Translate this page into:
Guidelines for bath PUVA, bathing suit PUVA and soak PUVA
Correspondence Address:
Shricharith Shetty
Department of Dermatology, Kasturba Medical College, Manipal University, Manipal - 576 104, Karnataka
India
| How to cite this article: Pai SB, Shetty S. Guidelines for bath PUVA, bathing suit PUVA and soak PUVA. Indian J Dermatol Venereol Leprol 2015;81:559-567 |
Abstract
Background: The aim of these guidelines is to encourage dermatologists to use bath psoralen plus ultraviolet A (PUVA), bathing suit PUVA and soak PUVA in the treatment of psoriasis vulgaris and other conditions. Methods: Evidence was collected using searches of the PubMed, MEDLINE and COCHRANE databases using the keywords “bath PUVA,” “soak PUVA,” “bathing suit PUVA” and “turban PUVA.” Only publications in English were reviewed. Results: One hundred and thirty-eight studies were evaluated, 57 of which fulfilled the criteria for inclusion. Conclusions: Both bath PUVA and bathing suit PUVA are very effective and safe treatments for generalized stable plaque psoriasis (strength of recommendation, A). Soak PUVA is very effective in the treatment of both palmoplantar psoriasis and chronic palmoplantar eczema (strength of recommendation, A).Introduction
Psoralen plus ultraviolet A (PUVA) photochemotherapy combines the use of psoralen and long-wave ultraviolet A (UVA) radiation. Psoralen bath plus UVA therapy is known as bath PUVA therapy. Bath PUVA treatment for psoriasis was first reported by Fischer and Alsins in 1976.[1] It has since been recognized as an important and effective tool for treating psoriasis.[2],[3],[4],[5],[6] Studies have shown that bath PUVA is as effective as oral PUVA in the treatment of psoriasis.[7],[8],[9],[10] It also avoids the adverse effects associated with oral PUVA therapy and is being increasingly used in the treatment of psoriasis.[11] Concentrations of 8-methoxy psoralen ranging from 0.5 to 4.6 mg/L have been used.[4],[5],[6] In India, where bathtubs are not in vogue and water shortages are perennial, bathing suit PUVA is an alternative, and effective therapy in psoriasis. Turban PUVA is yet another similar alternative useful in treating conditions affecting the scalp. In cases where only the hands and feet are affected, soak PUVA (basin PUVA) can be used. In all these treatment methods, sunlight can also be used as a source of UVA rays.
These guidelines are intended to encourage the use of bath PUVA, bathing suit PUVA and soak PUVA by dermatologists in the treatment of psoriasis and other conditions.
Definition
Bath PUVA therapy involves the immersion of the entire body in psoralen solution followed by exposure to UVA. In bathing suit PUVA, a suit made of absorbent material is soaked in a psoralen solution. The patient wears the suit for a fixed duration and is then exposed to UVA rays. In soak PUVA, the affected part (hand or foot) is immersed in psoralen solution for a fixed duration and then exposed to UVA rays in a UVA hand and foot unit.
Rationale
The rationale of topical PUVA therapy (bath PUVA, bathing suit, soak PUVA) is to induce a controlled phototoxic reaction without the systemic side effects associated with oral PUVA therapy.
Mechanism of action of PUVA in psoriasis
The phototherapeutic effects of PUVA result from photochemical reactions. In molecules in their normal ground state, electrons have a specific distribution in the space around the atomic nuclei. When a molecule in this ground state absorbs the energy of a UV photon, the molecule shifts to a higher energy excited state called the singlet excited state, which exists for a few nanoseconds. The molecule may then return to the ground state or it may form a photoproduct. An important example is the formation of covalent adducts between psoralen and DNA. First, the psoralen molecule enters the cell nucleus and intercalates between the stacked nucleic acid bases. When the skin is exposed to ultraviolet A rays, the psoralen molecule absorbs a photon and gets excited. The excited-state psoralen covalently binds to the pyrimidine base forming a photo - adduct. This photo-adduct absorbs another UVA photon and links to a pyrimidine base on the complementary DNA strand, forming a DNA-psoralen crosslink. These crosslinks are toxic to cells and are important for the effect of PUVA in psoriasis.[12] PUVA therapy has also been shown to downregulate the Th1/Th17 pro-inflammatory axis and upregulate the counter-regulatory Th2 pathway, leading to clinical improvement.[13]
Methods
Searches of the PubMed, MEDLINE and the COCHRANE databases for the years 1978 to 2015 were carried out using the keywords “bath PUVA,” “soak PUVA,” “bathing suit PUVA” and “turban PUVA". Only publications in English were reviewed. The available evidence was evaluated using guidelines suggested by the British Association of Dermatologists.[14] The methodology of each study selected was assessed as per the National Institute of Clinical Excellence Technical Manual and graded as “++,” “+” or “−,” based on the extent to which potential biases were minimized. Thereafter, a grade of recommendation was assigned as follows: Grade A, at least one meta-analysis, systematic review, or randomized controlled trial rated as 1++, and directly applicable to the target population, or a systematic review of randomized controlled trials or a body of evidence consisting principally of studies rated as 1+, directly applicable to the target population and demonstrating overall consistency of results; Grade B, a body of evidence including studies rated as 2++, directly applicable to the target population and demonstrating overall consistency of results, or extrapolated evidence from studies rated as 1++ or 1+; Grade C, a body of evidence including studies rated as 2+, directly applicable to the target population and demonstrating overall consistency of results, or extrapolated evidence from studies rated as 2++: Grade D, evidence level 3 or 4, or extrapolated evidence from studies rated as 2+, or formal consensus.[14]
Facilities required and procedure
Bath PUVA
A separate room with non-skid tiles and a bathtub with markings for 50, 65, 80 and 100 litres are needed, as also a geyser to provide warm water especially during the rainy season and winter.
The bathtub is filled with 100 litres of warm water using separate taps for hot and cold water. Next, 37.5 ml of 1% 8-methoxypsoralen is added to obtain a concentration of 3.75 mg/L. A lower concentration of 2.6 mg/L can also be used.[11] The patient then soaks their body for 10 minutes in the supine position and 10 min in the prone position. The whole body is immersed to ensure maximum coverage, avoiding splashing the face and eyes with the solution. The patient may also gently agitate the water while soaking. After 20 minutes of soaking, the patient comes out of the tub, gently pats the skin dry and is then immediately exposed to UVA in a whole-body UVA phototherapy chamber. The eyes should be protected with UVA-protective goggles and men need to cover their genitalia with dark undergarments. The bathtub used should be cleaned with liquid soap and rinsed thoroughly before another patient uses it.
The treatment is given 3 times a week. Clearance is usually seen with 12–15 treatments. After clearance, the patient is generally given maintenance treatments for another 2–3 months, twice weekly for the first month and then once weekly. However, if the patient cannot attend maintenance therapy sessions, treatment can be stopped after clearance.
Ultraviolet A chamber
A whole-body UVA chamber is used. Measuring the output of the phototherapy chamber is important, as this ensures that patients receive the doses required for optimal outcomes. Inbuilt dosimetry has been found to be unreliable.[15] It is better to check the output of the chambers manually. The photometer should be calibrated at least once a year. The output of the chamber should also be checked when old tubes are replaced with new ones. It is better not to put two new tubes together because that part of the chamber would then emit more light.
Ultraviolet A protocol
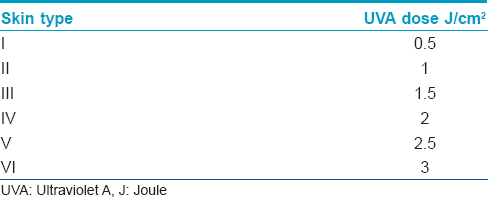
The starting dose of UVA is between 1 and 2 J/cm 2 with increments of 0.5 J/cm 2 at each treatment session, provided there is no erythema. Erythema is the limiting factor with regard to the UVA dose that can be given at each treatment. Though phototoxicity testing to establish the minimal phototoxic dose is ideal, it is difficult to assess on Indian skin. Hence, the UVA dose may be based on skin type instead [Table - 1].
Post-bath PUVA care
Post-treatment bathing is not required as cutaneous absorption and binding dynamics suggest that no free psoralen remains on the skin surface. However, the exposed parts of the body should be protected from sunlight.[12]
Bathing suit PUVA
A plastic bucket, a bathing suit made up of water absorbing material (flannel) and a rain coat is required.
Two liters of water are taken in a bucket and 1 ml of 1% 8-methoxypsoralen added to obtain a concentration of 3.75 mg/L. A bathing suit of flannel material (stitched to suit the patient) is dipped in this solution for 5 minutes, then taken out and gently squeezed to remove excess solution. The patient wears this suit for 15 minutes with a raincoat over it to prevent evaporation of the solution and is then immediately exposed to UVA in a whole-body phototherapy chamber. The starting dose of UVA is usually 1–2 J/cm 2 with increments of 0.5 J/cm 2. A total of 15–20 treatments are usually required for clearing psoriasis.
Bathing suit PUVA can also be carried out at home with sunlight as the UVA source. The duration of sun exposure needed varies from place to place. The ideal time for sun exposure is 9.15-11.15 am or 2.30-3.30 pm, when ultraviolet B and infrared radiation are minimum.[16] While sunlight is the cheapest and the most easily available source of ultraviolet radiation, disadvantages include its variation with time, place and season, lack of privacy and atmospheric conditions. The lack of privacy can be overcome with 'clothes-on PUVA,'[17] wherein a plain woven, cream-colored lightweight cotton gown (2 × 2 cotton blouse cloth) is worn during sun exposure, and the time of exposure increased by a factor of 3.33.
Soak PUVA
The affected parts (hands and/or feet) are soaked in a 3.75 mg/L solution of 8-methoxypsoralen (prepared as above) in a small plastic tub or a basin for 20 minutes and then patted dry. After another 30 minutes, the part is exposed to UVA in a hand and foot unit. Treatments are repeated 3–4 times/week, with an initial UVA dose of 1–2 J/cm 2 and increments of 0.5 J/cm 2.[18]
If sunlight is used as the UVA source, the exposure time is 4–5 minutes initially with 1-minute increments every week up to a maximum of 30 minutes.
Turban PUVA
An absorbent cotton cloth is soaked for 30 seconds in a 3.75 mg/L solution of 8-methoxypsoralen (prepared as above), gently squeezed to remove excess water and wrapped around the head for 5 minutes. This is repeated 4 times (i.e., a total of 20 minutes) and the area is then exposed to UVA or sunlight.
If sunlight is used as the source of UVA, exposure starts with 5 minutes, increased by 1 minute with each exposure up to a maximum of 15 minutes. The treatment is given 3–4 times/week for 10–12 weeks.[19],[20],[21]
Patient education
Before starting therapy, the procedure involved should be explained to the patient, Powerpoint slides and pre- and post-treatment photographs may be used where possible. Potential side effects including phototoxic reactions should be discussed and the need to adhere to the treatment regimen emphasised.
Indications
Bathwater PUVA [Table - 2]
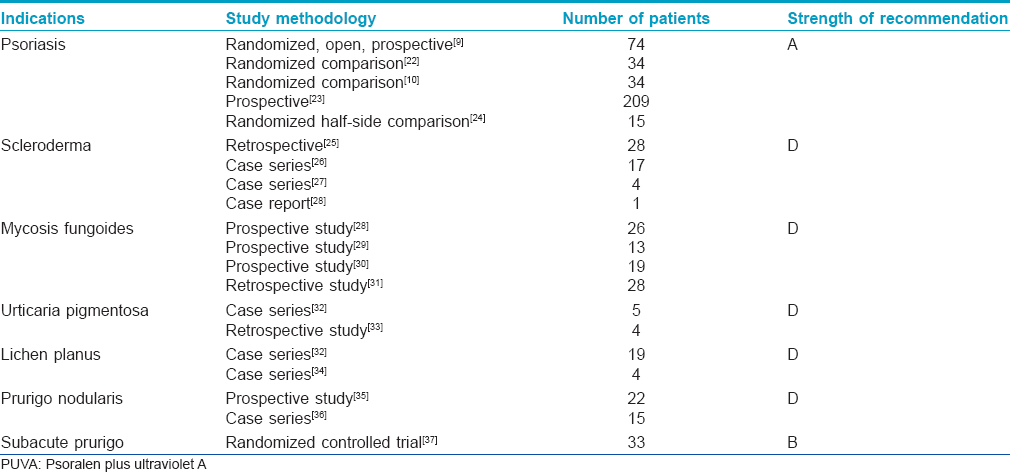
Psoriasis
Several studies have clearly demonstrated the effectiveness of bath PUVA in psoriasis. In one randomized study involving 74 patients, the median psoriasis area and severity index (PASI) score improved by 73.8% in 6 weeks in the bath PUVA group compared to 62% in the oral PUVA group.[9] Another study with 34 patients showed a significantly higher reduction in the PASI score with bath PUVA than in the narrow-band ultraviolet B group (85.4% vs. 58.7%).[22] In yet another randomized study, bath PUVA was shown to be as effective as, or more effective than, oral PUVA and required <50% of the total UVA dose of the latter.[10] A prospective studyinvolving 209 patients with psoriasis demonstrated good response in 93.3% of patients on bath PUVA.[23] However, one randomized half-side comparative study between bath PUVA and narrow band-ultraviolet B found the latter to be more efficient and better tolerated.[24]
Scleroderma
A retrospective study of 28 patients with localized scleroderma treated with bath PUVA showed complete remission in 11, partial softening and regression in 14, and no effect in 3 patients.[25] Another study noted good improvement in induration in 13 out of 17 consecutive patients evaluated.[26] Three cases of progressive systemic sclerosis and one of generalized morphea improving with 3–8 weeks of bath PUVA.[27] and a case of disseminated scleroderma showing marked improvement though requiring high cumulative UVA doses have also been reported.[38]
Mycosis fungoides
In a prospective study of 26 patients (14 with folliculotropic mycosis fungoides and 12 with narrow band-ultraviolet B-refractory early-stage mycosis fungoides), complete clinical response was achieved in 62% of patients after an average of 33 weeks and a cumulative radiation dose of 158 J/cm 2.[28] Further, a study of 13 patients with mycosis fungoides showed bath PUVA therapy decreasing infiltrating CCR4-expressing tumor cells and regulatory T-cells in mycosis fungoides lesions, though systemic immunosuppression was not induced.[29] Complete or almost complete healing was noted with bath PUVA in all 3 patients with parapsoriasis en plaques, all 7 with mycosis fungoides stage II and in 4 of 5 with mycosis fungoides stage III in another study. However, one patient with Sezary syndrome and another with erythrodermic mycosis fungoides were reported to have responded with severe phototoxic reactions.[30] A retrospective study of childhood mycosis fungoides noted favorable response rates with both bath PUVA and narrow band-ultraviolet B, but remissions appeared to be longer with bath PUVA.[31]
Urticaria pigmentosa
All 5 patients of urticaria pigmentosa on bath PUVA in one series showed good results with respect to whealing, itching and dermographism; in one of them the lesions disappeared completely.[32] However a later retrospective study of urticaria pigmentosa and mastocytosis failed to find any therapeutic effect with bath PUVA in any of the 4 patients included.[33]
Lichen planus
Out of 19 patients with lichen planus in one study, all 16 with widespread papular lesions healed completely with bath PUVA. The hypertrophic variant was noted to be more resistant to treatment with 2 out of 3 recovering completely, and one with a good response.[32] Others have also shown good results with bath PUVA in long-standing cases of lichen planus.[34]
Prurigo nodularis
Bath PUVA produced good healing of prurigo nodularis in a prospective trial of 22 patients. Adding 308 nm excimer ultraviolet B sped up the healing process and reduced the PUVA dose by 30% in this study.[35] Other investigators found good to excellent results in 13 out of 15 patients studied, in reaching the maintenance phase of treatment with bath PUVA.[36]
Subacute prurigo
A randomized, controlled, three-arm study with 33 patients showed significantly higher reductions in clinical signs with bath PUVA and medium dose ultraviolet A 1 than with narrow band-ultraviolet B treatment.[37]
Hidradenitis suppurativa
A retrospective study of 13 patients with hidradenitis suppurativa treated with bath PUVA found 5 patients to have achieved clearing or near-clearing at the end of the course; in 4 of them, the response was sustained at 3 months' follow-up. Four patients showed no or minimal” improvement.[39]
Graft-versus-host disease
Two cases of severe cutaneous sclerodermic chronic graft-versus-host disease (GVHD) following allogeneic stem cell transplantation responding well to bath PUVA have been reported, with cumulative doses of about 90 J/cm 2 of UVA having been used.[40] A retrospective study of chronic graft-versus-host disease noted that bath PUVA alone or in combination with isotretinoin may resolve or improve graft-versus-host disease-associated sclerosis.[41] In another study 3 out of 6 patients suffering from severe chronic graft-versus-host disease of the skin who did not respond to immunosuppressive therapy or relapsed after reduction of corticosteroids showed complete remission.[42] Four pediatric patients with drug-resistant cutaneous graft-versus-host disease treated successfully with bath PUVA have also been reported.[43]
Other indications
Bath PUVA has also been reported to be useful in lymphomatoid papulosis, eosinophilic fasciitis, keratosis lichenoides chronica, disseminated pagetoid reticulosis, generalized granuloma annulare, lichen amyloidosis, scleredema, aquagenic pruritus and childhood vitiligo.[44],[45],[46],[47],[48],[49],[50],[51],[52],[53],[54]
Bathing suit PUVA
Psoriasis
A randomized controlled study with 24 Indian patients of stable plaque-type psoriasis involving more than 20% of the body surface found good improvement in 75% of the patients using bathing suit PUVA.[55]
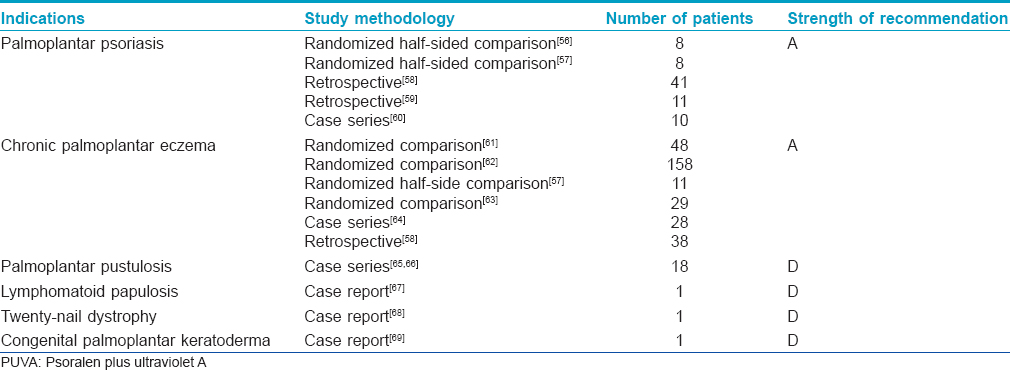
Soak PUVA
Soak PUVA is indicated primarily in palmoplantar dermatoses [Table - 3].
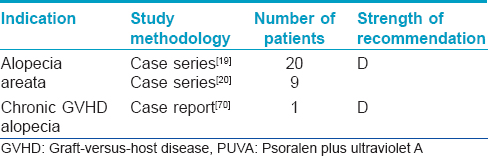
Turban PUVA
Turban PUVA therapy is mainly used in the treatment of alopecia areata [Table - 4].
Contraindication
Generalized unstable psoriasis.
Special groups
Children
Bucket PUVA
This option is useful in children, in whom oral psoralens are best avoided. A plastic bucket of appropriate size with markings for litres may be used instead of a bathtub. If such a bucket is not available, markings can be made on the outer side of any bucket. The child is placed in the bucket and water poured till a suitable level. The child is then removed and the amount of water required recorded. Before each phototherapy session, water is filled up to the required level in the bucket and 8-methoxy psoralen solution added as described above. The water can be agitated using a long stick to avoid the solution coming in contact with the forearms and hand of the person preparing the solution. The child is first placed in the bath as advised for bath PUVA and then exposed to UVA. Alternatively, treatment may be carried out when the child returns from school with sunlight as the UVA source, provided there is adequate light. (Dr. C R Srinivas, personal communication).
Adverse effects
- Skin phototoxicity: The most common adverse effect is phototoxic erythema, and this is more common during the first five treatments.[71],[72] It is recommended that adequate photoprotective measures be taken by patients both during the course of treatment and up to a week after the course is completed
- Pruritus: The incidence of pruritus following bath PUVA is about 10–40%[1]
- Folliculitis [7]
- Pigmentation [7]
- Contact and photocontact dermatitis: Rare, but have been reported with bath PUVA [73]
- Skin cancer: Bath PUVA is as carcinogenic as oral PUVA. It is therefore recommended, as for oral PUVA, to keep bath PUVA treatments to a minimum.[74] There are no Indian data on how many bath PUVA treatments a patient can receive. A combined analysis of two cohort studies (944 patients treated with bath PUVA) found no increase in the risk of squamous cell carcinoma after a mean follow-up of 14.7 years (standardized incidence ratio 1.1, 95% confidence interval: 0.2–3.2), suggesting that bath PUVA is possibly safer than conventional PUVA [75]
- Eye phototoxicity: There is no published evidence of an increased incidence of cataract development in humans following bath PUVA treatment. It has been shown that higher PASI scores are associated with higher plasma levels of psoralen.[76] In the UK, UVA protective glasses are advised on the day of treatment for patients with psoriasis involving more than 30% of the body surface area. We do not advise eye protection after bath PUVA in Indian patients.
Advantages and disadvantages
Bath PUVA
Advantages
- There are no associated systemic side effects, unlike with oral PUVA
- The total ultraviolet A dose required for bath PUVA is 3–6 times lower than oral PUVA.[74]
Disadvantages
- The time for each session is longer; some extra space is required and additional staff are needed to supervise bathing and to clean the tub between patients
- Exposure to UVA needs to be done immediately after soaking in the psoralen solution as photosensitivity declines rapidly.[77]
Bath PUVA is rarely used in the United States due to the high cost of establishing an efficient bath PUVA unit, and since their Food and Drug Administration has not approved bath PUVA with trimethylpsoralen.[78]
Bathing suit PUVA
Advantages
- This method requires only 2 litres of water and 1 ml of psoralen solution per treatment
- Therapy can be carried out at home with sunlight as the UVA source.
Disadvantages
- The entire body surface may not come in contact with the bathing suit
- The concentration of psoralen may not be uniform in the bathing suit.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Fischer T, Alsins J. Treatment of psoriasis with trioxsalen baths and[80] dysprosium lamps. Acta Derm Venereol 1976;56:383-90.
[Google Scholar]
|
| 2. |
Väätäinen N, Hannuksela M, Karvonen J. Long-term local trioxsalen photochemotherapy in psoriasis. Dermatologica 1981;163:229-31.
[Google Scholar]
|
| 3. |
Lauharanta J, Geiger JM. A double-blind comparison of acitretin and etretinate in combination with bath PUVA in the treatment of extensive psoriasis. Br J Dermatol 1989;121:107-12.
[Google Scholar]
|
| 4. |
Collins P, Rogers S. Bath-water delivery of 8-methoxypsoralen therapy for psoriasis. Clin Exp Dermatol 1991;16:165-7.
[Google Scholar]
|
| 5. |
Gomez M, Perez B, Harto A, Misa R, Lido A. 8-MOP bath PUVA in the treatment of psoriasis; clinical results in 42 patients. J Dermatol Treat 1996;7:11-2.
[Google Scholar]
|
| 6. |
Streit V, Wiedow O, Christophers E. Treatment of psoriasis with polyethylene sheet bath PUVA. J Am Acad Dermatol 1996;35(2 Pt 1):208-10.
[Google Scholar]
|
| 7. |
Sridhar KS, Srinivas CR, Shenoi SD. PUVA therapy for psoriasis, comparision of oral and bath water delivery of 8-MOP. Indian J Dermatol Venereol Leprol 1992;58:252-4.
[Google Scholar]
|
| 8. |
Karrer S, Eholzer C, Ackermann G, Landthaler M, Szeimies RM. Phototherapy of psoriasis: Comparative experience of different phototherapeutic approaches. Dermatology 2001;202:108-15.
[Google Scholar]
|
| 9. |
Berneburg M, Herzinger T, Rampf J, Hoetzenecker W, Guenova E, Meisner C, et al. Efficacy of bath psoralen plus ultraviolet A (PUVA) vs. system PUVA in psoriasis: A prospective, open, randomized, multicentre study. Br J Dermatol 2013;169:704-8.
[Google Scholar]
|
| 10. |
Cooper EJ, Herd RM, Priestley GC, Hunter JA. A comparison of bathwater and oral delivery of 8-methoxypsoralen in PUVA therapy for plaque psoriasis. Clin Exp Dermatol 2000;25:111-4.
[Google Scholar]
|
| 11. |
Lüftl M, Degitz K, Plewig G, Röcken M. Psoralen bath plus UV-A therapy. Possibilities and limitations. Arch Dermatol 1997;133:1597-603.
[Google Scholar]
|
| 12. |
Kochevar IE, Taylor CR, Krutmann J. Fundamentals of cutaneous photobiology and photoimmunology. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology in General Medicine. 7th ed. New York: McGraw Hill; 2008. p. 804.
[Google Scholar]
|
| 13. |
Wong T, Hsu L, Liao W. Phototherapy in psoriasis: A review of mechanisms of action. J Cutan Med Surg 2013;17:6-12.
[Google Scholar]
|
| 14. |
Bell HK, Ormerod AD, BAD Therapy and Guidelines Subcommittee. Writing a British Association of Dermatologists clinical guideline: An update on the process and guidance for authors. Br J Dermatol 2009;160:725-8.
[Google Scholar]
|
| 15. |
Moseley H. Phototest equipment. In: Ferguson J, Dover JS, editors. Photodermatology. 1st ed. London: Manson Publishing Ltd.; 2007. p. 20.
[Google Scholar]
|
| 16. |
Balasaraswathy P, Kumar U, Srinivas CR, Nair S. UVA and UVB in sunlight, optimal utilization of UV rays in sunlight for phototherapy. Indian J Dermatol Venereol Leprol 2002;68:198-201.
[Google Scholar]
|
| 17. |
Varma S, Ballambat SP, Balachandran C, Shenoi SD, Prabhu S. Clothes-on PUVA in psoriasis: Single blind randomized comparative trial on 21 patients. Indian J Dermatol Venereol Leprol 2004;70:152-5.
[Google Scholar]
|
| 18. |
Konya J, Diffey BL, Hindson TC. Time course of activity of topical 8-methoxypsoralen on palmoplantar skin. Br J Dermatol 1992;127:654-6.
[Google Scholar]
|
| 19. |
Broniarczyk-Dyla G, Wawrzycka-Kaflik A, Dubla-Berner M, Prusinska-Bratos M. Effects of psoralen-UV-A-Turban in alopecia areata. Skinmed 2006;5:64-8.
[Google Scholar]
|
| 20. |
Behrens-Williams SC, Leiter U, Schiener R, Weidmann M, Peter RU, Kerscher M. The PUVA-turban as a new option of applying a dilute psoralen solution selectively to the scalp of patients with alopecia areata. J Am Acad Dermatol 2001;44:248-52.
[Google Scholar]
|
| 21. |
Sornakumar L, Sekar CS, Srinivas C. Turban PUVASOL: An Effective Treatment in Alopecia Totalis. Int J Trichology 2010;2:106-7.
[Google Scholar]
|
| 22. |
Salem SA, Barakat MA, Morcos CM. Bath psoralen+ultraviolet A photochemotherapy vs. narrow band-ultraviolet B in psoriasis: A comparison of clinical outcome and effect on circulating T-helper and T-suppressor/cytotoxic cells. Photodermatol Photoimmunol Photomed 2010;26:235-42.
[Google Scholar]
|
| 23. |
Rodríguez-Granados MT, Pereira-Rodríguez MJ, Vázquez-Vizoso FL. Therapeutic effectiveness of psoralen-UV-A bath therapy in psoriasis. Actas Dermosifiliogr 2009;100:212-21.
[Google Scholar]
|
| 24. |
Snellman E, Klimenko T, Rantanen T. Randomized half-side comparison of narrowband UVB and trimethylpsoralen bath plus UVA treatments for psoriasis. Acta Derm Venereol 2004;84:132-7.
[Google Scholar]
|
| 25. |
Pavlotsky F, Sakka N, Lozinski A, Barzilai A. Bath psoralen-UVA photochemotherapy for localized scleroderma: Experience from a single institute. Photodermatol Photoimmunol Photomed 2013;29:247-52.
[Google Scholar]
|
| 26. |
Kerscher M, Meurer M, Sander C, Volkenandt M, Lehmann P, Plewig G, et al. PUVA bath photochemotherapy for localized scleroderma. Evaluation of 17 consecutive patients. Arch Dermatol 1996;132:1280-2.
[Google Scholar]
|
| 27. |
Kanekura T, Fukumaru S, Matsushita S, Terasaki K, Mizoguchi S, Kanzaki T. Successful treatment of scleroderma with PUVA therapy. J Dermatol 1996;23:455-9.
[Google Scholar]
|
| 28. |
Pavlotsky F, Hodak E, Ben Amitay D, Barzilai A. Role of bath psoralen plus ultraviolet A in early-stage mycosis fungoides. J Am Acad Dermatol 2014;71:536-41.
[Google Scholar]
|
| 29. |
Kato H, Saito C, Ito E, Furuhashi T, Nishida E, Ishida T, et al. Bath-PUVA therapy decreases infiltrating CCR4-expressing tumor cells and regulatory T cells in patients with mycosis fungoides. Clin Lymphoma Myeloma Leuk 2013;13:273-80.
[Google Scholar]
|
| 30. |
Fischer T, Skogh M. Treatment of parapsoriasis en plaques, mycosis fungoides, and Sézary's syndrome with trioxsalen baths followed by ultraviolet light. Acta Derm Venereol 1979;59:171-3.
[Google Scholar]
|
| 31. |
Laws PM, Shear NH, Pope E. Childhood mycosis fungoides: Experience of 28 patients and response to phototherapy. Pediatr Dermatol 2014;31:459-64.
[Google Scholar]
|
| 32. |
Väätäinen N, Hannuksela M, Karvonen J. Trioxsalen baths plus UV-A in the treatment of lichen planus and urticaria pigmentosa. Clin Exp Dermatol 1981;6:133-8.
[Google Scholar]
|
| 33. |
Godt O, Proksch E, Streit V, Christophers E. Short- and long-term effectiveness of oral and bath PUVA therapy in urticaria pigmentosa and systemic mastocytosis. Dermatology 1997;195:35-9.
[Google Scholar]
|
| 34. |
Kerscher M, Volkenandt M, Lehmann P, Plewig G, Röcken M. PUVA-bath photochemotherapy of lichen planus. Arch Dermatol 1995;131:1210-1.
[Google Scholar]
|
| 35. |
Hammes S, Hermann J, Roos S, Ockenfels HM. UVB 308-nm excimer light and bath PUVA: Combination therapy is very effective in the treatment of prurigo nodularis. J Eur Acad Dermatol Venereol 2011;25:799-803.
[Google Scholar]
|
| 36. |
Väätäinen N, Hannuksela M, Karvonen J. Local photochemotherapy in nodular prurigo. Acta Derm Venereol 1979;59:544-7.
[Google Scholar]
|
| 37. |
Gambichler T, Hyun J, Sommer A, Stücker M, Altmeyer P, Kreuter A. A randomised controlled trial on photo(chemo) therapy of subacute prurigo. Clin Exp Dermatol 2006;31:348-53.
[Google Scholar]
|
| 38. |
Aragane Y, Kawada A, Maeda A, Isogai R, Isogai N, Tezuka T. Disseminated scleroderma of a Japanese patient successfully treated with bath PUVA Photochemotherapy. J Cutan Med Surg 2011;5:135-9.
[Google Scholar]
|
| 39. |
Shareef M, Dawe R. Bath psoralen plus ultraviolet A for hidradenitis suppurativa: A review of 13 patients. Br J Dermatol 2011;164:895-6.
[Google Scholar]
|
| 40. |
Hoffner MV, Carrizosa Esquivel A, Pulpillo Ruiz A, Herrera Saval A, Conejo-Mir J, Camacho FM. Two cases of cutaneous chronic graft versus host disease in treatment with psoralen plus ultraviolet-A-bath photochemotherapy. J Drugs Dermatol 2009;8:1027-9.
[Google Scholar]
|
| 41. |
Ghoreschi K, Thomas P, Penovici M, Ullmann J, Sander CA, Ledderose G, et al. PUVA-bath photochemotherapy and isotretinoin in sclerodermatous graft-versus-host disease. Eur J Dermatol 2008;18:667-70.
[Google Scholar]
|
| 42. |
Leiter U, Kaskel P, Krähn G, Gottlöber P, Bunjes D, Peter RU, et al. Psoralen plus ultraviolet-A-bath photochemotherapy as an adjunct treatment modality in cutaneous chronic graft versus host disease. Photodermatol Photoimmunol Photomed 2002;18:183-90.
[Google Scholar]
|
| 43. |
Bonanomi S, Balduzzi A, Tagliabue A, Biagi E, Rovelli A, Corti P, et al. Bath PUVA therapy in pediatric patients with drug-resistant cutaneous graft-versus-host disease. Bone Marrow Transplant 2001;28:631-2.
[Google Scholar]
|
| 44. |
Volkenandt M, Kerscher M, Sander C, Meurer M, Rocken M. PUVA-bath photochemotherapy resulting in rapid clearance of lymphomatoid papulosis in a child. Arch Dermatol 1995;131:1094.
[Google Scholar]
|
| 45. |
Schiener R, Behrens-Williams SC, Gottlöber P, Pillekamp H, Peter RU, Kerscher M. Eosinophilic fasciitis treated with psoralen-ultraviolet A bath photochemotherapy. Br J Dermatol 2000;142:804-7.
[Google Scholar]
|
| 46. |
Kunte C, Kerschenlohr K, Röcken M, Schirren C. Keratosis lichenoides chronica: Treatment with bath-PUVA. Acta Derm Venereol 2007;87:182-3.
[Google Scholar]
|
| 47. |
Behrens S, Reuther T, Gruss C, Auer T, Altmeyer P, Kerscher M. Disseminated pagetoid reticulosis: Response to bath PUVA. Br J Dermatol 1998;139:343-4.
[Google Scholar]
|
| 48. |
Szegedi A, Bégány A, Hunyadi J. Successful treatment of generalized granuloma annulare with polyethylene sheet bath PUVA. Acta Derm Venereol 1999;79:84-5.
[Google Scholar]
|
| 49. |
Batchelor R, Clark S. Clearance of generalized papular umbilicated granuloma annulare in a child with bath PUVA therapy. Pediatr Dermatol 2006;23:72-4.
[Google Scholar]
|
| 50. |
Grimmer J, Weiss T, Weber L, Meixner D, Scharffetter-Kochanek K. Successful treatment of lichen amyloidosis with combined bath PUVA photochemotherapy and oral acitretin. Clin Exp Dermatol 2007;32:39-42.
[Google Scholar]
|
| 51. |
Yüksek J, Sezer E, Köseoglu D, Markoç F, Yildiz H. Scleredema treated with broad-band ultraviolet A phototherapy plus colchicine. Photodermatol Photoimmunol Photomed 2010;26:257-60.
[Google Scholar]
|
| 52. |
Hager CM, Sobhi HA, Hunzelmann N, Wickenhauser C, Scharenberg R, Krieg T, et al. Bath-PUVA therapy in three patients with scleredema adultorum. J Am Acad Dermatol 1998;38(2 Pt 1):240-2.
[Google Scholar]
|
| 53. |
Smith RA, Ross JS, Staughton RC. Bath PUVA as a treatment for aquagenic pruritus. Br J Dermatol 1994;131:584.
[Google Scholar]
|
| 54. |
Mai DW, Omohundro C, Dijkstra JW, Bailin PL. Childhood vitiligo successfully treated with bath PUVA. Pediatr Dermatol 1998;15:53-5.
[Google Scholar]
|
| 55. |
Pai S, Srinivas CR. Bathing suit delivery of 8-methoxypsoralen for psoriasis: A double-blind, placebo-controlled study. Int J Dermatol 1994;33:576-8.
[Google Scholar]
|
| 56. |
Hofer A, Fink-Puches R, Kerl H, Quehenberger F, Wolf P. Paired comparison of bathwater versus oral delivery of 8-methoxypsoralen in psoralen plus ultraviolet: A therapy for chronic palmoplantar psoriasis. Photodermatol Photoimmunol Photomed 2006;22:1-5.
[Google Scholar]
|
| 57. |
Schiener R, Gottlöber P, Müller B, Williams S, Pillekamp H, Peter RU, et al. PUVA-gel vs. PUVA-bath therapy for severe recalcitrant palmoplantar dermatoses. A randomized, single-blinded prospective study. Photodermatol Photoimmunol Photomed 2005;21:62-7.
[Google Scholar]
|
| 58. |
Bretterklieber A, Legat FJ, Wolf P, Hofer A. Retrospective long-term follow-up in patients with chronic palmoplantar dermatoses after good response to bath PUVA therapy. J Dtsch Dermatol Ges 2012;10:814-8.
[Google Scholar]
|
| 59. |
Coleman WR, Lowe NJ, David M, Halder RM. Palmoplantar psoriasis: Experience with 8-methoxypsoralen soaks plus ultraviolet A with the use of a high-output metal halide device. J Am Acad Dermatol 1989;20:1078-82.
[Google Scholar]
|
| 60. |
Behrens S, von Kobyletzki G, Gruss C, Reuther T, Altmeyer P, Kerscher M. PUVA-bath photochemotherapy (PUVA-soak therapy) of recalcitrant dermatoses of the palms and soles. Photodermatol Photoimmunol Photomed 1999;15:47-51.
[Google Scholar]
|
| 61. |
Tupker RA, Coenraads PJ, Zanen P, Schuttelaar ML. Randomized controlled observer-blinded treatment of chronic foot eczema with iontophoresis and bath-PUVA. Acta Derm Venereol 2013;93:456-60.
[Google Scholar]
|
| 62. |
van Coevorden AM, Kamphof WG, van Sonderen E, Bruynzeel DP, Coenraads PJ. Comparison of oral psoralen-UV-A with a portable tanning unit at home vs hospital-administered bath psoralen-UV-A in patients with chronic hand eczema: An open-label randomized controlled trial of efficacy. Arch Dermatol 2004;140:1463-6.
[Google Scholar]
|
| 63. |
Tzaneva S, Kittler H, Thallinger C, Hönigsmann H, Tanew A. Oral vs. bath PUVA using 8-methoxypsoralen for chronic palmoplantar eczema. Photodermatol Photoimmunol Photomed 2009;25:101-5.
[Google Scholar]
|
| 64. |
Schempp CM, Müller H, Czech W, Schöpf E, Simon JC. Treatment of chronic palmoplantar eczema with local bath-PUVA therapy. J Am Acad Dermatol 1997;36(5 Pt 1):733-7.
[Google Scholar]
|
| 65. |
Lassus A, Lauharanta J, Eskelinen A. The effect of etretinate compared with different regimens of PUVA in the treatment of persistent palmoplantar pustulosis. Br J Dermatol 1985;112:455-9.
[Google Scholar]
|
| 66. |
Matsunami E, Takashima A, Mizuno N, Jinno T, Ito H. Topical PUVA, etretinate, and combined PUVA and etretinate for palmoplantar pustulosis: Comparison of therapeutic efficacy and the influences of tonsillar and dental focal infections. J Dermatol 1990;17:92-6.
[Google Scholar]
|
| 67. |
Errichetti E, Piccirillo A, Ricciuti F, Ricciuti F. Steroid-resistant localized lymphomatoid papulosis treated with local bath-PUVA therapy. Indian J Dermatol 2013;58:163.
[Google Scholar]
|
| 68. |
Halkier-Sørensen L, Cramers M, Kragballe K. Twenty-nail dystrophy treated with topical PUVA. Acta Derm Venereol 1990;70:510-1.
[Google Scholar]
|
| 69. |
Kaskel P, Leiter U, Krähn G, Schiener R, Pillekamp H, Peter RU, et al. PUVA-bath photochemotherapy for congenital palmoplantar keratoderma in an 11-year-old girl. Br J Dermatol 2000;143:464-5.
[Google Scholar]
|
| 70. |
Tekin NS, Tekin IO, Cinar S, Altinyazar HC, Koca R, Esturk E. The PUVA-turban as an alternative treatment of alopecia associated with chronic graft versus host disease. J Am Acad Dermatol 2005;53:902-3.
[Google Scholar]
|
| 71. |
Calzavara-Pinton PG, Ortel B, Carlino AM, Honigsmann H, De Panfilis G. Phototesting and phototoxic side effects in bath PUVA. J Am Acad Dermatol 1993;28:657-9.
[Google Scholar]
|
| 72. |
Koulu LM, Jansén CT. Skin phototoxicity variations during repeated bath PUVA exposures to 8-methoxypsoralen and trimethylpsoralen. Clin Exp Dermatol 1984;9:64-9.
[Google Scholar]
|
| 73. |
Takashima A, Yamamoto K, Kimura S, Takakuwa Y, Mizuno N. Allergic contact and photocontact dermatitis due to psoralens in patients with psoriasis treated with topical PUVA. Br J Dermatol 1991;124:37-42.
[Google Scholar]
|
| 74. |
Halpern SM, Anstey AV, Dawe RS, Diffey BL, Farr PM, Ferguson J, et al. Guidelines for topical PUVA: A report of a workshop of the British photodermatology group. Br J Dermatol 2000;142:22-31.
[Google Scholar]
|
| 75. |
Hannuksela-Svahn A, Sigurgeirsson B, Pukkala E, Lindelöf B, Berne B, Hannuksela M, et al. Trioxsalen bath PUVA did not increase the risk of squamous cell skin carcinoma and cutaneous malignant melanoma in a joint analysis of 944 Swedish and Finnish patients with psoriasis. Br J Dermatol 1999;141:497-501.
[Google Scholar]
|
| 76. |
Gómez MI, Azaña JM, Arranz I, Harto A, Ledo A. Plasma levels of 8-methoxypsoralen after bath-PUVA for psoriasis: Relationship to disease severity. Br J Dermatol 1995;133:37-40.
[Google Scholar]
|
| 77. |
Neumann NJ, Ruzicka T, Lehmann P, Kerscher M. Rapid decrease of phototoxicity after PUVA bath therapy with 8-methoxypsoralen. Arch Dermatol 1996;132:1394.
[Google Scholar]
|
| 78. |
Menter A, Korman NJ, Elmets CA, Feldman SR, Gelfand JM, Gordon KB, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 5. Guidelines of care for the treatment of psoriasis with phototherapy and photochemotherapy. J Am Acad Dermatol 2010;62:114-35.
[Google Scholar]
|
Fulltext Views
15,751
PDF downloads
3,388





