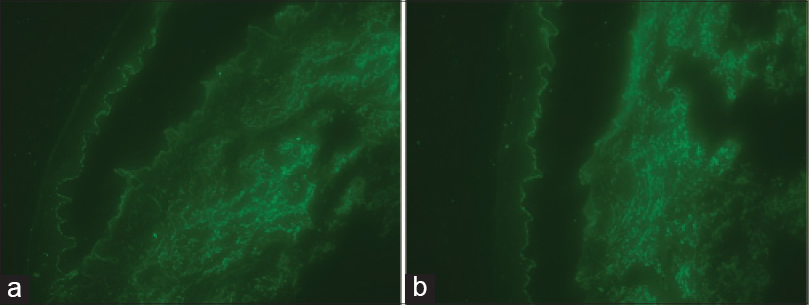 |
| Figure 3: (a) Linear deposition of IgG along the basement membrane zone (Direct immunofluorescence staining for IgG, ×200). (b) Linear deposition of C3 along the basement membrane zone (Direct immunofluorescence staining for C3, ×200) |
The present case with neutrophils along the basal layer should be differentiated from linear IgA bullous disease, inflammatory epidermolysis acquisita and bullous lupus erythematosus. In addition, neutrophil infiltration in bullous pemphigoid may be due to anti-p200 pemphigoid, also known as antilaminin-gamma 1 pemphigoid. This variant differs from bullous pemphigoid in having more frequent cephalic, acral and mucous membrane involvement as well as a greater degree of miliary scarring, early neutrophil infiltration but with no eosinophilia on biopsy and negative results on ELISA screening for anti-BP180 and anti-BP230 antibodies. Mucosal pemphigoid shows a similar histological pattern, even though it presents with very different clinical manifestations.
In 2012, Andrachuk et al. reported a 59-year-old woman presenting with a 1-month history of a pruritic blistering eruption that was clinically compatible with bullous pemphigoid. [1] Histopathologically, there were subepidermal blisters with an infiltrate of neutrophils and lymphocytes in the upper dermis and a linear arrangement of neutrophils along the basal layer which mimicked linear IgA bullous dermatosis. However, in our case, the upper dermal infiltrate was composed mainly of eosinophils and lymphocytes. The significance of a linear arrangement of neutrophils along the basal layer in bullous pemphigoid is unclear, although it may be associated with the heterogeneity of the histopathological manifestations of bullous pemphigoid. [1]
BP180, a key pathogenic antigen of bullous pemphigoid, is a transmembrane glycoprotein in hemidesmosomes, which has an important role in maintaining the structure of the epidermal-dermal junction. The interaction of BP180 with autoantibodies can induce a series of autoimmune cascade reactions, such as complement activation, mast cell degranulation and inflammatory cell (neutrophil and eosinophil) aggregation. [2] During the initial stages of bullous pemphigoid, the production and release of matrix metalloproteinases following the influx of a large number of eosinophils that were found to cluster at the dermal-epidermal junction may contribute to subepidermal blister formation via cleavage of BP180.
However, neutrophils have been observed as the main infiltrating cells during the initial stages of bullous pemphigoid in animal models so it has been proposed that neutrophils are important effector cells in the pathogenesis of the disease. [3],[4] Complement factors are activated when IgG in the antigen-antibody complex combines with the Fc receptor of immunoglobulins in neutrophils (FcR III) which contributes to rapid activation and proliferation of neutrophils, and the subsequent release of large amounts of neutrophil proteases, including neutrophil elastase, cathepsin G, and gelatinase B. These proteases collaborate to cleave extracellular matrix components including BP180, resulting in dermal-epidermal separation. [5] From these findings, it appears that usually eosinophils are effector cells in the physiopathologic process of bullous pemphigoid but occasionally neutrophils may take on this role, especially in the pre-bullous phase.
| 1. |
Andrachuk L, Ghazarian D, Siddha S, Al Habeeb A. Linear arrangement of neutrophils along the Basal layer in bullous pemphigoid: A unique histological finding. Am J Dermatopathol 2012;34:192-3.
[Google Scholar]
|
| 2. |
Ujiie H, Nishie W, Shimizu H. Pathogenesis of bullous pemphigoid. Immunol Allergy Clin North Am 2012;32:207-15.
[Google Scholar]
|
| 3. |
Liu Z, Diaz LA, Troy JL, Taylor AF, Emery DJ, Fairley JA, et al. A passive transfer model of the organ-specific autoimmune disease, bullous pemphigoid, using antibodies generated against the hemidesmosomal antigen, BP180. J Clin Invest 1993;92:2480-8.
[Google Scholar]
|
| 4. |
Liu Z, Giudice GJ, Zhou X, Swartz SJ, Troy JL, Fairley JA, et al. A major role for neutrophils in experimental bullous pemphigoid. J Clin Invest 1997;100:1256-63.
[Google Scholar]
|
| 5. |
Verraes S, Hornebeck W, Polette M, Borradori L, Bernard P. Respective contribution of neutrophil elastase and matrix metalloproteinase 9 in the degradation of BP180 (type XVII collagen) in human bullous pemphigoid. J Invest Dermatol 2001;117:1091-6.
[Google Scholar]
|
Fulltext Views
3,205
PDF downloads
3,022





