Translate this page into:
Obesity-associated lymphedematous mucinosis
2 Department of Pathology, Istanbul Medeniyet University, School of Medicine, Goztepe Research and Training Hospital, Istanbul, Turkey
Correspondence Address:
Ayse Serap Karadag
Department of Dermatology, Istanbul Medeniyet University, School of Medicine, Goztepe Research and Training Hospital, Istanbul
Turkey
| How to cite this article: Karadag AS, Ozlu E, Ozkanli S. Obesity-associated lymphedematous mucinosis . Indian J Dermatol Venereol Leprol 2014;80:456-457 |
Sir,
Obesity-associated lymphedematous mucinosis is a newly recognised entity with only a few patients reported to date. Though this condition can clinically mimic pretibial myxedema, it is differentiated from the latter by microscopic findings and a lack of thyroid disease. [1],[2]
A 71-year-old female presented to us with swelling, erythema, and discoloration on both her legs; these symptoms had been present for 1 year. She had been overweight for 30 years (height 160 cm, weight 95 kg, and body mass index 37.1). Dermatologic examination revealed pink-red plaques on both legs, especially the left leg. Several circular, semi-translucent, papulo-nodular lesions of 1-2 cm diameter were noted surmounting these plaques [Figure - 1]a and b.
Blood tests including total protein, immunoglobulin levels, and thyroid function tests were all normal. No cardiac or renal failure was detected. A skin biopsy taken from a lesion showed a basket-weave stratum corneum with focal hyperkeratosis and mild acanthosis. Dermal edema was noted, with mucin deposition around vessels in the superficial papillary dermis, the deposits staining with PAS, Alcian blue, and mucicarmine stains. Dermal capillaries were increased in number and thickness; perivascular lymphocytes and increased dermal stellate fibroblasts were also seen [Figure - 2]a and b.
 |
| Figure 1: (a and b) Pink-red coloured plaques and several circular, semitranslusent papulonodular lesions on legs |
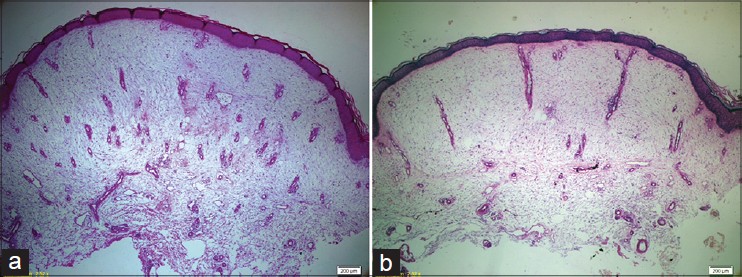 |
| Figure 2: (a and b) Hyperorthokeratosis, mucinous oedema and increased fibroblast of the dermis, increased and thickened capillary vessels, dilated lymphatic vessels (2a: Pas-Alcian Blue, ×100, 2b: Haematoxylin-eosin, ×100) |
The patient was treated initially with pentoxyphylline 400 mg thrice daily and clobetasol 17-propionate 0.05% cream, applied daily for the first month and then on alternate days. After 5 months, since the patient no longer wished to continue with the cream, administration of monthly triamcinolone acetonide (40 mg/mL) injections into the nodular lesions was started. Three months later, the plaques had slightly regressed and the papulonodular lesions were smaller [Figure - 3]. The patient continued to take pentoxyphylline tablets for another 10 months. Meanwhile, she was referred to a dietician and a low-calorie diet was recommended; however, she only lost 3-4 kg. After 10 months of therapy, there was no significant regression of the lesions so further treatment was stopped; the patient is still following up with us.
 |
| Figure 3: Posttreatment appearance |
Mucin accumulation on the legs is usually considered an indicator of pretibial myxedema. [3] In 1993, Somach et al. reported that pretibial myxedema in euthyroid patients may be histologically different from the pretibial myxedema of hyperthyroidism. [2] Then in 2006, Tokuda et al. reported three cases of "chronic obesity lymphedematous mucinosis," [4] where mucin accumulation on the legs accompanying lymphedema had histological findings similar to those reported by Somach et al. Most recently, in 2009, Rongioletti et al. reported five cases of obesity-associated lymphedema with mucin accumulation on the legs. They renamed this entity "obesity-associated lymphedematous mucinosis." [3] The pathogenesis of this condition is unclear but a lymphatic drainage defect may be a cause, [5] leading to excessive high-protein fluid collecting in the interstitium. This in turn could cause thickening of the legs and a peau d′orange appearance. [2]
Clinically, obesity-associated mucinosis is characterized by skin-colored or brown-red papules and/or nodules on an erythematous base on the pretibial region accompanied by edema; rarely, these may occur on the foot or ankle. Patients have long-standing obesity with lymphedema and do not have thyroid disease. Pretibial myxedema, despite being similar, can be differentiated on the basis of histopathological findings and the presence of thyroid disease. Obesity-associated lymphedematous mucinosis shows epidermal atrophy and disappearance of rete ridges with hyper-orthokeratosis, while pretibial myxedema is not associated with epidermal atrophy. [3],[4] Both conditions show varying levels of fibrosis associated with stellate or linear fibroblasts and separation of collagen bundles by mucin. [3],[4] Dermal mucin accumulation is moderate and occurs in the papillary as well as superficial reticular dermis in obesity-associated lymphedematous mucinosis. In contrast, mucin is abundant in the reticular dermis, particularly in the deeper portions, in pretibial myxedema. [3],[4] The dermis in obesity-associated lymphedematous mucinosis also shows vertically running vessels, increased in number and thickness, a feature absent in pretibial myxedema. While hemosiderin deposition may occur, there is no increase in mast cells and inflammatory infiltrate in obesity-associated lymphedematous mucinosis, unlike in pretibial myxedema. [3],[4] Further, dermo-epidermal splitting can be seen in obesity-associated lymphedematous mucinosis but not in pretibial myxedema with thyroid disease. [3],[4]
There is limited information on the treatment of obesity-associated lymphedematous mucinosis as only a few cases have been described. Normalization of thyroid function, topical corticosteroids, plasmapheresis, intravenous immunoglobulin, and octreotide have all been tried in the management of "real" pretibial myxedema, but the approach probably needs to be different for obesity-associated lymphedematous mucinosis. Rongioletti et al. advised two of their 5 patients a low-calorie diet resulting in significant weight loss, and noted marked improvement. [3] In addition to a low-calorie diet, our patient was put on pentoxyphylline, and occlusive topical and intralesional corticosteroids, resulting in a partial if not dramatic response. In conclusion, obesity-associated lymphedematous mucinosis is a newly recognized entity that should be differentiated from pretibial myxedema and other conditions causing secondary mucinosis for appropriate management.
| 1. |
Lynch PJ, Maize JC, Sisson JC. Pretibial myxedema and nonthyrotoxic thyroid disease. Arch Dermatol 1973;107:107-11.
[Google Scholar]
|
| 2. |
Somach SC, Helm TN, Lawlor KB, Bergfeld WF, Bass J. Pretibial mucin. Histologic patterns and clinical correlation. Arch Dermatol 1993;129:1152-6.
[Google Scholar]
|
| 3. |
Rongioletti F, Donati P, Amantea A, Ferrara G, Montinari M, Santoro F, et al. Obesity-associated lymphoedematous mucinosis. J Cutan Pathol 2009;36:1089-94.
[Google Scholar]
|
| 4. |
Tokuda Y, Kawachi S, Murata H, Saida T. Chronic obesity lymphoedematous mucinosis: Three cases of pretibial mucinosis in obese patients with pitting oedema. Br J Dermatol 2006;154:157-61.
[Google Scholar]
|
| 5. |
Yosipovitch G, DeVore A, Dawn A. Obesity and the skin: Skin physiology and skin manifestations of obesity. J Am Acad Dermatol 2007;56:901-16.
[Google Scholar]
|
Fulltext Views
3,945
PDF downloads
2,667





