Translate this page into:
Pyoderma gangrenosum in successive pregnancies
Correspondence Address:
Chintagunta Sudha Rani
Department of Dermatology, Venereology and Leprology, Gandhi Medical College, Hyderabad - 500 025, Telangana
India
| How to cite this article: Rani CS, Kiran AG, Vani DS, Devi EN. Pyoderma gangrenosum in successive pregnancies. Indian J Dermatol Venereol Leprol 2015;81:548 |
Sir,
Pyoderma gangrenosum is a chronic non-infectious ulcerative condition of skin often associated with systemic diseases like inflammatory bowel disease, rheumatological or hematological diseases. Immunological alterations in pregnancy play a role in the development of pyoderma gangrenosum in susceptible individuals. Pregnancy-associated pyoderma gangrenosum is rare. We report a case of pyoderma gangrenosum occurring in the first trimester in four consecutive pregnancies in a woman without any underlying systemic diseases.
A 25-year-old woman presented in her fourth pregnancy at 20 weeks of amenorrhoea with multiple non-healing ulcers over the legs, buttocks and dorsum of hands and feet. The ulcers started within 2 weeks of conception as vesiculopustular lesions and progressed to painful necrotic ulcers. There was no history of fever, arthralgia/arthritis or of drug intake. Signs and symptoms suggestive of systemic involvement were absent. The patient had had similar skin lesions at 10-12 weeks of gestation in the previous three pregnancies. During the first pregnancy, there was no response to medical therapy hence skin grafting was done at 32 weeks of gestation. Two days later she delivered a still-born child. The skin lesions completely healed within 1 month in the postpartum period. During the second pregnancy, she delivered a full term live child and the lesions healed after delivery. She aborted at 20 weeks in the third pregnancy, which was followed by complete healing of lesions.
Cutaneous examination revealed a large ulcer about 15-20 cm on the lower two-third of left leg [Figure - 1]. The floor was covered with granulation tissue and the edges were well defined, edematous and pale to bluish in color. Similar lesions of 3-5 cm in size were present over the hands, feet and buttocks [Figure - 2] with atrophic scars over the legs. Systemic and general examination was unremarkable.
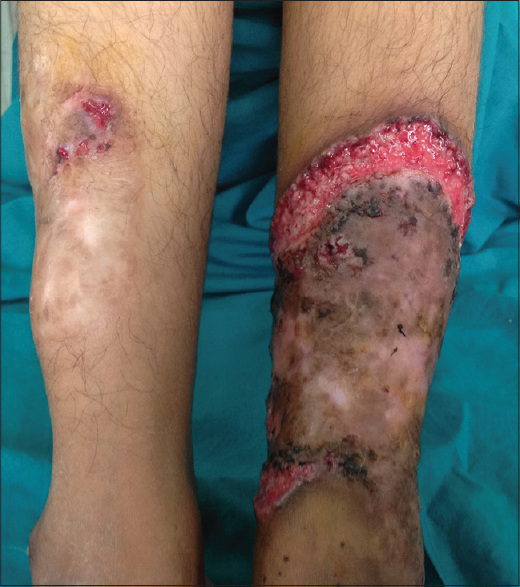 |
| Figure 1: Well defined ulcer showing edematous pale bluish border with granulation tissue on the left leg |
 |
| Figure 2: Similar ulcers on the buttock |
Routine investigations were normal. Serological tests for syphilis, hepatitis B and hepatitis C virus and human immunodeficiency virus were non-reactive. Tests for rheumatoid factor, C-reactive protein and anti nuclear antibodies were negative. Pus for bacterial culture was negative. Pathergy test was positive. Targeted imaging for fetal anomalies by ultrasonography showed a single live fetus of 20 weeks gestation. Skin biopsy revealed focal ulceration of the epidermis along with a predominantly neutrophilic inflammatory infiltrate in the dermis. Based on clinical findings and excluding other causes of non-healing ulcers, a diagnosis of pyoderma gangrenosum was made. As the lesions were extensive and extremely painful, the patient was started on prednisolone 30 mg/day tapered by 5 mg every 2 weeks. There was complete resolution of lesions with atrophic scars [Figure - 3]. The patient delivered a full term baby and both mother and child are doing well.
 |
| Figure 3: Resolution of the lesion after treatment |
Pyoderma gangrenous is presently considered a reactive inflammatory condition that belongs to the group of neutrophilic dermatoses. [1] The exact etiopathogenesis is not known and immunological alterations and neutrophilic dysfunction are hypothesized. [2] A total of 25-50% of cases are idiopathic and 50% are associated with immune mediated systemic disorders. It is common between 20 to 50 years of age but can occur at any age. It frequently occurs on the lower extremities and trunk. Lesions can be single or multiple, chronic or recurrent. The occurrence of pyoderma gangrenosum during pregnancy is rare. A literature search revealed 17 case reports associated with pregnancy. Wierzbicka-Hainaut et al. reported a patient with this condition during the third trimester in two pregnancies [3] whereas in our case it occurred during the first trimester in four successive pregnancies. Sapna et al. reported a case of pyoderma gangrenosum at the Caesarean wound site in two successive pregnancies. [4]
The hypothesis for the occurrence of pyoderma gangrenosum is altered or defective immune processes. Immunological changes occurring in pregnancy are immune-suppression with altered humoral and cell mediated immunity, inhibition of IL2 and IL1 activity and decreased polymorphonuclear leukocyte chemotaxis and adherence functions. These altered immune functions could play a role in the development of pyoderma gangrenosum during pregnancy.
Pyoderma gangrenosum in pregnancy, without any pathological association, suggests that there is a link between pregnancy and the condition per se. This could be explained by pathergy phenomenon or neutrophil activation due to increased secretion of granulocyte-colony stimulating factor or an inappropriate response to the receptors of the same molecule after their stimulation during pregnancy. [5] Occurrence of this condition in pregnancy appears to have no impact on the development of the fetus and no neonatal morbidity has been observed.
Interestingly, our patient presented with pyoderma gangrenosum in the first trimester in four consecutive pregnancies without any underlying immune mediated systemic disorders, unlike earlier reports. Skin lesions were multiple and progressive until delivery in the previous three pregnancies and healed after delivery. In the present pregnancy, a dramatic response was observed with a moderate dose of systemic steroids. Pregnancy appeared to be the only triggering factor in our patient.
| 1. |
Su WP, Davis MO, Weenig RH, Powell FC, Perry HO. Pyoderma gangrenosum: Clinicopathologic correlation and proposed diagnostic criteria. Int J Dermatol 2004;43:790-800.
[Google Scholar]
|
| 2. |
Bhat RM, Nanda Kishore B, Sequeira FF, Sukumar D, Kamath GH, Martis J, et al. Pyoderma gangrenosum: An Indian perspective. Clin Exp Dermatol 2011;36:242-7.
[Google Scholar]
|
| 3. |
Amin SV, Bajapai N, Pai A, Bharatnur S, Hebbar S. Pyoderma gangrenosum in two successive pregnancies complicating caesarean wound. Case Rep Obstet Gynecol 2014;2014:654843.
[Google Scholar]
|
| 4. |
Wierzbicka-Hainaut E1, Le Naoures H, Bonneric-Malthieu F, Debiais P, Levillain P, Pierre F, et al. Recurring pyoderma gangrenosum in pregnancy. Ann Dermatol Venereol 2010;137:225-9.
[Google Scholar]
|
| 5. |
White LE, Villa MT, Pertronic-Rosic V, Jiang J, Medinica MM. Pyoderma gangrenosum related to a new granulocyte colony stimulating factor. Skinmed 2006;5:96-8.
[Google Scholar]
|
Fulltext Views
1,873
PDF downloads
1,220





