Translate this page into:
Keratosis follicularis spinulosa decalvans showing excellent response to isotretinoin
2 Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
3 Department of Otorhinolaryngology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
Correspondence Address:
Rashmi Kumari
Assistant Professor, Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry - 605 006
India
| How to cite this article: Gupta D, Kumari R, Bahunutula RK, Thappa DM, Toi PC, Parida PK. Keratosis follicularis spinulosa decalvans showing excellent response to isotretinoin. Indian J Dermatol Venereol Leprol 2015;81:646-648 |
Sir,
Keratosis follicularis spinulosa decalvans is a rare genodermatosis and we were able to find less than fifty previous reports of the condition. We describe two such cases in a family, a mother and her daughter who had ethmoidal and lacrimal sac mucocoeles as well.
A 7-year-old girl, born of a non-consanguineous marriage, presented with multiple follicular lesions over the face and trunk with patchy hair loss over the scalp, eyebrows and eyelashes since the age of three. She also suffered from persistent rhinorrhoea and epiphora from the left eye. There was no photophobia, hearing loss or decreased sweating. She was earlier diagnosed and treated for atopic dermatitis and blepharitis.
Cutaneous examination revealed keratosis pilaris [Figure - 1]a along with scarring alopecia over the vertex [Figure - 1]c and partial loss of eyebrows and eyelashes [Figure - 1]d. The nails, mucosa, palms and soles were unaffected. Oral examination revealed dental caries in all the deciduous molar teeth. Her lower incisors were tapering in shape with gaps between them (diastema). Dermoscopy revealed normal hair shafts with follicular effacement [Figure - 2]a. Histopathology showed hyperkeratosis, acanthosis, follicular plugging, perifollicular inflammatory infiltrate composed predominantly of lymphocytes and mild dermal fibrosis [Figure - 2]b. There was no basal vacuolar change and direct immunofluorescence was negative. Ophthalmological examination revealed telecanthus with regurgitation of mucopurulent discharge through the lacrimal sac punctii. A 99mTc-pertechnetate dacryoscintigraphy revealed proximal left nasolacrimal duct obstruction. A CT scan showed left lacrimal sac and ethmoidal mucocoeles [Figure - 2]c and [Figure - 2]d.
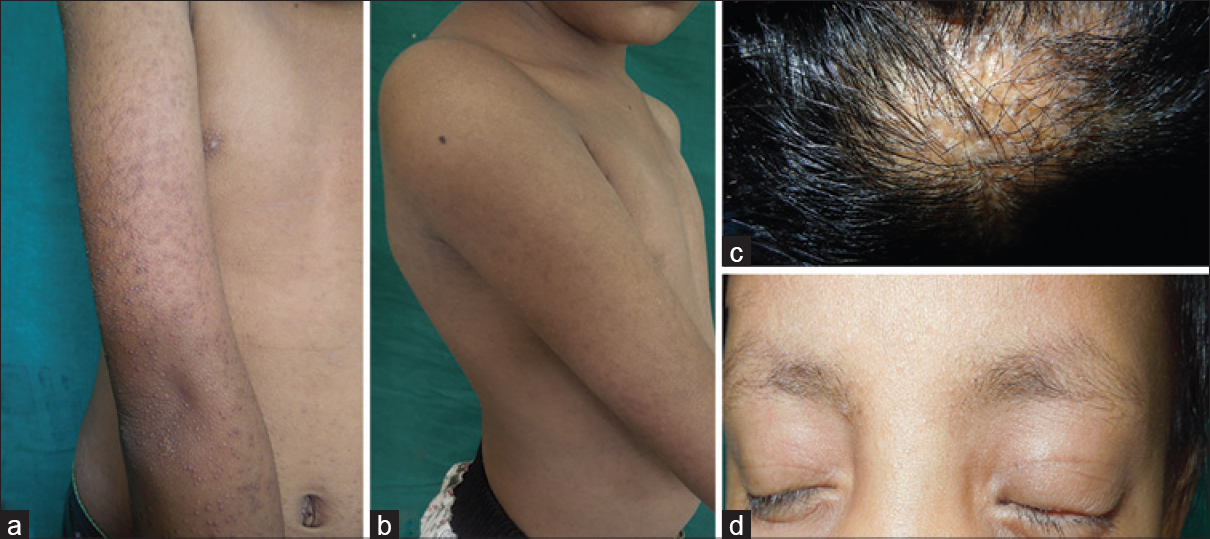 |
| Figure 1: (a) Keratosis pilaris over the extensor aspect of right upper limb. (b) Resolution of keratosis pilaris after 10 months of isotretinoin. (c) Follicular papules with scarring alopecia over the scalp. (d) Thinning of eyebrows and partial loss of eyelashes |
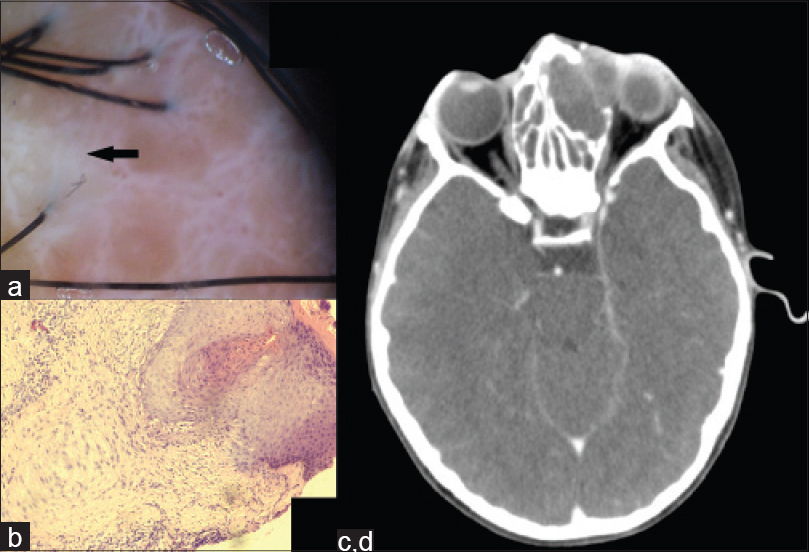 |
| Figure 2: (a) Areas of scarring as seen on dermoscopy. (b) Follicular hyperkeratosis, acanthosis with follicular plugging, fibrous stelae and surrounding mononuclear infiltrate (Hematoxylin and Eosin, ×400). (c and d) CT scan showing (c) lacrimal mucocoele and (d) ethmoidal mucocoele |
The girl's 35-year-old mother had similar complaints including allergic rhinitis since the age of six. Cutaneous examination revealed keratosis pilaris with extensive cicatricial alopecia involving almost the entire scalp [Figure - 3]a. She had dystrophy of both the great toenails[Figure - 3]b. Oral examination revealed extensive dental caries. Microscopic examination and cultures from the nail were negative for fungi. The males in the family were unaffected.
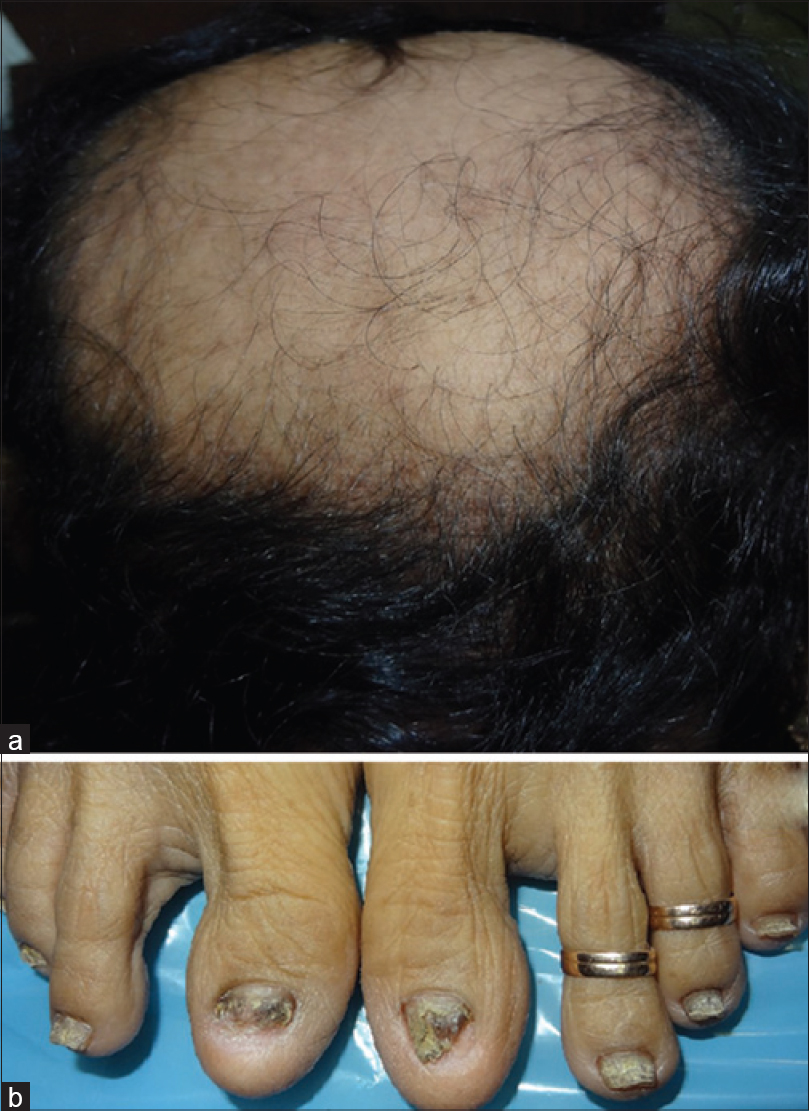 |
| Figure 3: (a) Extensive scarring alopecia in the mother. (b) Dystrophy of both the great toe nails |
A diagnosis of keratosis follicularis spinulosa decalvans was made and the child was started on isotretinoin (0.5 mg/kg/day). She underwent ethmoidectomy and excision of the mucocoeles. There was regression of the keratotic papules within four weeks. Further hair loss and scarring also had stopped. There was no relapse at one year of follow up [Figure - 1]b. The mother did not want any treatment as she had already developed scarring alopecia over 80% of the scalp and used to cover it under a scarf.
Keratosis follicularis spinulosa decalvans was first described by Siemens in 1926. It begins in early childhood. A progressive cicatricial alopecia of the scalp, eyebrows and eyelashes starts in late childhood and remits by adolescence. Ocular abnormalities include photophobia, corneal opacities and blepharitis. Oral manifestations include absent or conoid teeth, dental caries and enamel hypoplasia. Thickened dystrophic nails and high cuticles have been described.[1],[2],[3] Histopathology shows hyperkeratosis and hypergranulosis at the infundibulum and isthmus of the hair follicle, with surrounding polymorphonuclear leukocytes. This is followed by sparse mononuclear cell infiltrate, collagen deposition and follicular destruction.[4]
This condition occurs due to a missense mutation in the MBTPS2 (membrane-bound transcription factor peptidase site 2) gene, which leads to disturbed epidermal differentiation due to inhibition of cholesterol biosynthesis. The adverse impact on epidermal lipid composition results in disturbed barrier function. This leads to increased transepidermal water loss, disturbed cytokine production, epidermal hyperplasia, hyperkeratosis and inflammation, akin to many inherited ichthyoses. This may explain the efficacy of isotretinoin in this disorder. This disorder has an X-linked mode of inheritance and severe clinical manifestations involving only females as in our case may be explained by Lyonization.[2]
Evidence for treatment of keratosis follicularis spinulosa decalvans is anecdotal. Topical keratolytic agents and emollients offer only symptomatic improvement. Antibiotics may be necessary during pustular flares of disease.[4] Oral retinoids are effective in the early phase of disease when active perifollicular infiltrate is present. It must be continued for 6 to 12 months for an optimum response. Retinoids decrease epidermal proliferation and cytokine production thereby reducing hyperkeratosis and inflammation.[5]
Ethmoidal and lacrimal sac mucocoeles may have been a coincidental finding. Atopy and persistent rhinorrhoea may have resulted in mucus secretion which could have blocked the sinus ostium and formed a cyst-like expansile lesion. Unique features about this family include mother to daughter transmission, presence of nail and dental findings, lack of photophobia and no clinical involvement in male members of the family. This condition is uncommon in Asians, and we were able to find only 4 previous reports from India.
| 1. |
van Osch LD, Oranje AP, Keukens FM, Voorst Vader van PC, Veldman E. Keratosis follicularis spinulosa decalvans: A family study of seven male cases and six female carriers. J Med Genet 1992;29:36-40.
[Google Scholar]
|
| 2. |
Fong K, Wedgeworth EK, Lai-Cheong JE, Tosi I, Mellerio JE, Powell AM, et al. MBTPS2 mutation in a British pedigree with keratosis follicularis spinulosa decalvans. Clin Exp Dermatol 2012;37:631-4.
[Google Scholar]
|
| 3. |
Castori M, Covaciu C, Paradisi M, Zambruno G. Clinical and genetic heterogeneity in keratosis follicularis spinulosa decalvans. Eur J Med Genet 2009;52:53-8.
[Google Scholar]
|
| 4. |
Baden HP, Byers HR. Clinical findings, cutaneous pathology, and response to therapy in 21 patients with keratosis pilaris atrophicans. Arch Dermatol 1994;130:469-75.
[Google Scholar]
|
| 5. |
Richard G, Harth W. Keratosis follicularis spinulosa decalvans. Therapy with isotretinoin and etretinate in the inflammatory stage. Hautarzt 1993;44:529-34.
[Google Scholar]
|
Fulltext Views
3,923
PDF downloads
1,132





