Translate this page into:
Crusted scabies diagnosed by reflectance confocal microscopy
2 Istanbul Training and Research Hospital, Department of Dermatology, Istanbul, Turkey
Correspondence Address:
Pinar Incel Uysal
Ankara Numune Training And Research Hospital, Dermatology Department, Anafartalar Mh, Talatpasa Bulvari, No: 5, Altindag, Ankara
Turkey
| How to cite this article: Uysal PI, Gurel MS, Erdemir AV. Crusted scabies diagnosed by reflectance confocal microscopy. Indian J Dermatol Venereol Leprol 2015;81:620-622 |
Sir,
A 44-year-old man was admitted with asymptomatic multiple, erythematous, tiny papules and hyperkeratotic and psoriasiform plaques [Figure - 1]a. The lesions had been slowly extending over a 1 year period. The patient, who had been living alone for 2 years did not have any other medical problem. There was no family history of inflammatory dermatoses or genodermatoses. Examination revealed multiple, tiny, erythematous papules mainly on the trunk, inguinal folds, over the gluteal region and a few on upper and lower extremities. Lichenoid papules were seen on the dorsum of hands [Figure - 1]b. General physical examination including cardiovascular, respiratory, genitourinary and lymphatic system revealed no abnormalities. Laboratory results demonstrated that the patient was hepatitis B surface antigen (HBsAg), hepatitis Be antigen (HBeAg) and hepatitis Be antibody (anti-HBeAg) positive and hepatitis B core antibody IgM (anti-HBc IgM) negative. Serum hepatitis B virus (HBV) DNA was 115,000 copies/mL. Hepatitis C virus (HCV) RNA and human immunodeficiency virus (HIV) RNA tests were negative. Other laboratory tests (complete blood count, glucose, blood urea nitrogen, serum creatinine, total bilirubin, albumin, liver function tests, sodium, potassium and urinalysis) were normal except elevated IgE (395 IU/mL). X-ray of the chest and ultrasonography of the abdomen were also normal. Clinically, we considered an initial diagnosis of lichenoid eruption or generalized eruptive lichen planus. Biopsies from lichenoid papules on his back and dorsum of hand revealed hyperkeratosis, parakeratosis, acanthosis, dermal mononuclear inflammatory infiltrates, and dilated dermal vessels, consistent with lichen simplex chronicus [Figure - 2].
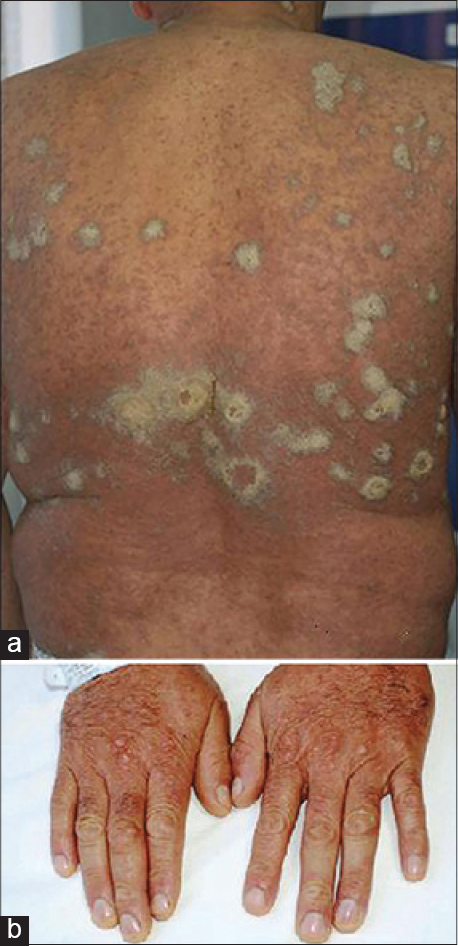 |
| Figure 1: (a) Extensive, multiple, tiny erythematous papules and plaques with hyperkeratosis (b) Lichenoid papules on the dorsa of hands |
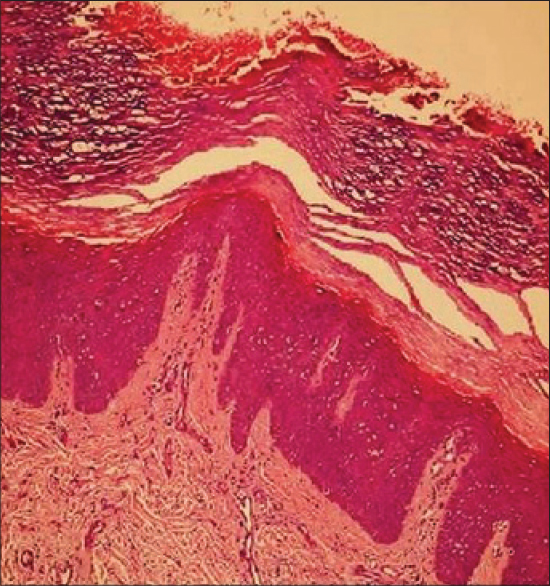 |
| Figure 2: Hyperkeratosis, parakeratosis, acanthosis, infiltration of dermis with mononuclear cells and dilated dermal blood vessels (H and E, ×100) |
We treated the patient with methylprednisolone, 40 mg daily and cyclosporine, 300 mg daily. In addition, he received lamivudine, 100 mg daily for active hepatitis B. After 2 weeks of treatment, the patient did not show any significant clinical improvement and additionally developed new psoriasiform plaques and sterile pustules [Figure - 3]a and [Figure - 3]b.
 |
| Figure 3: (a) New onset psoriasiform plaques and (b) pustules while on therapy |
Due to the discrepancy between clinical presentation, progression and histopathology, the lesions were examined by reflectance confocal microscopy (RCM; Vivascope 3000, Lucid Inc., Henrietta, NY, USA). Each given image corresponds to a horizontal skin section of 0.5 × 0.5 mm (0.25 mm2) at a selected depth. Stack images were captured from the top of the stratum corneum to the upper dermis with steps of 3–5 µm thickness. With the aim of minimizing light scattering, hyperkeratotic squames were removed. Increased thickening of the stratum corneum of >40 µm was remarkable on images taken from the skin of the patient's back. On confocal images, multiple tortuous large segments representing burrows were noted in the stratum corneum and at the end of the burrows, mites were clearly identified [Figure - 4]. These burrows contained roundish, refractile, oval particles corresponding to eggs and mite feces. Additionally, highly refractile round to polygonal structures were seen consistent with parakeratosis. There were no other abnormalities. Once the diagnosis of crusted scabies was confirmed by reflectance confocal microscopy, immunosuppressive therapy was stopped at day 15. Additional laboratory tests (blood smear, complement C3 and C4, immunoglobulin (A, G, M) levels and T cell subset analyses) performed to investigate for an underlying immune deficiency were within normal limits.
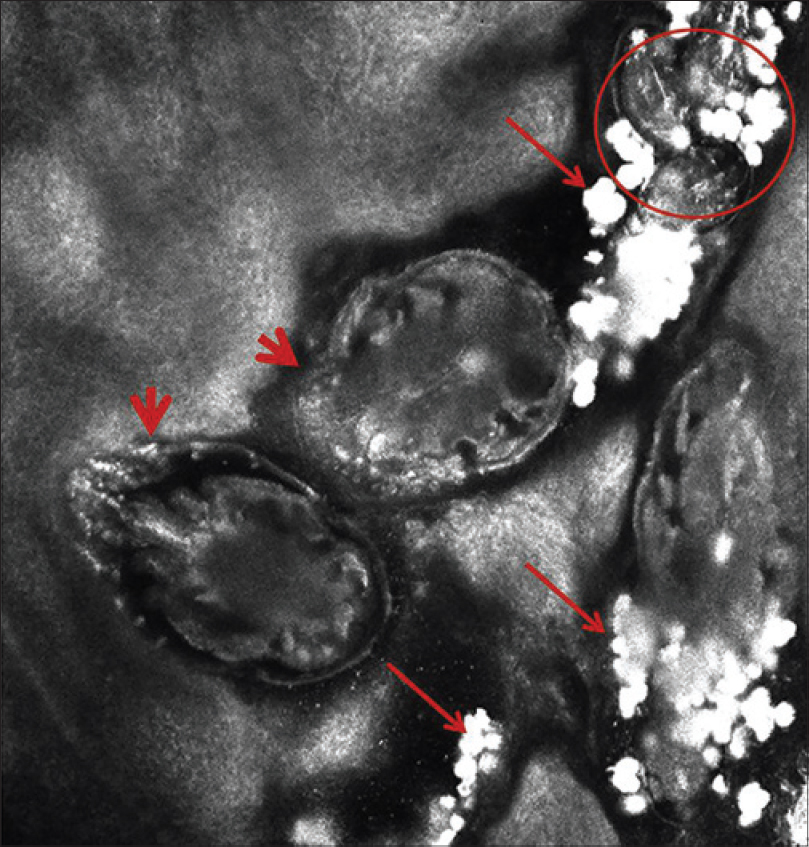 |
| Figure 4: A curled linear burrow filled with mites (thick arrows), eggs and developing mites (circle) and abundant feces (thin arrows) |
The patient was treated with ivermectin, 0.2 mg/kg/week (12 mg/week) for 4 weeks and a keratolytic cream till complete clearance. The patient showed partial recovery at week 4 [Figure - 5] and recovered completely at week 10.
 |
| Figure 5: Improvement of lesions at week 4 following ivermectin therapy |
Crusted scabies is a distinct clinical subtype of scabies associated with immunosuppressed states due to topical or systemic glucocorticoid therapy, human immunodeficiency virus infection, human T lymphotropic virus 1 infection, T-cell lymphoma and leukemia or following organ transplant patients, and has also been noted in physically or mentally handicapped, senile bedridden patients.[1],[2],[3],[4],[5] It has also been associated with previously treated leprosy, substance abuse, systemic lupus erythematosus, pulmonary tuberculosis, diabetes mellitus and hepatitis B.[6] Crusted scabies may be misdiagnosed because of its unusual presentations. Clinical manifestations of crusted scabies could be misdiagnosed as psoriasis, hyperkeratotic eczema, contact dermatitis, cutaneous lymphoma, Darier's disease or lichenoid dermatosis as in our case. Recent evidence indicates that crusted scabies develops typically as a result of a Th1/Th2 imbalance, with a cytotoxic T cell type 2 response in the skin, high levels of antibody in the blood and uncontrolled growth of the parasite. In our case, the patient's physical examination, immunoglobulin levels (IgG, IgM, IgA) and T cell subset analyses were normal and HIV tests were negative. Furthermore, there was no peripheral or tissue eosinophilia. However, he was found to have active hepatitis B which may have led to immunologic dysregulation, deficient eosinophilic response and as a result, crusted scabies.
Reflectance confocal microscopy is a non-invasive technique that uses a diode laser as a source of light and allows diagnosis of melanocytic and non-melanocytic skin tumors and inflammatory skin disease using a real-time digital imaging system. It offers a unique tool to study dynamic changes of skin disease, in vivo and has been previously reported by some workers to be useful in the detection and quantification of Sarcoptes scabiei.[7],[8],[9],[10]
Although the gold standard for visualizing scabies ex vivo is microscopic examination, reflectance confocal microscopy has the potential to provide an easy and quick diagnosis in vivo, which may be particularly useful in atypical cases.
| 1. |
Hulbert TV, Larsen RA. Hyperkeratotic (Norwegian) scabies with gram-negative bacteremia as the initial presentation of AIDS. Clin Infect Dis 1992;14:1164-5.
[Google Scholar]
|
| 2. |
Mollison LC, Lo ST, Marning G. HTLV-I and scabies in Australian aborigines. Lancet 1993;341:1281-2.
[Google Scholar]
|
| 3. |
Roberts LJ, Huffam SE, Walton SF, Currie BJ. Crusted scabies: Clinical and immunological findings in seventy-eight patients and a review of the literature. J Infect 2005;50:375-81.
[Google Scholar]
|
| 4. |
Suzumiya J, Sumiyoshi A, Kuroki Y, Inoue S. Crusted (Norwegian) scabies with adult T-cell leukemia. Arch Dermatol 1985;121:903-4.
[Google Scholar]
|
| 5. |
Cakmak SK, Gonul M, Gul U, Unal T, Daglar E. Norwegian scabies in a renal transplant patient. Australas J Dermatol 2008;49:248-9.
[Google Scholar]
|
| 6. |
Roberts LJ, Huffam SE, Walton SF, Currie BJ. Crusted scabies: Clinical and immunological findings in seventy-eight patients and a review of the literature. The Journal of infection. 2005;50:375-81
[Google Scholar]
|
| 7. |
Longo C, Bassoli S, Monari P, Seidenari S, Pellacani G. Reflectance-mode confocal microscopy for the in vivo detection of Sarcoptes scabiei. Arch Dermatol 2005;141:1336.
[Google Scholar]
|
| 8. |
Turan E, Erdemir AT, Gurel MS, Basaran YK. The detection of Sarcoptes scabiei in human skin by in vivo confocal microscopy. Eur J Dermatol 2011;21:1004-5.
[Google Scholar]
|
| 9. |
Levi A, Mumcuoglu KY, Ingber A, Enk CD. Assessment of Sarcoptes scabiei viability in vivo by reflectance confocal microscopy. Lasers Med Sci 2011;26:291-2.
[Google Scholar]
|
| 10. |
Cinotti E, Perrot JL, Labeille B, Vercherin P, Chol C, Besson E, et al. Reflectance confocal microscopy for quantification of Sarcoptes scabiei in Norwegian scabies. J Eur Acad Dermatol Venereol 2013;27:e176-8.
[Google Scholar]
|
Fulltext Views
4,932
PDF downloads
1,690





