Translate this page into:
Revisiting cutaneous metastasis from carcinoma gall bladder
2 Department of Pathology, Cancer Institute, Amrita Institute of Medical Sciences, Ponekkara, AIMS P.O., Kochi, Kerala, India
Correspondence Address:
Wesley M Jose
Department of Medical Oncology, Cancer Institute, Amrita Institute of Medical Sciences, Ponekkara, AIMS P.O., Kochi - 682 041, Kerala
India
| How to cite this article: Jose WM, Boyella PK, Nair IR, Eapen M, Keechilat P. Revisiting cutaneous metastasis from carcinoma gall bladder. Indian J Dermatol Venereol Leprol 2014;80:82-85 |
Sir,
Gall bladder carcinoma is the most aggressive tumor with poorest prognosis among all hepato-biliary cancers. [1] Gall bladder malignancy is common in north and central India with a strong female predilection. [2] Estimated female to male ratio of gall bladder carcinoma incidence in northern India is 10.1:1.01/100,000. [3] However, incidence is one-tenth in Southern India compared with north (0.0-0.7/100,000 women). Gall bladder malignancy in spite of being common in Indian subcontinent is still diagnosed at an advanced stage. The diagnosis evades common differentials especially when presenting in unusual ways. Skin is a site of both primary and metastatic malignancy. Metastasis to skin from internal malignancies is rare and portends a poor prognosis. Skin is commonly involved in metastasis from carcinoma breast, lung, colon and kidneys. Furthermore, skin metastasis from gall bladder is extremely uncommon with only few reports in the world literature. The common site for gall bladder to metastasize is the liver and draining lymph nodes.
A 76-year-old lady presented with 2-3 months history of multiple non-pruritic, painless subcutaneous lesions on exposed areas of the face and upper trunk, not improving with routine measures prescribed by her personal physician. She had unquantified weight loss but no history of fever, night sweats or pruritus. Clinical examination revealed multiple 4-7 mm erythematous discrete papular lesions with no surrounding induration over her face, neck and trunk. There were no palpable nodes. There was mild fullness in the right hypochondrium. No mass was palpable.
She had normal hematocrit, mildly elevated aspartate transaminase (65.4 IU/L); alanine transaminase (133.6 IU/L) and alkaline phosphatase (211.8 IU/L). An excision biopsy from a skin lesion revealed subcutaneous tissue infiltration by neoplastic cells arranged singly. The cells were medium sized, with moderate cytoplasm and pleomorphic vesicular nuclei, some with prominent nucleoli. Numerous admixed lymphocytes, plasma cells and neutrophils were seen. Many apoptotic bodies were also noted [H and E, stain, [Figure - 1]. Features were of a poorly differentiated neoplasm. On immunohistochemical analysis, cells were positive for pan cytokeratin (CK), CK7 [Figure - 2], focally for carcinoembryonic antigen (CEA) [Figure - 3] and negative for leucocyte common antigen, thyroid transcription factor, CK20, CD30 and anaplastic lymphoma kinase. Ki 67 (mitotic index) was 50% in the large cells. Immunohistochemistry was suggestive of a metastatic adenocarcinoma possibly from the stomach, pancreatico-biliary tract or breast.
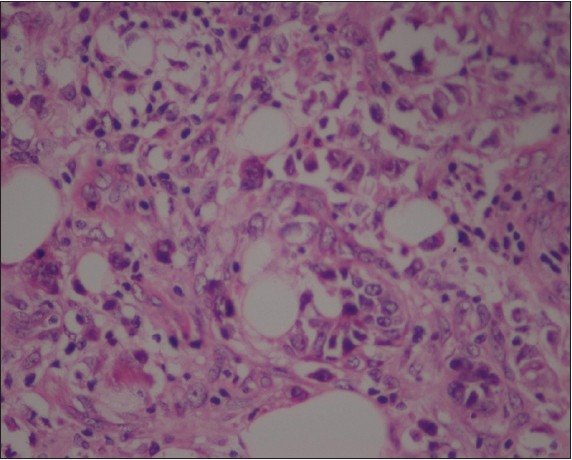 |
| Figure 1: Subcutaneous nodules - H and E |
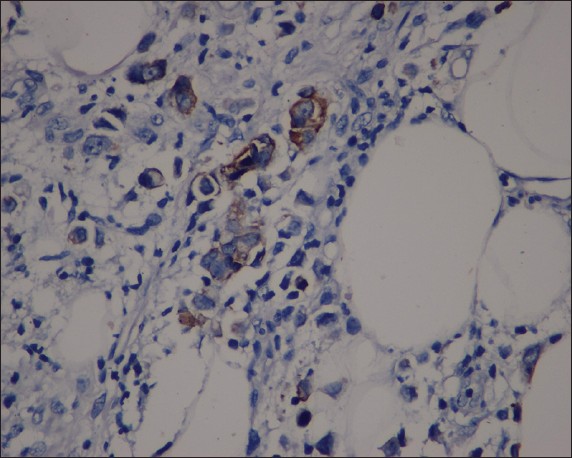 |
| Figure 2: Subcutaneous nodules - cytokeratin 7 |
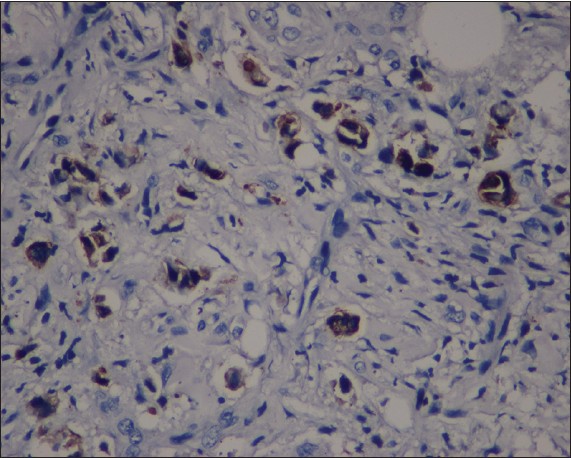 |
| Figure 3: Subcutaneous nodules - carcinoembryonic antigen |
A computed tomography scan of the abdomen [Figure - 4] revealed a minimally enhancing hypodense lesion in the gall bladder measuring 2.8 cm × 2.6 cm, infiltrating into segment IV of liver and subsegmental right hepatic ducts causing moderate intrahepatic biliary radical dilatation in both lobes. Multiple lymph nodes were seen in porta hepatis and along celiac axis causing mass effect. A hypodense lesion was seen in segment VII measuring 1.4 cm × 1.3 cm. An ultrasound guided biopsy from liver and gall bladder lesion revealed a poorly differentiated carcinoma with the same immunohistochemical pattern as the cutaneous neoplasm.
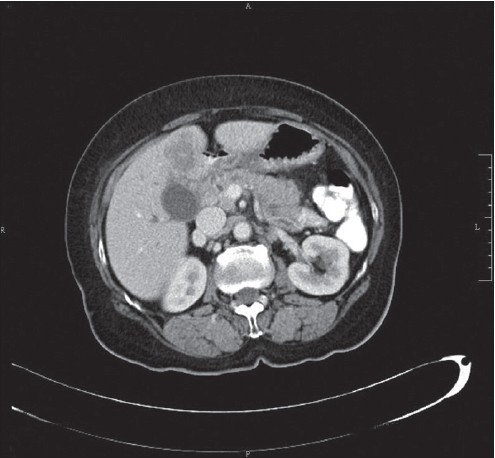 |
| Figure 4: Computed tomography scan with gall bladder mass |
Her CA 19-9 was 50251 U/ml, serum CEA 12.55 ng/ml and alpha fetoprotein 47.11 ng/ml. She was administered palliative chemotherapy (gemcitabine/carboplatin), which produced complete resolution of skin lesions and 70% reduction in target lesion (Response Evaluation Criteria in Solid Tumors criteria). Her CA 19-9 dropped to 2765.8 U/ml. Post fifth cycle of treatment she had severe fatigue and further treatment was discontinued. A few weeks later her CA 19-9 began to rise and her general condition deteriorated rapidly. She succumbed to her illness 3 months later (7.5 months from the day of diagnosis).
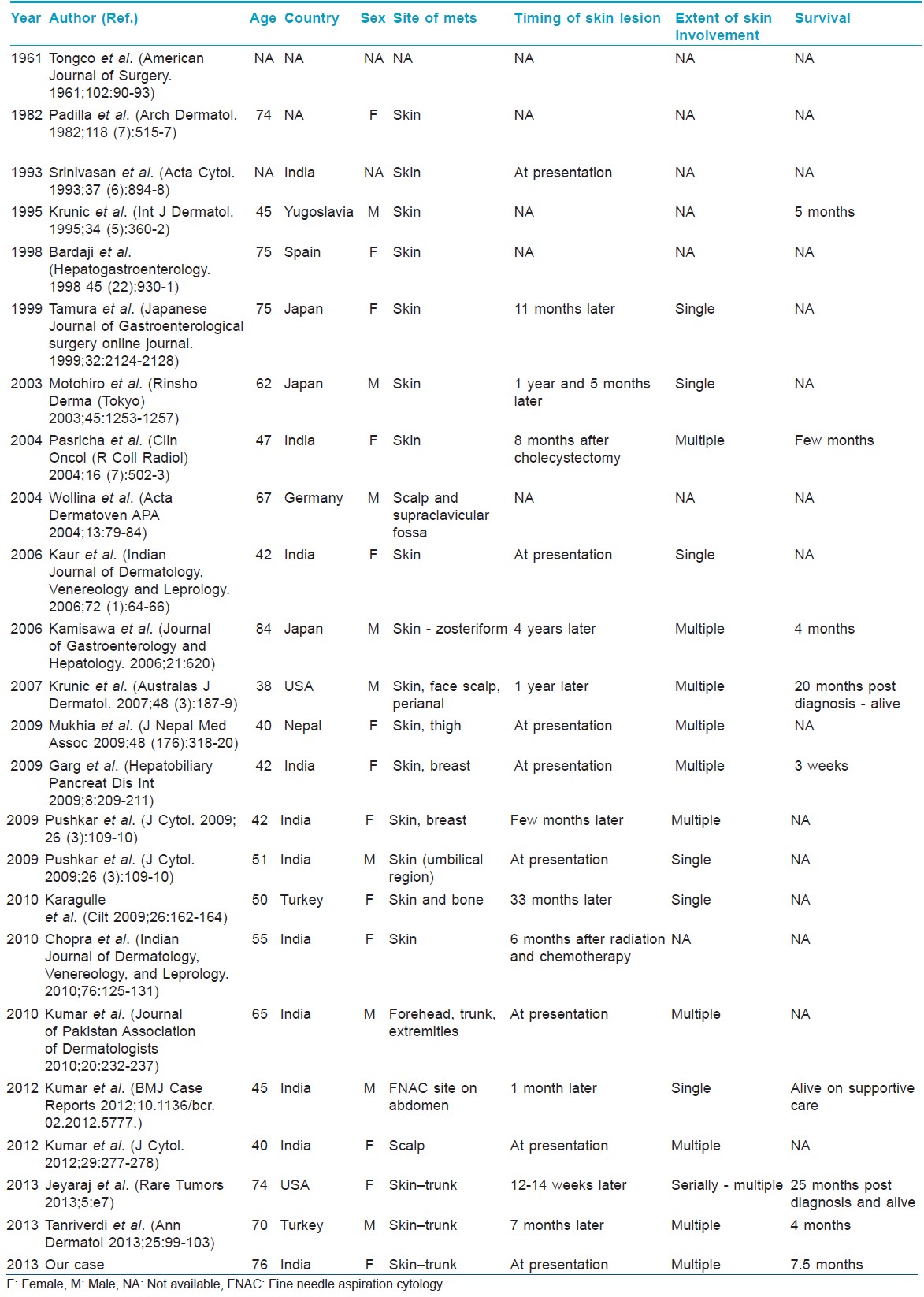
In a large retrospective analysis from Veteran Administration Hospital (USA), only 77 (0.07%) of 100,453 cases reviewed, were reported to have cutaneous metastasis with average survival of 7.5 months. [4] This sort of rarity leads to misdiagnosis of skin lesions, more so when skin metastasis pre- or post-dates the malignancy. Review of the literature revealed 23 case reports of gall bladder carcinoma metastasizing to skin [Table - 1]. Majority of the reported cases are from Northern India. More than 50% are females with the median age of 53 years. Among reported Indian patients 70% are females and the median age was lower at 46 years. Most of the reported patients presented to the physician with skin lesions as their primary symptom. Cases with umbilical metastasis (Sister Mary Joseph nodule) alone were excluded as we believe that the mechanism is different. The generalized dermatological metastasis is likely due to hematogenous spread, however in umbilical metastasis direct, hematogenous and lymphatic spread occurs. The skin metastasis generally occurs on the chest and abdomen and is rare in the extremities, neck, back and scalp. [5] Single metastatic lesions can closely simulate a benign cyst, keratoacanthoma, basal cell carcinoma or melanoma. The other differentials may include pyogenic granuloma, granular cell tumor, a benign subcutaneous nodule and cutaneous angiosarcoma. Certain metastatic tumors may closely simulate skin primary tumors, including metastatic small cell carcinoma as Merkel cell carcinoma, metastatic systemic sarcoma as primary skin sarcoma, papillary thyroid carcinoma as primary papillary adnexal tumors, clear cell renal cell carcinoma as either sebaceous carcinoma or clear cell hidradenoma and metastatic mucinous carcinoma as primary cutaneous mucinous carcinoma. Nodular metastatic lesions are easily and often misdiagnosed as simple cysts or benign connective tissue lesions. Therefore, atypical or persistent nodular lesions in patients with a history of systemic malignancy should be considered for biopsy to rule out metastasis. [6]
The intent of treatment in a patient with a Stage IV carcinoma gall bladder is palliative; however, the treatment (chemotherapy or best supportive care) for symptom control would definitely provide the patient a better quality-of-life if the diagnosis is made early.
| 1. |
Zhu AX, Hong TS, Hezel AF, Kooby DA. Current management of gallbladder carcinoma. Oncologist 2010;15:168-81.
[Google Scholar]
|
| 2. |
Kapoor VK, McMichael AJ. Gallbladder cancer: An 'Indian' disease. Natl Med J India 2003;16:209-13.
[Google Scholar]
|
| 3. |
Indian Council of Medical Research (ICMR). Annual report of population-based cancer registries of the national cancer registry program. 1996.
[Google Scholar]
|
| 4. |
Saeed S, Keehn CA, Morgan MB. Cutaneous metastasis: A clinical, pathological, and immunohistochemical appraisal. J Cutan Pathol 2004;31:419-30.
[Google Scholar]
|
| 5. |
Krathen RA, Orengo IF, Rosen T. Cutaneous metastasis: A meta-analysis of data. South Med J 2003;96:164-7.
[Google Scholar]
|
| 6. |
Sariya D, Ruth K, Adams-McDonnell R, Cusack C, Xu X, Elenitsas R, et al. Clinicopathologic correlation of cutaneous metastases: Experience from a cancer center. Arch Dermatol 2007;143:613-20.
[Google Scholar]
|
Fulltext Views
2,897
PDF downloads
2,827





