Translate this page into:
Recurrent blisters in a case of resolving Stevens-Johnson syndrome/toxic epidermal necrolysis
Correspondence Address:
Tsu-Man Chiu
Director of Phototherapy Division, Department of Dermatology, Changhua Christian Hospital, No. 135, Nanhsiao Street, Changhua City, Changhua County 500
Taiwan
| How to cite this article: Chuang YN, Ho YY, Chiu TM. Recurrent blisters in a case of resolving Stevens-Johnson syndrome/toxic epidermal necrolysis . Indian J Dermatol Venereol Leprol 2014;80:546-547 |
Sir,
Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) are rare, potentially life-threatening, mainly drug-induced conditions characterized by widespread apoptosis of keratinocytes provoked by the activation of cell-mediated cytotoxic reaction and amplified by cytokines, mainly granulysin. Dry skin and heat intolerance are common complaints among survivors of SJS/TEN. [1] We report a patient with SJS/TEN overlap who developed recurrence of vesicles and bullae several days after the initial healing of lesions due to sweat retention which simulated a fresh episode of SJS/TEN.
A 51-year-old woman who had rectal cancer with lung and brain metastases was admitted to our burn center because of phenytoin induced SJS/TEN overlap. Phenytoin had been introduced 32 days before the skin rash to control seizures after whole brain radiotherapy. On physical examination, the patient exhibited conjunctivitis, oral mucositis, and generalized maculopapular rash characterized by atypical targetoid lesions with centrally darkened macules and blisters. She was treated with supportive care including empiric antibiotics (piperacillin/tazobactam), nutritional support, fluid and electrolyte replacement, wound dressing, heating lamps to prevent hypothermia, and pain control. After 6 days of treatment, most of the detached skin lesions started to heal gradually without development of new lesions. However, on day 12 of admission, multiple clear water drop-like vesicles and bullae, 1-30 mm in size erupted rapidly on thighs, bathing trunk areas, neck, and arms over 1 day. At that point, there was no new mucositis or targetoid lesion [Figure - 1]. Because new episodes of SJS could not be ruled out, we analyzed the fluid content from blisters for the presence of granulysin which was not detected. Skin biopsy from a new vesicle revealed intracorneal blister overlying eccrine ducts and completely re-epithelialized skin without apoptotic keratinocytes [Figure - 2]. Based on the clinical and histopathologic findings, we hypothesized that the formation of these new blisters was secondary to fluid retention, but not persistent or recurrent SJS/TEN. Furthermore, because the location of new blisters was mainly on areas exposed to heating lamp we hypothesized that excessive sweating contributed to the fluid retention in these blisters. We avoided further use of heating lamps, without any specific treatment for the blisters which spontaneously resolved over the following week.
 |
| Figure 1: Multiple new clear fluid-filled blisters, 1-30 mm in size, erupted rapidly on (a) trunk, (b) arms, thighs, and neck in 1 day during remission stage. Re-epithelialization of the original detached wound could be seen on chest |
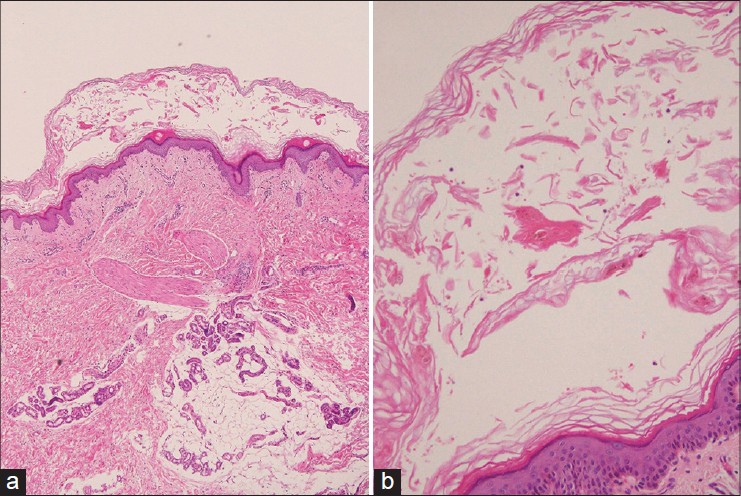 |
| Figure 2: Intracorneal blister overlying eccrine ducts. (H and E, ×40) (b) Only a few neutrophils could be seen in the blister. The base of the blister was completely re-epithelialized, compatible with resolving SJS/TEN. (H and E, ×100) |
Abnormalities of the sweat duct including necrosis of the duct and destruction of the distal duct accompanied by dilatation of the proximal duct have been detected in a histopathologic study of sweat glands in cases of TEN. [2] However, the secretory gland may be normal. Disruption of eccrine ducts during SJS/TEN may lead to sweat accumulation in a potential space between the necrotic epidermis and the newly re-epithelialized skin, predisposing SJS/TEN patients to recurrent blistering during the remission stage. Recently, a case of recurrent blistering in resolving SJS/TEN due to fluid accumulation beneath necrotic epidermis was reported. [3] The author speculated that the result of a positive fluid balance and reduced oncotic pressure from hypoalbuminemia contributed to local fluid accumulation at sites of subclinical epidermal necrosis that were not previously detached. The hydrostatic pressure could also contribute to blister formation in our case. However, the new blister formation in our case occurred mainly on areas exposed to a heat lamp, not on dependent or edematous sites. Thus, we hypothesized that the sweat was the main component of fluid retention in our case, so these blisters could simply be treated by avoidance of excessive sweating caused by heating lamps.
In conclusion, our case highlights that recurrent blistering due to fluid accumulation beneath necrotic epidermis could complicate SJS/TEN, and prompt recognition of this self-limiting and harmless condition is important to avoid unnecessary worry.
Acknowledgement
We acknowledge Wen-Hung Cheng, MD, PhD, the director of Drug Hypersensitivity Clinical and Research Center, Chang Gung Memorial Hospital, Taipei, Taiwan, for analyzing the fluid content.
| 1. |
Kano Y, Shiohara T. Long-term outcome of patients with severe cutaneous adverse reactions. Dermatol Sin 2013;31:211-6.
[Google Scholar]
|
| 2. |
Akosa AB, Elhag AM. Toxic epidermal necrolysis. A study of the sweat glands. J Cutan Pathol 1995;22:359-64.
[Google Scholar]
|
| 3. |
Mahil SK, Martin B, Creamer D, Smith CH. New blisters in a patient treated for Stevens-Johnson syndrome/toxic epidermal necrolysis. Clin Exp Dermatol 2014;39:63-5.
[Google Scholar]
|
Fulltext Views
3,446
PDF downloads
1,644





