Translate this page into:
Psychodermatology: A comprehensive review
Correspondence Address:
Tarun Narang
Department of Dermatology, Venereology and Leprology, Post Graduate Institute of Medical Education and Research, Chandigarh
India
| How to cite this article: Yadav S, Narang T, Kumaran M S. Psychodermatology: A comprehensive review. Indian J Dermatol Venereol Leprol 2013;79:176-192 |
Abstract
Psychodermatology is an interesting domain of dermatology that overlaps with psychiatry. This arena in dermatology has received limited diligence, partly due to lack of training in this realm. We present here a comprehensive review of salient features and treatment updates in primary psychiatric dermatoses and have also discussed the role of psyche in psychophysiological cutaneous disorders. Secondary psychiatric morbidity is relatively common among patients visiting the dermatologists but often overlooked and uncared for. Dermatologist should be able to initiate basic pharmacotherapy, should be knowledgeable about various non-pharmacological treatments and know the right time to refer the patient to the psychiatrist. Awareness and pertinent treatment of psychodermatological disorders among dermatologists will lead to a more holistic treatment approach and better prognosis in this unique group of patients.Introduction
Psychodermatology or psychocutaneous medicine encompasses disorders prevailing on the boundary between psychiatry and dermatology. This domain of dermatology is not new, but has often received limited attention. A survey done via mail to assess the level of training regarding awareness and attitude about this condition among dermatologists revealed a clear understanding of psychodermatology in only 18%, and 39% expressed their interest and willingness to attend any kind of continuing medical education activity on psychodermatologic disorders. [1]
Approximately 30-40% patients seeking treatment for skin disorders have an underlying psychiatric or a psychological problem that either causes or exacerbates a skin complaint. [2] Ample evidence in literature suggests that the course of many skin disorders is affected by stress and psychological events. [3],[4] Disfiguring dermatological conditions often run a chronic course, resulting in profound psychological morbidity, leading to secondary psychiatric disorders (SPsD). [5] These patients need to be addressed with a special approach assisting their psychological need, pharmacotherapy for their psychiatric morbidity, and skin disease; hence, a complete holistic treatment approach to the patient.
The aim of this review was as follows:
- The dermatologist should be able to identify a primary psychiatric disorder (PPsD) with its cutaneous manifestations, assess the extent of role of psychological state influencing the psychophysiologic disorders, and be able to gauge the secondary psychological morbidity in chronic dermatoses.
- Dermatologist should be able to initiate non-pharmacological as well as basic pharmacological treatment for various psychodermatological disorders and must know the ideal time to refer the patient to psychiatrists and the importance of counseling the patient prior to referral.
Pathogenesis
The complex interrelationship between mind and skin has been investigated at both molecular and cellular levels and has been studied extensively. It has been recorded that patients with depression suffer more from physical illness and patients with chronic illness suffer more often from major depressive illness, suggesting that the state of mind has a marked bearing not only on how an illness is perceived but also on its severity and content. [6],[7]
Brain, nerve, and skin are embryologically derived from the neural plate in the ectoderm. The neuro-immuno-cutaneous-endocrine model was proposed by O′Sullivan et al., [8] to explain the mind and body relationship. It forms the basis of many inflammatory cutaneous dermatoses that are triggered or exacerbated by psychological factors. These organs share a complex language of neuropeptides, cytokines, glucocorticoids, and other effecter molecules [Figure - 1]. [8],[9],[10],[11] Hypothalamic pituitary axis (HPA) responds to psychological stress with upregulation of stress hormones (corticotrophin-releasing hormone, adrenocorticotropin releasing hormone, cortisol, and prolactin), sympathetic nervous system activation leading to elevated catecholamine levels, and the release of neuropeptides and neuromediators (substance P and calcitonin gene-related peptide). Skin mast cells are an important target of key stress hormones and mediators, and their activation leads to immune dysregulation and various skin disorders. Arc et al., [11] suggested that skin is exquisitely well innervated and has its own neuro-endocrine system equivalent of the HPA axis local stress response system, which is tightly linked to systemic neuro-endocrine axis. Suarez et al., [12] described in detail the role of psychoneuroimmunology of stress in the pathogenesis of atopic dermatitis.
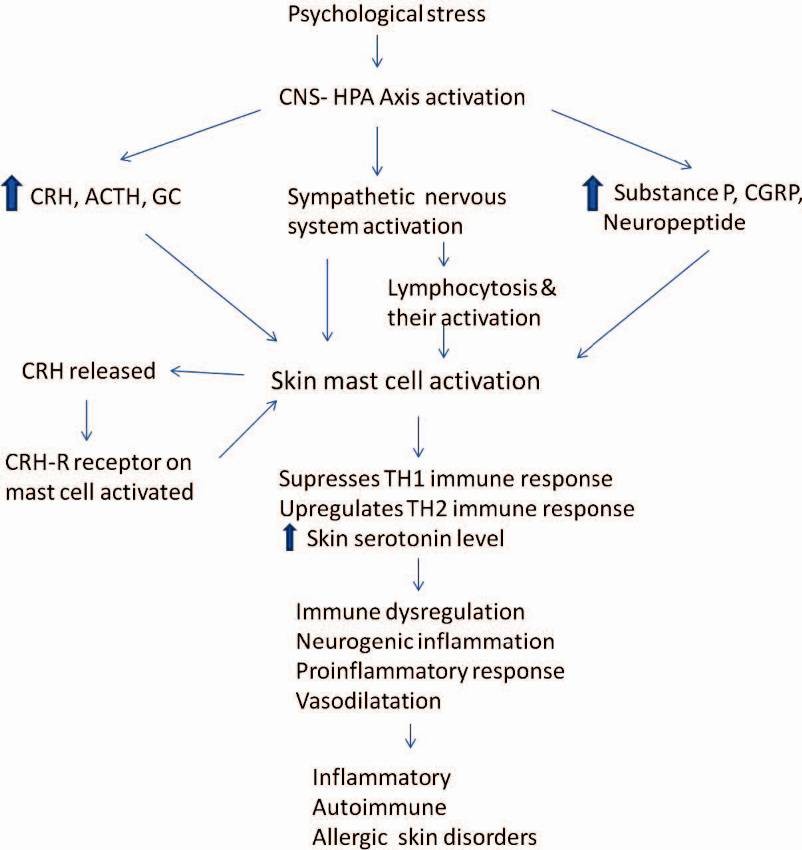 |
| Figure 1: Flow-chart describing interplay of various factors leading to skin disorders originating from psychological stress |
The term and concept of alexithymia introduced by Nemiah and Sifneos [13] is characterized by reduced symbolic thinking, a poor fantasy life, and a limited ability to identify and verbally express emotions,whichresults in altered physiologic and immune body responses. [14] Various studies have reported a high incidence of alexithymia in alopecia areata (58%), [15] psoriasis (35%), [16] chronic urticaria (50%), [17] and vitiligo (35.5%). [18]
Epigenetics is a new concept in the arena of psychiatry that suggests novel pathophysiology and entirely new approach to prevention and treatment of various psychosomatic disorders. [19] Epigenetics suggests that there is a regulation of gene expression via molecular mechanisms (DNA methylation, histone modification, and microRNA dysregulation) in response to environmental stimuli, drugs, and chemicals and that epigenomes reside at the interface between genome and the environment. This field is still in its infancy, but has added newer dimension to our understanding of comorbidity and multimorbidity in psychosomatic medicine. It has great potential to explain how external factors can affect our genes and possibly lead to various diseases.
Classification
Psychodermatologic disorders can be classified under three broad categories [20] : Psychophysiologic disorders, PPsD, and SPsDs.
Psychophysiologic Disorder
Psychophysiological disorders are those in which the course of a given skin disease is affected by the psychological state of a patient. These disorders are often precipitated or exacerbated by emotional stress and/or anxiety in a significant number of cases [Table - 1]. [21],[22],[23],[24],[25],[26],[27],[28] Other skin disorders exacerbated by stress are atopic dermatitis, mucocutaneous herpes simples infection, hyperhidrosis, and chronic telogen effluvium.
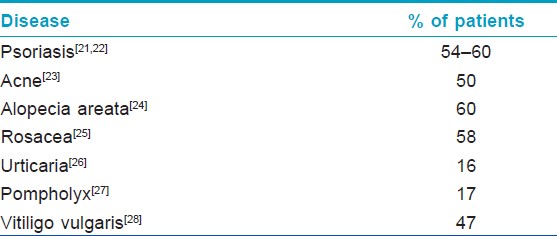
While dealing with these patients, dermatologists should always try to ascertain the extent of role played by psychosocial and occupational stress in a given case to prevent the vicious cycle of stress-disease exacerbation and, finally, deterioration of the primary disease.
These patients generally have a good insight into their diseases, but most are unable to decipher the role of psychological factors on their skin disease. Non-pharmacological as well as pharmacologic therapy such as with benzodiazepines (BDZ) and selective serotonin reuptake inhibitors (SSRIs) are helpful. In non-responders, a psychiatric referral is required and the goal and expected benefit must be discussed with the patient before the referral.
Primary Psychiatric Disorders
PPsD are uncommon, the primary pathology is in psyche, and skin complaints are self-induced and secondary. Dermatologist plays an important role in these disorders, initially to suspect and establish the diagnosis and later to provide appropriate management. [Table - 2] lists the main group′s of PPsDs. Sometimes diagnosis is easy and straight forward, but few PPsD′s may mimic cutaneous disorders; hence, a high degree of suspicion is required to arrive at a proper diagnosis. These patients often have an underlying psychological functional problem such as delusion, obsessive compulsive disorder (OCD), anxiety, depression, impulse control disorder, and personality disorder, which is essential to be identified and managed accordingly. In addition, the supportive skin therapy must be given.
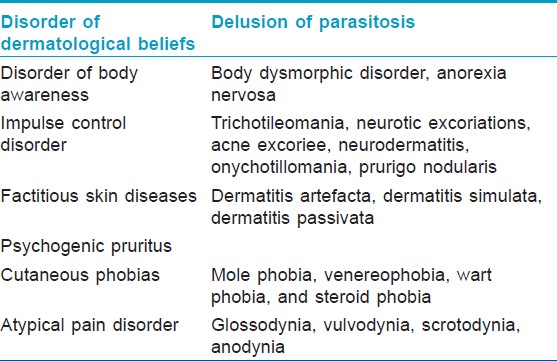
Disorder of Dermatological Beliefs
Delusion of parasitosis
Delusion of parasitosis (DP), also known as Ekbom′s Syndrome, is a rare disorder whose exact prevalence is unknown. DSM-IV-TR defines it as a delusional disorder of somatic type. Hebbar et al., [29] found it to be the most common subtype of delusional disorders. Among 4234 psychiatry outpatients, 1% and 0.5% had delusional disorders and delusional parasitosis, respectively. Here, the patient develops an impervious delusional belief that their bodies are infested with parasites. The underlying psychiatric problem is a "monosymptomatic hypochondriacal psychosis."
Characteristic profile is a middle aged/elderly females presenting in anxious, ruminative, and overwhelmed state after having visited several doctors without satisfaction. The patients narrated about visual and tactile hallucinations of the parasites crawling, burrowing, and biting all over their body. Excoriations are usual and, sometimes, extensively produced in an attempt to extricate the organism. They often presented an evidence of parasite infection in the form of clothing lint, skin crust, or debris, which were misinterpreted as parasite parts, larva, ova, or the entire organism. Morgellons disease has drawn a lot of media attention, but it is largely considered a manifestation of DP by both the dermatologists and psychiatrists.
At the outset, actual infestation must be ruled out first. The differential diagnosis includes psychiatric disorders such as schizophrenia, psychotic depression, psychosis episode in a maniac patient, formication without delusion, organic causes such as withdrawal from cocaine, amphetamines or alcohol, vitamin B12 deficiency, multiple sclerosis, syphilis, and cerebrovascular disease.
These are difficult patients and the dermatologists must express concern, lend a sympathetic ear, and examine the material brought by the patient to establish a good relationship with the patient. Then, the attendants/family of the patient should be counseled regarding the patients illness. Antipsychotic medication can be started by the dermatologist in consultation with psychiatrist before referral.
Disorder of Body Image
Body dysmorphic disorder
Body dysmorphic disorder (BDD), also known as dysmorphophobia or dermatological non-disease, is a disorder characterized by distortion of psychological body image. A patient is preoccupied and distressed with an imagined defect in appearance or an excessive concern over a trivial defect. BDD is defined in DSM-IV and classified as a somatoform disorder. There is an underlying co-morbid mental disorder including mood disorders such as depression, OCD, social phobia, and/or avoidant personality disorder. The intensity with which the patients hold on to their abnormal beliefs is variable. In some patients, the belief is of delusional intensity, then it is classified under psychotic disorders. [30]
Recent evidence suggests that BDD is not very uncommon, having prevalence in many studies varying from 0.75% to 12%. [31],[32] Most patients are females in their 30′s. [31] These patients are rich in symptoms, while poor in signs of organic skin disease. Women present with complaints related to mainly face, breast, hair, nose, and stomach, while men presented with concern related to hair, nose, ear, genitals, and body build. [33] Their thoughts dominated the mind, leading to distress, poor self esteem, and impairment in social, occupational, and domestic functioning. They often perform repetitive compulsive behavior to hide their imaginary/trivial defect. BDD patients are doctor shoppers, they repeatedly undergo procedures to find solution for their flaws and majority are dissatisfied with results and consultation. [34],[35] Suicidal ideation and suicide attempts are common in BDD patients, with studies showing a rate of attempted suicide to the tune of thirty percent. [36] There are two types of patient with BDD: those with insight and those without. Often, those without insight are also diagnosed with delusional disorder, somatic type.
Management of BDD is extremely difficult, every attempt to explain the trivial nature of skin complaints is futile. [37] Most difficult task is to shift the focus from the primary dermatological illness to the one that requires psychiatric treatment. The approach to patients with insight is much like those with trichotillomania, and these patients are relatively easy to manage; they are open to discussion, continue with their medications, and have behavioral modifications unlike those without insight and who are difficult to manage and are treated on the lines of DP.
Impulse Control Disorders
Trichotillomania
The term trichotileomania (TM) literally means a morbid craving/impulsivity to pull out hairs. It is one of the types of traumatic alopecia. The revised DSM-IV diagnostic criteria suggested for TM are: [38] (A) Recurrent pulling out of one′s own hair resulting in hair loss, (B) an increasing sense of tension immediately before pulling out the hair or when attempting to resist the behavior, (C) pleasure, gratification, or relief when pulling out the hair, (D) the disturbance is not better accounted for by another mental disorder, and (E) the disturbance provokes clinically marked distress and/or impairment in occupational, social, or other areas of functioning.
The exact incidence in the general population is not known. In a questionnaire-based survey among college students, incidence was found to be 0.6% among male and female students. [39] There is evidence of bimodal age distribution. Two distinct populations include childhood cases presenting between 5-15 years with a good prognosis and adult cases presenting in later life with a relatively poorer outcome. [40],[41] TM is seven times more common in children as compared to adults. [42] Childhood cases are habitual disorders with no serious psychopathology, sometimes associated with nail biting and thumb sucking. [43] In adults, there is female preponderance, more diversely associated with depression, anxiety disorder, and OCD. [44],[45]
Hair plucking is most common from the scalp and rarely from eyebrows, eyelashes, pubic hair, and torso hair. [44],[45],[46] Hair loss may be minimal to extensive. Typically, hairs are short, broken, irregular in length, distorted, and feel like stubble. The patterns of plucked hair are varied [Figure - 2] and [Figure - 3]. In adults, especially, the loss of hair has psychosocial effects and patients devise means to disguise this defect. Plucked hairs may be stroked, licked, and sometimes swallowed (trichophagia), leading to trichobezoar. [47]
 |
| Figure 2: Extensive scalp involvement in trichotillomania |
 |
| Figure 3: Bizzare pattern of trichotillomania |
Diagnosis is primarily clinical, but scalp biopsy can be done in ambiguous cases. [48] There will be normally growing hairs amongst the empty anagen hair follicles in a non-inflamed dermis. Trichomalacia (distorted and curled hair bulb), bizarre fractured hair shafts, pigment casts, and perifollicular hematoma are fairly specific for TM.
Management in these cases is directed by the age of the patient. [49],[50] Childhood cases have good prognosis. Identification of the stressor, parent education, behavior modification help pre-schoolers to eventually "grow out" of this condition. [51] In adolescents and young adults unaware of their hair pulling, information/awareness of the diagnosis helps in persuading them to seeing a psychiatrist/psychologist and engaging in non-pharmacological management such as cognitive behavioral therapy (CBT). Reassurance that normal hair regrowth is possible if the hair is left alone is also important. Pharmacological management is discussed under the section on treatment. [52],[53]
Neurotic Excoriations
Neurotic excoriations or pathological skin picking is characterized by an unfounded, untamable urge to scratch the skin accompanied by visible tissue damage and functional impairment. [54] There is female preponderance and average age of onset varies between 30 and 50 years. [55] The exact pathophysiology is elusive; however, psychosocial stress precedes exacerbation in around 30-90% cases. [56],[57] There is a compulsive quality and the associated psychological co-morbidity commonly is depression. [54],[55],[56]
The picking can target real blemishes or imaginary flaws. It can involve picking, pulling, poking, prodding, squeezing, or tearing of the skin. It can be episodic, irregular, or constant. Patients pick at areas until they can pull the material out of the skin, also referred as "pulling a thread from the skin." Patients admit to an urge to pick and gouge (unconscious or deliberate) at their skin unlike patients with dermatitis artefacta.
The lesions are polymorphic. Newer lesions are angulated excoriated crusted erosions, while older lesions have depigmented scarred center and hyperpigmented periphery [Figure - 4]. Lesion number vary from few to hundred and are in all stages of development. Prurigo nodularis is an extreme variant of this entity. Distribution of the lesions reflects their self-inflicted nature with lesions concentrated over the most accessible sites.
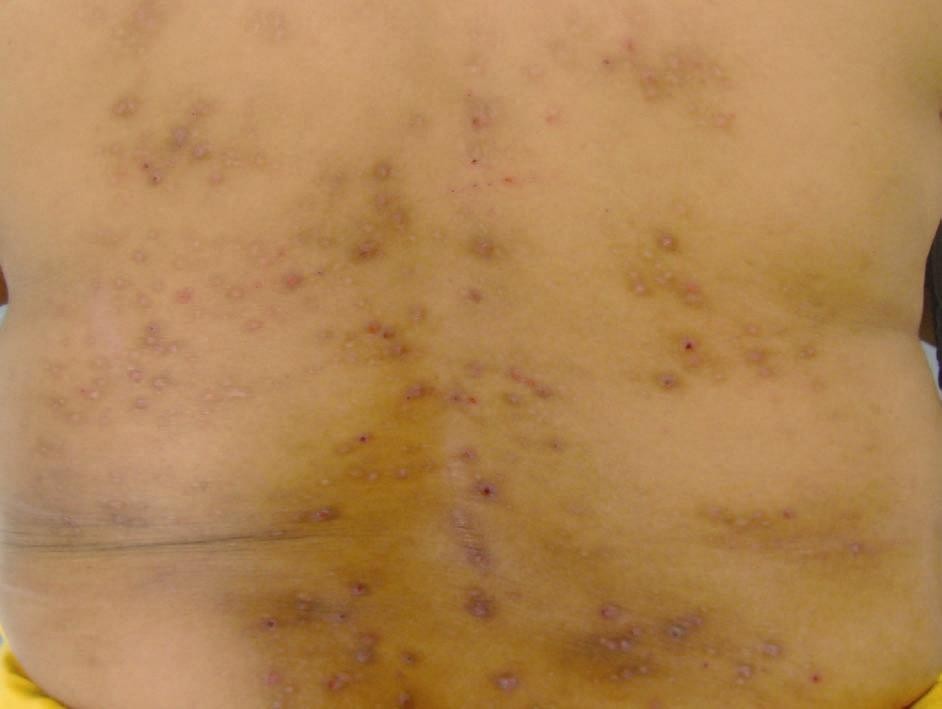 |
| Figure 4: Neurotic excoriation over back with depigmented center and hyperpigmented periphery |
Neurotic excoriation is differentiated from dermatitis artefacta by its conscious and compulsive nature. However, patient should be evaluated for all cutaneous and systemic causes of pruritus before making this diagnosis. Supportive psychotherapy, CBT, and habit reversal programs along with anti-depressants help all patients. [57],[58],[59]
Acne Excoriee
Acne excoriee is a variant of neurotic excoriation where patients either have only facial or predominant facial involvement. Few patients develop lesions after picking acne lesions while majority did not have acne at any time. [60] It is commoner in females with a mean age of 30 years. [60],[61] Psychiatric comorbidity includes BDD, depression, anxiety, OCD, delusional disorder, personality disorder, and social phobias.
Lesions morphologically resemble chronic excoriation or neurotic excoriations and are found predominantly distributed around the hairline, forehead, preauricular cheek, and chin areas [Figure - 5]. If the patient has concomitant acne, aggressive treatment with systemic antibiotic and or systemic retinoids must be considered. Topical non-irritating anti-acne drugs should be prescribed. Rest of the treatment is on the lines of treatment of neurotic excoriation.
 |
| Figure 5: Acne excoriee |
Factitious Skin Diseases
Factitious disorders (ICD-10: F 68.1, L98.1; DSM-IV, 300.16/300.19) are defined as self-harming behaviors that directly or indirectly cause subjective, clinically-relevant harm without being directly linked to suicidal intent. The current classification differentiates between four groups:
- ermatitis artefacta syndrome - as unconscious/dissociated self-injury,
- Dermatitis paraartefacta syndrome: Disorders of impulse control, often as manipulation of an existing specific dermatoses (often semi-conscious, admitted self-injury),
- Malingering: Consciously simulated injuries and diseases to obtain material gain,
- Special forms, such as the Gardner Diamond syndrome, Münchausen syndrome, and Münchhausen by Proxy syndrome.
Dermatitis Artefacta
Dermatitis artefacta (DA) is a skin disease caused by the deliberate action of a fully aware patient on skin, hair, nails, or the mucosa. The DSM-IV-TR criteria for factitious disorder include: [38]
a) Intentional feigning of physical or psychological signs or symptoms, b) The motivation is to assume the sick role, c) External incentives for the behavior (such as economic gain, avoiding legal responsibility, or improving physical well-being, as in malingering) are absent.
Onset in majority is during adolescence or in adults <30 years of age. [62],[63],[64],[65] The female to male ratio varies between 20:1 to 4:1, while in children, there is equal sex incidence. [62],[63],[64],[65] Although reported to be more common in health care workers and their families, recent studies do not suggest the same. [62],[63],[64]
The pathophysiology of DA is poorly understood, but may be multifactorial including complex interplay by genetics, psychosocial factors, and personal/family history of psychiatric illness. [62],[63] The underlying psychopathology is assuming a sick role. Affected children have anxiety disorder or immaturity of coping styles in response to dysfunctional parent-child relationship, bullying, sexual, and substance abuse. [65] Adults may be neurotic, depressed, hysterical, or paranoid personality disorder patients.
The two characteristics of DA are the physical signs and the fabrication. The most common site of involvement is face, followed by dorsum of hands and forearm. [63],[64],[65] The lesions are polymorphic, bizarre, clearly demarcated from the surrounding normal skin and can resemble many inflammatory reactions in the skin. They are crude, angulated, and have the tendency for linear configuration. They are produced by every known means of damaging the skin.
Self-inflicted chemical burn may show a "drip sign." Punched-out necrotic areas or uniform circular blisters or erosions are typical of cigarette burns. Oedema of limbs from tied bands is described as Secretan′s syndrome. [66] Dramatic dermal induration and necrosis occur from foreign body injection of milk, oil, or grease into breasts, thighs, abdomen [Figure - 6], and penis [67] The other common presentation is chronic, non-healing infected wounds. [68] Infectious complications are of serious nature and sometime supervene. [69]
 |
| Figure 6: Dermatitis artefacta following subcutaneous injections with pentazocin mimicking atypical mycobacterial infection |
A patient is unable to provide clear history of evolution of the lesions and typically denies any role in the production of the lesions. [70] Lesions evolve overnight without prior signs and symptoms.
In dermatitis simulata, the patient uses external disguise to simulate a disease, and there is no significant damage to the skin. Make-up has been used to simulate a rash or a birthmark, [71] and topical printing dyes has been used to produce a discolored sweat. [72]
Bizarre crude presentations are easy to diagnose. At times, lesions mimic specific dermatosis, where a skin biopsy must be considered. DA lesions histopathology is usually non-specific, but can sometimes provide supportive information. [73]
Doctor should avoid immediate confrontation regarding the suspicion that the lesions are self-inflicted. [74],[75] This can be counter-productive and the patient may flee from the treatment. Clinician needs to build-up a relationship with the patient by frequent visits, symptomatic treatment, and gradually explore the complex personality and behavioral derangement that underlies this condition.
Munchhausen syndrome is a special form of factitious disorder in which the affected person feigns disease or illness to draw attention or sympathy. Dermatological complaints are uncommon in this syndrome.
Psychogenic Pruritus
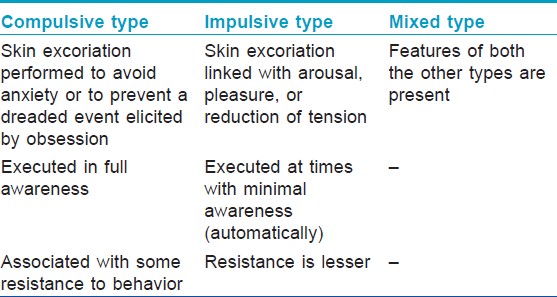
Psychogenic pruritus (PP) is a poorly defined entity in which the patient has intractable or persistant itch, not ascribed to any physical or dermatological illness. Misery et al., [76] have proposed diagnostic criteria [Table - 3]. There are three subtypes of PP [Table - 4].
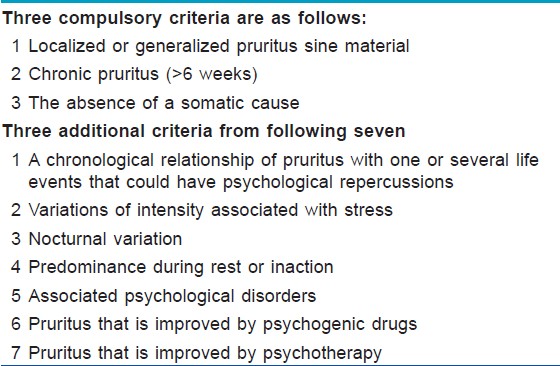
Pruritic episodes are unpredictable with abrupt onset and termination, predominantly occurring at the time of relaxation. PP can be generalized or localized. The commonest sites of predilection are legs, arms, back, and genitals. Often there is history of a major psychological stress preceding the onset of PP. [77] A significant number of patients have associated anxiety and or depression. [78] Detailed cutaneous and systemic examination and routine baseline investigation should be performed to rule out cutaneous and systemic causes of pruritus before diagnosing PP.
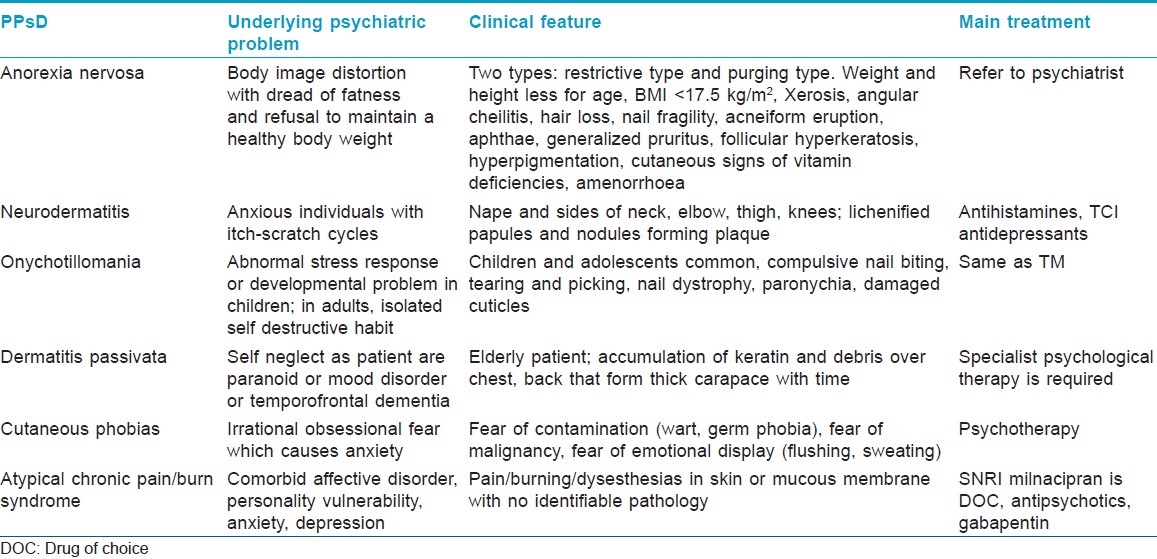
Brief salient features of other PPsD are summarized in [Table - 5].
Dissociative Somatization
Symptoms with no explainable underlying physical pathology are commonly encountered in clinical practice such as unexplained cutaneous sensory syndromes, body memories in post-traumatic stress syndrome that manifest as pruritus, urticaria, or angioedema, self-induced dermatoses such as dermatitis artefacta and trichotillomania associated with dissociative states, and BDD, when the patient has a somatic preoccupation involving the skin or hair. [79] About 20% patients of acne, have aspects of BDD. These patients are more responsive to active non-pharmacological treatments such as exercise and psychotherapy as compared with pharmacological treatment. Drugs with central nervous system action generally are more effective than those that affect peripheral physiologic function. [80]
It should be emphasized that psychiatric referral and consultation should be attempted whenever feasible. Yet, for a significant proportion of patients who refuse psychiatric referral, the judicious use of psychotropic medications by dermatologists may provide much needed assistance in the recovery. However, frequent and regular follow-ups of these patients are required to evaluate clinical response or worsening and adverse effects.
Secondary Psychiatric Disorders
Skin disorders are rarely life threatening, but are associated with significant morbidity and bearing on the quality of life. Overall prevalence of psychological disorders among patients with skin disease is 30-60%. [2] Skin problems, especially chronic skin diseases, affecting exposed body parts because of the visibility and resultant disfigurement lead to embarrassment, depression, anxiety, poor self image, low self esteem, and suicidal ideation in the patients. [81],[82],[83] Also, patients have to commonly face social isolation and discrimination and, at times, have difficulty getting jobs. [84] Many patients are able to cope up with the disease while few develop secondary psychiatric morbidity.
When skin patients were screened for depression, the prevalence of major depressive disorder was found to be 8.4%. [5] The study by Gupta and Gupta showed the prevalence of suicidal ideation as 5.5% and 5.6% in severe psoriasis and acne patients, respectively. [85] Alcohol abuse is more common in psoriasis patients and the amount of daily intake correlates with the severity of psoriasis and its poor response to treatment. [86],[87] Mattoo et al., [88] found 25% of vitiligo patients to have psychiatric morbidity. Majority of the cases had a diagnosis of adjustment disorder. In another study, General Health Questionnaire (GHQ) assessed psychiatric morbidity rates at 33.63% and 24.7% for vitiligo and psoriasis, respectively. [89] Adjustment disorder (56% vs 62%), depressive episode (22% vs 29%), and dysthymia (9% vs 4%) were the most common psychiatric disorders in vitiligo and psoriasis patients, respectively.
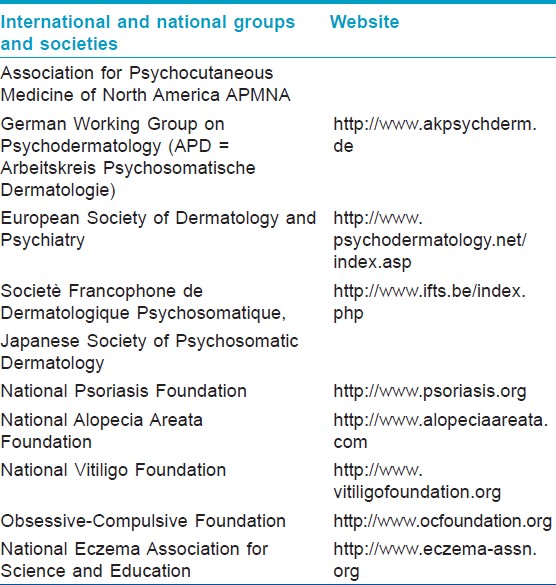
Dermatologist should look into this aspect of chronic disfiguring dermatoses. Most of the time, patients do not discuss the psychological effects of their disease with the treating physician. If the dermatologist suspects significant secondary psychological morbidity then interrogation, counseling, psychiatric referral, and help of dermatologic support group [Table - 6] should be sought.
Management of Psychocutaneous Patients
Most of the patients with psychocutaneous disorders can be broadly categorized under four diagnoses: (a) Anxiety, (b) depression, (c) psychosis, and (d) OCD.
The choice of a psychotropic medication is based primarily on the nature of the underlying psychopathology. The initial and the most important step in successful management of these patients are to establish rapport. It is important to recognize that the patient expects the clinician to treat him or her as having a bona fide skin disease, rather than a psychiatric condition. Patients with psychophysiological disorders or SPsDs usually welcome an opportunity to discuss their psychological status, but patients with PPsDs are extremely resistant to it. [90] It is necessary to start both somatic (i.e., dermatologic) and psychotropic treatment simultaneously in these patients. In PPsD, psychotropic therapy is the mainline of treatment and somatic modalities are supportive. For secondary psychiatric cases, the approach is treating the dermatoses by using a potent therapeutic option because of the great emotional distress suffered by the patient such as the use of isotretinoin for borderline acne with severe psychosocial or occupational impact although there is much debate over the potential psychiatric side-effects of oral isotretinoin as a recent systemic review did not find any conclusive evidence for such an association. [90]
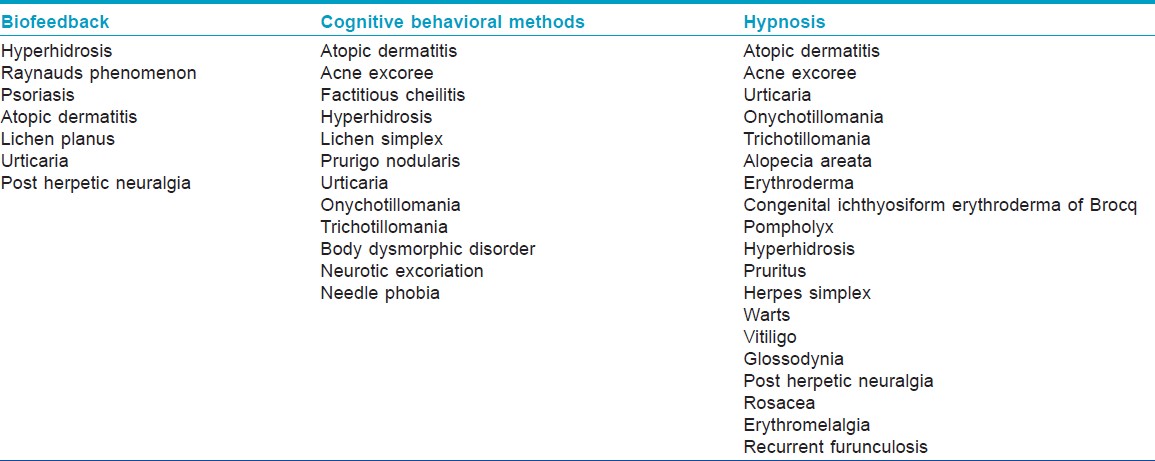
Management includes standard psychotropic drugs, placebo effect, suggestion, cognitive-behavioral methods, biofeedback, and hypnosis. Whenever simple measures fail to produce the results desired, combination of drugs or an addition of non-pharmacological therapy may be required. Psychophysiological skin disorders respond to non-pharmacological therapies that counteract stress, supplemented by anxiolytics, or antidepressants when indicated. Treatment of PPsDs that affects the skin often results in improvement of the associated skin disorders. [90],[91]
Anxiety
Therapeutic modalities for anxiety include BDZ, non-BDZ, and CBT. Risk of dependence on BDZ is quite high; hence, they are indicated only for short-term treatment (2-4 weeks) for severe and disabling symptoms and should be avoided in milder forms. Diazepam, alprazolam, chlordiazepoxide, and clobazam are longer-acting drugs. Lorazepam and oxazepam are shorter-acting compounds with a greater risk of withdrawal symptoms and addiction.
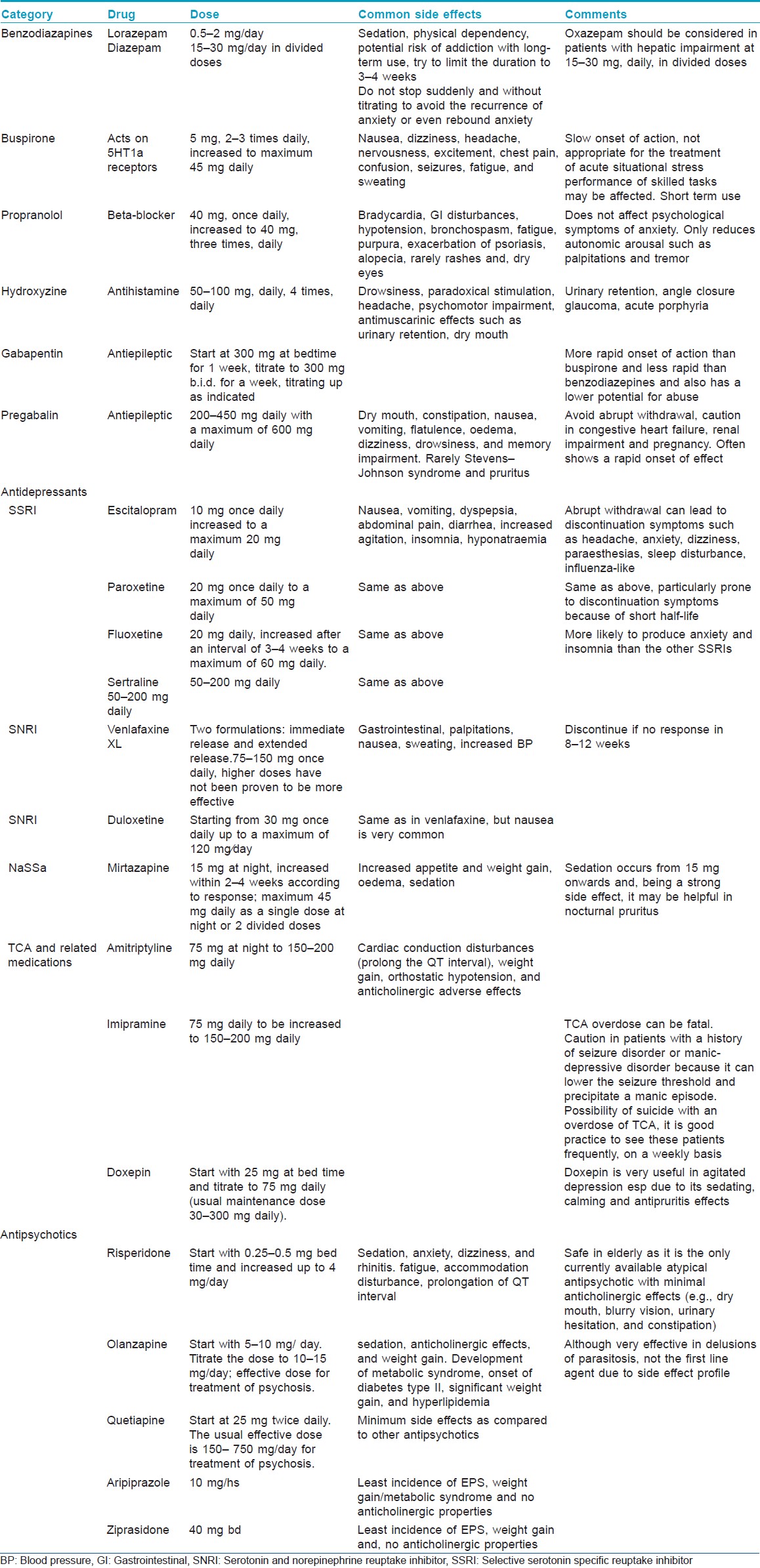
Non-BDZ used in the treatment of anxiety are selective SSRIs (citalopram escitalopram, paroxetine), serotonin-norepinephrine reuptake inhibitors (SNRIs) (venlafaxine XL, duloxetine), antihistamines (hydroxyzine), beta-blockers (propranolol), and the antiepileptic pregabalin [Table - 7]. Antidepressants and pregabalin are non-addictive, but those with a short half-life (paroxetine) may cause discontinuation symptoms when they are stopped abruptly. In the treatment of anxiety, SSRIs may have to be used in a dose higher than that used in depression. Occasionally, an increase in anxiety symptoms may be observed for 1 week when the SSRIs are initiated. [90],[92]
Depression
Depression can be a PPsD or secondary to dermatological condition. Treatment depends on the severity of symptoms; in cases with mild symptoms, if a patient does not wish treatment then watchful waiting or CBT is recommended. Moderate symptoms can be managed with SSRI and CBT. But in cases with severe symptoms and suicidal ideation admission, antidepressants with possibly electroconvulsive therapy (ECT) are recommended. [93]
Currently available antidepressants are equally effective. The clinical response is gradual and usually begins 2-3 weeks after the therapeutic dosage is reached, but for complete therapeutic effectiveness minimum of 6 weeks of full-dose treatment is required. Side-effect profiles and toxicity vary substantially, thus the choice of antidepressant medication depends primarily on tolerability and safety. [90],[92] The antidepressants can be broadly classified as in [Table - 7].
Antipsychotics
Antipsychotics are used in the therapy of psychocutaneous disorders such as delusions of parasitosis, dermatitis artefacta, and monosymptomatic hypochondriasis [Table - 7]. Compliance is the most challenging aspect in the management of these patients, as they lack insight. It is difficult to convince them to participate in a behavioral modification or to seek psychiatric advice. Therefore, the goal of the dermatologist is not to relieve the patients of their delusion, but to help them function better with the delusion.
Second-generation antipsychotics are considered the treatment of choice for patients with psychosis, because of a better side effect profile and compliance. The main side-effects of these agents are sedation and weight gain; however, aripiprazole and ziprasidone are least likely to cause these effects. Risperidone and olanzapine are useful in patients who are rapidly deteriorating or have a severe negative effect on the quality of life. [90],[92],[94]
Obsessive Compulsive Disorder
Disorders like BDD and impulse control disorder (acne excoree, trichotillomania, onychotillomania, neurodermatitis) are treated on the lines of OCD.
The approach to these patients is different from that of the delusional patient, and one may directly confront these patients about their activities. However, we should avoid exacerbating the existing embarrassment in patients. Initially, we should try to build a rapport with them and start by saying "many people develop a habit during stress,… some start smoking, others bite their nails,… and others pull their hair. Have you also been in any kind of stress…?" Once patients develop insight into the etiology of their problem, they are more amenable to see a psychiatrist and engage in non-pharmacological management (CBT). For patients who are unwilling or unable to initiate behavioral modification, pharmacological therapy can be helpful. [95]
Currently, three SSRIs-fluoxetine, paroxetine, and sertraline-are the first-line therapy for the management of OCD. Patients here often require higher doses and more time to respond than those with depression. Initial response to SSRI may require up to 4-8 weeks, and maximal response may take as long as 20 weeks. The response should be assessed after 6 weeks and then the dose is increased for patients with partial response. If the patient does not respond to 10-12 week at therapeutic dosage, a psychiatric referral is required. If it is not feasible then it is advisable to switch to another SSRI. Therapy should be continued for at least 6 months to 1 year once a therapeutic response is achieved. [90],[92] Medications require slow tapering during discontinuation and restarted if symptoms reappear.
Behavioral modification is the cornerstone in the management of OCD, therefore, the most effective treatment is a combination of medication and CBT. However, if patients are resistant to psychiatric referral, they should be encouraged to pursue other resources such as self-help books on habit reversal training and/or self-help groups for OCD. [95]
Non-Pharmacological Treatments
There is a significant psychosomatic/behavioral component in many dermatologic conditions hence complementary non-pharmacological psychotherapeutic interventions like biofeedback, CBT, hypnosis, placebo, and suggestion have positive impacts on many dermatologic disorders. These psychocutaneous modalities cause beneficial modification of immune, autonomic, and endocrine function leading to a decreased release of catecholamines and modification of numerous cytokines and neuropeptides. Moreover, these interventions are reported to enhance compliance with therapeutic regimens, which is a big advantage. [91]
Biofeedback
Biofeedback is a non-invasive conditioning technique with wide applications in the field of medicine. Electromyography (EMG, muscle tension) and blood flow (temperature) training are the most commonly used modalities. Patients are taught relaxation techniques and their effects can be directly observed by the patients in terms of changes in muscle tension, blood flow, heart rate, or other parameters paralleling desired improvements. Patients are often enthusiastic about this modality because the monitoring and feedback displays suggest that they are receiving a high-tech intervention. Besides the auditory or visual feedback endpoints, the patients also experience/observe enhanced feelings of relaxation, well-being, symptom reduction, and an increased patient′s sense of bodily control.
Biofeedback training encompasses a wide variety of progressive muscle-relaxing techniques, autogenic training, imagery techniques, transcendental, and other meditation techniques as well as other relaxation-directed programs (i.e., breathing techniques, self-talk, and others). Relaxation training is primarily directed at minimizing sympathetic reactivity and enhancing parasympathetic function.
Biofeedback is useful in skin disorders that have an autonomic nervous system component, [Table - 8] such as biofeedback of galvanic skin resistance (GSR) for hyperhidrosis and biofeedback of skin temperature for Raynaud′s syndrome. Using biofeedback, individuals may learn consciously how to alter the autonomic response and with enough repetition (20-40 sessions) may establish new habit patterns. Hypnosis or autogenic training may enhance the effects obtained by biofeedback. [91] An example of autogenic imagery training in a patient of psoriasis can be imagery focused on slowing the hyperproliferating keratinocytes by using guided imagery of a calm, serene, beachside/hill station, and the warm, sun gently soothing, and slowing his racing skin cells.
Cognitive Behavioral Therapy
CBT deals with dysfunctional thought patterns (cognitive) or actions (behavioral) that damage the skin or interfere with dermatologic therapy [Table - 8]. In addition to hypnosis, CBT can facilitate aversive therapy and enhance desensitization.
The various steps involved are as follows:
- First identify specific problems by listening to the patient′s verbalization of thoughts and feelings or by observing behaviors
- Determine the goals of CBT such as reduction in anxiety or stop a harmful action
- Develop a hypothesis about the underlying beliefs or environmental events that precede (stimulate), maintain (reinforce), or minimize (extinguish) these thought patterns and behaviors.
- Test the hypothesis of cause and effect by altering the underlying cognitions, the behavior, the environment, or all three, and observe and document the effects on the patient′s dysfunctional thoughts, feelings, and actions.
- Revise the hypothesis if the desired results are not obtained or to continue the treatment if the desired results are obtained until the goals of therapy are reached (modified from Levenson and colleagues [96]).
Hypnosis
Hypnosis is an intentional induction, deepening, maintenance, and termination of a trance state for a specific purpose. Hypnotic trance can be defined as a heightened state of focus that can be helpful in reducing unpleasant sensations (i.e., pain, pruritus, dysesthesias), while simultaneously inducing favorable physiologic changes. Hypnosis may improve or clear many skin disorders. [97] There are many myths about hypnosis; however, the main purpose of medical hypnotherapy is to reduce suffering, promote healing, or help the person alter a destructive behavior. Although the exact mechanism is unknown, it can help to regulate blood flow and other autonomic functions that are usually not under conscious control. The relaxation response during hypnosis alters the neurohormonal systems that in turn regulate many body functions. Hypnosis may be used to help control harmful habits such as scratching. It also can be used to provide immediate and long-term analgesia, reduce pruritus, improve recovery from surgery, and facilitate the mind-body connection to promote healing.
Although psychotherapeutic interventions have come of age and are being incorporated in all spheres of medicine. These non-pharmacological approaches are currently underused and underpromoted in dermatology especially in our country. Selection of patients is very important as there are subsets who are a more resistant and difficult population such as patients with personality disorders including borderline, narcissistic, and schizotypal disorders and patients with any active psychotic process. Therapeutic success in these patients is not as good as expected; however, they are often the ones in the greatest subjective distress and certainly can profit from any of the described interventions. A multipronged approach to the problem is more effective than using only one mode of treatment. While psychoactive drugs have reasonable efficacy in the areas of anxiety, depression, and psychosis, they also have significant side effects. Use of non-pharmacological therapies can often reduce the amount of conventional drugs required, thereby reducing side effects while synergistically contributing to effectiveness. All these interventions require more commitment and lifestyle changes than just swallowing a drug, but the side effects are far less and the benefits often are greater than with a drug.
Complementary Psychocutaneous Therapies
These include herbs and supplements, lavender oil aromatherapy, passion flower, St. John′s wort, S-adenosyl-L-methionine (SAM), and melatonin [Table - 9]. [90],[91],[98],[99] The role of these interventions is rather ill defined and vague. They have been used as anxiolytics, antidepressants, soporifics, and few studies have compared these with standard therapies; however, it is difficult to interpret these studies due to variable results, heterogenous designs, and end points.

An analysis of 29 clinical trials with more than 5000 patients was conducted by Cochrane Collaboration. [100] The review concluded that extracts of St. John′s wort were superior to placebo in patients with major depression. St. John′s wort had similar efficacy to standard antidepressants. The rate of side-effects was half that of newer SSRI antidepressants and one-fifth that of older tricyclic antidepressants. [6] The exact mechanism by which St. John′s wort functions is unclear and subject to conjecture. It′s mechanism is believed to involve inhibition of serotonin (5-HT) reuptake, much like the conventional SSRI′s. The major active antidepressive constituents in St. John′s wort are believed to be hyperforin and hypericin. Standardized extracts are available in the form of tablets, capsules, teabags, and tinctures. Most studies of St. John′s wort for treating depression used doses varying from 300-1,800 mg daily. Similarly, a meta-analysis of studies that compared SAM with controls showed significant clinical improvement with SAM similar to that of the standard SSRI treatment with fewer side effects.
Conclusion
We need to broaden our conception of psychocutaneous medicine. It is not just a collection of specific diagnoses, such as DP and BDD, its main concern is how we relate to our patients. The practical clinical experience in dealing with a delusional or a depressed patient teaches us volumes about these complex and difficult situations and the learning acquired in these difficult cases also extends into the daily and mundane dimensions of our practice. The more we know about psychocutaneous medicine, the better physicians we are. It is important to incorporate a psychological approach to treatment of patients with conditions like psoriasis, vitiligo, acne, or recalcitrant dermatoses.
| 1. |
Jafferany M, Vander Stoep A, Dumitrescu A, Hornung RL. The knowledge, awareness, and practice patterns of dermatologists toward psychocutaneous disorders: Results of a survey study. Int J Dermatol 2010;49:784-9.
[Google Scholar]
|
| 2. |
Picardi A, Abeni D, Melchi CF, Puddu P, Pasquini P. Psychiatric morbidity in dermatological outpatients: An issue to be recognized. Br J Dermatol 2000;143:983-91.
[Google Scholar]
|
| 3. |
Humphreys F, Humphreys MS. Psychiatric morbidity and skin disease: What dermatologists think they see. Br J Dermatol 1998;139:679-81.
[Google Scholar]
|
| 4. |
Capoore HS, Rowland Payne CM, Goldin D. Does psychological intervention help chronic skin conditions? Postgrad Med J 1998;74:662-4.
[Google Scholar]
|
| 5. |
Picardi A, Adler DA, Abeni D, Chang H, Pasquini P, Rogers WH, et al. Screening for depressive disorders in patients with skin diseases: A comparison of three screeners. Acta Derm Venereol 2005;85:414-9.
[Google Scholar]
|
| 6. |
Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci 2011;13:7-23.
[Google Scholar]
|
| 7. |
Johnson TJ, Basu S, Pisani BA, Avery EF, Mendez JC, Calvin JE Jr, et al. Depression predicts repeated heart failure hospitalizations. J Card Fail 2012;18:246-52.
[Google Scholar]
|
| 8. |
O′Sullivan RL, Lipper G, Lerner EA. The neuro-immuno-cutaneous-endocrine network: Relationship of mind and skin. Arch Dermatol 1998;134:1431-5.
[Google Scholar]
|
| 9. |
Slominski A, Pisarchik A, Zbytek B, Tobin DJ, Kauser S, Wortsman J. Functional activity of serotoninergic and melatoninergic systems expressed in the skin. J Cell Physiol 2003;196:144-53.
[Google Scholar]
|
| 10. |
Azmitia EC. Serotonin neurons, neuroplasticity, and homeostasis of neural tissue. Neuropsychopharmacology 1999;21:S33-45.
[Google Scholar]
|
| 11. |
Arck PC, Slominski A, Theoharides TC, Peters EM, Paus R. Neuroimmunology of stress: Skin takes center stage. J Invest Dermatol 2006;126:1697-704.
[Google Scholar]
|
| 12. |
Suárez AL, Feramisco JD, Koo J, Steinhoff M. Psychoneuroimmunology of psychological stress and atopic dermatitis: Pathophysiologic and therapeutic updates. Acta Derm Venereol 2012;92:7-15.
[Google Scholar]
|
| 13. |
Nemiah JC, Sifneos PE. Psychosomatic illness: A problem in communication. Psychother Psychosom1970;18:154-60.
[Google Scholar]
|
| 14. |
Taylor GJ, Bagby RM. New trends in alexithymia research. Psychother Psychosom2004;73:68-77.
[Google Scholar]
|
| 15. |
Sayar K, Köse O, Ebrinç S, Setin M. Hopelessness, depression and alexithymia in young Turkish soldiers suffering from alopecia areata. Dermatol Psychosom 2001;2:12-5.
[Google Scholar]
|
| 16. |
Richards HL, Fortune DG, Griffiths CE, Main CJ. Alexithymia in patients with psoriasis: Clinical correlates and psychometric properties of the Toronto Alexithymia Scale-20. J Psychosom Res 2005;58:89-96.
[Google Scholar]
|
| 17. |
Maniaci G, Epifanio MS, Marino MA, Amoroso S. The presence of alexithymia investigated by the TAS-20 in chronic urticaria patients: A preliminary report. Allerg Immunol (Paris)2006;38:15-9.
[Google Scholar]
|
| 18. |
Picardi A, Pasquini P, Cattaruzza MS, Gaetano P, Melchi CF, Baliva G, et al. Stressful life events, social support, attachment security and alexithymia in vitiligo. A case-control study. Psychother Psychosom2003;72:150-8.
[Google Scholar]
|
| 19. |
Jakovljeviæ M, Reiner Z, Miliciæ D, Crnceviæ Z. Comorbidity, multimorbidity and personalized psychosomatic medicine: Epigenetics rolling on the horizon. Psychiatr Danub 2010;22:184-9.
[Google Scholar]
|
| 20. |
Koo JY, Lee CS. General approach to evaluating psychodermatological disorders. In: Koo JY, Lee CS editors. Psychocutaneous medicine. New York: Marcel Dekker Inc.; 2003. p. 1-29.
[Google Scholar]
|
| 21. |
Fortune DG, Richards HL, Main CJ, Griffiths CE. What patients with psoriasis believe about their condition. J Am Acad Dermatol1998;39:196-201.
[Google Scholar]
|
| 22. |
Manolache L, Petrescu-Seceleanu D, Benea V. Life events involvement in psoriasis onset/recurrence. Int J Dermatol 2010;49:636-41.
[Google Scholar]
|
| 23. |
Poli F, Dreno B, Verschoore M. An epidemiological study of acne in female adults: Results of a survey conducted in France. J Eur Acad Dermatol Venereol 2001;15:541-5.
[Google Scholar]
|
| 24. |
Matzer F, Egger JW, Kopera D. Psychosocial stress and coping in alopecia areata: A questionnaire survey and qualitative study among 45 patients. Acta Derm Venereol 2011;91:318-27.
[Google Scholar]
|
| 25. |
Jaworek AK, Wojas-Pelc A, Pastuszczak M. [Aggravating factors of rosacea]. Przegl Lek 2008;65:180-3.
[Google Scholar]
|
| 26. |
Malhotra SK, Mehta V. Role of stressful life events in induction or exacerbation of psoriasis and chronic urticaria. Indian J Dermatol Venereol Leprol 2008;74:594-9.
[Google Scholar]
|
| 27. |
Lodi A, Betti R, Chiarelli G, Urbani CE, Crosti C. Epidemiological, clinical and allergological observations on pompholyx. Contact Dermatitis 1992;26:17-21.
[Google Scholar]
|
| 28. |
Manolache L, Benea V. Stress in patients with alopecia areata and vitiligo. J Eur Acad Dermatol Venereol 2007;21:921-8.
[Google Scholar]
|
| 29. |
Hebbar S, Ahuja N, Chandrasekaran R. High prevalence of delusional parasitosis in an Indian setting. Indian J Psychiatry 1999;41:136-9.
[Google Scholar]
|
| 30. |
Phillips KA, Menard W, Pagano ME, Fay C, Stout RL. Delusional versus nondelusional body dysmorphic disorder: Clinical features and course of illness. J Psychiatr Res 2006;40:95-104.
[Google Scholar]
|
| 31. |
Otto MW, Wilhelm S, Cohen LS, Harlow BL. Prevalence of body dysmorphic disorder in a community sample of women. Am J Psychiatry2001;158:2061-3.
[Google Scholar]
|
| 32. |
Veale D. Body dysmorphic disorder. Postgrad MedJ2004;80:67-75.
[Google Scholar]
|
| 33. |
Phillips KA, Menard W, Fay C. Gender similarities and differences in 200 individuals with body dysmorphic disorder. Compr Psychiatry2006;47:77-87.
[Google Scholar]
|
| 34. |
Crerand CE, Franklin ME, Sarwer DB. Body dysmorphic disorder and cosmetic surgery. Plastic Reconstr Surg2006;118:167e-80.
[Google Scholar]
|
| 35. |
Veale D, Boocock A, Gournay K, Dryden W, Shah F, Willson R, et al. Body dysmorphic disorder: A survey of fifty cases. Br J Psychiatry1996;169:196-201.
[Google Scholar]
|
| 36. |
Phillips KA, Menard W. Suicidality in body dysmorphic disorder: A prospective study. Am J Psychiatry2006;163:1280-2.
[Google Scholar]
|
| 37. |
Phillips KA. Treating body dysmorphic disorder using medication. Psychiatr Ann2004;34:945-52.
[Google Scholar]
|
| 38. |
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. DSM-IV, 4 th ed. Text revision. Washington DC: American Psychiatric Press, Inc.; 2000.
[Google Scholar]
|
| 39. |
Christenson GA, Pyle RL, Mitchell JE. Estimated lifetime prevalence of trichotillomania in college students. J Clin Psychiatry 1991;52:415-7.
[Google Scholar]
|
| 40. |
Swedo SE, Rapoport JL. Annotation: Trichotillomania. J Child Psychol Psychiatry 1991;32:401-9.
[Google Scholar]
|
| 41. |
Christenson GA, Mackenzie TB, Mitchall JE. Characteries of 60 adult chronic hair pullers. Am J Psychiatry 1991;148:365-70.
[Google Scholar]
|
| 42. |
Keren M, Ron-Miara A, Feldman R, Tyano S. Some reflections on infancy-onset trichotillomania. Psychoanal Study Child 2006;61:254-72.
[Google Scholar]
|
| 43. |
Demaret A. Nail-biting, hair-plucking, and grooming. Ann Med Psychol (Paris)1973;2:235-42.
[Google Scholar]
|
| 44. |
Hautmann G, Hercogova J, Lotti T. Trichotillomania. J Am Acad Dermatol 2002;46:807-26.
[Google Scholar]
|
| 45. |
Cohen LJ, Stein DJ, Simeon D, Spadaccini E, Rosen J, Aronowitz B, et al. Clinical profile, comorbidity, and treatment history in 123 hair pullers: A survey study. J Clin Psychiatry 1995;56:319-26.
[Google Scholar]
|
| 46. |
Radmanesh M, Shafiei S, Naderi AH. Isolated eyebrow and eyelash trichotillomania mimicking alopecia areata. Int J Dermatol 2006;45:557-60.
[Google Scholar]
|
| 47. |
Kohler JE, Millie M, Neuger E. Trichobezoar causing pancreatitis: First reported case of Rapunzel syndrome in a boy in North America. J Pediatr Surg 2012;47:e17-9.
[Google Scholar]
|
| 48. |
Muller SA. Trichotillomania: A histopathologic study in sixty-six patients. J Am Acad Dermatol1990;23:56-62.
[Google Scholar]
|
| 49. |
Dougherty DD, Loh B, Jenike MA, Keuthen NJ. Single modality versus dual modality treatment for trichotillomania: Sertraline, behavioral therapy, or both? J Clin Psychiatry2006;67:1086-92.
[Google Scholar]
|
| 50. |
Bloch MH, Landeros-Weisenberger A, Dombrowski P, Kelmendi B, Wegner R, Nudel J, et al. Systematic review: Pharmacological and behavioural treatment for trichotillomania. Biol Psychiatry2007;62:839-46.
[Google Scholar]
|
| 51. |
Bruce TO, Barwick LW, Wright HH. Diagnosis and management of trichotillomania in children and adolescents. Paediatr Drugs 2005;7:365-76.
[Google Scholar]
|
| 52. |
Gupta MA, Gupta AK. The Use of psychotropic drugs in dermatology. Dermatol Clin2000;18:711-25.
[Google Scholar]
|
| 53. |
Franklin ME, Zagrabbe K, Benavides KL. Trichotillomania and its treatment: A review and recommendations. Expert Rev Neurother 2011;11:1165-74.
[Google Scholar]
|
| 54. |
Flessner CA, Woods DW. Phenomenological characteristics, social problems, and the economic impact associated with chronic skin picking. Behav Modif2006;30:944-63.
[Google Scholar]
|
| 55. |
Fruensgaard K. Neurotic excoriations. Int J Dermatol1978;17:761-7.
[Google Scholar]
|
| 56. |
Gupta MA, Gupta AK, Haberman HF. Neurotic excoriations: A review and some new perspectives. Compr Psychiatry1986;27:381-6.
[Google Scholar]
|
| 57. |
Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs2001;15:351-9.
[Google Scholar]
|
| 58. |
Arnold LM. Phenomenology and therapeutic options for dermatotillomania. Expert Rev Neurother 2002;2:725-30.
[Google Scholar]
|
| 59. |
Bloch MR, Elliott M, Thompson H, Koran LM. Fluoxetine in pathologic skin-picking: Open-label and double-blind results. Psychosomatics 2001;42:314-9.
[Google Scholar]
|
| 60. |
Wrong NM. Excoriated acne of young females. AMA Arch Derm Syphilol1954;70:576-82.
[Google Scholar]
|
| 61. |
Sneddon J, Sneddon I. Acne excoriée: A protective device. Clin Exp Dermatol1983;8:65-8.
[Google Scholar]
|
| 62. |
Millard L. Dermatitis artefacta in the 1990s. Br J Dermatol1996;135:27.
[Google Scholar]
|
| 63. |
Koblenzer CS. Dermatitis artefacta: Clinical features and approaches to treatment. Am J Clin Dermatol 2000;1:47-55.
[Google Scholar]
|
| 64. |
Verraes-Derancourt S, Derancourt C, Poot F, Heenen M, Bernard P. Dermatitis artefacta: Retrospective study in 31 patients. Ann Dermatol Venereol 2006;133:235-8.
[Google Scholar]
|
| 65. |
Rogers M, Fairley M, Santhaman R. Artefactual skin disease in children and adolescents. Australas J Dermatol2001;42:264-70.
[Google Scholar]
|
| 66. |
Smith RJ. Factitious lymphedema of the hand. J Bone Joint Surg Am 1975;57:89-94.
[Google Scholar]
|
| 67. |
Behar TA, Anderson EE, Barwick WJ, Mohler JL. Sclerosing lipogranulomatosis. A case report of scrotal injection of automobile transmission fluid and literature review of subcutaneous injection of oils. Plast Reconstr Surg 1993;91:352-61.
[Google Scholar]
|
| 68. |
Angus JE, Affleck AG, Leach IH, Millard LG. Factitious disease presenting as nonhealing wounds. J Eur Acad Dermatol Venereol 2005;19:70.
[Google Scholar]
|
| 69. |
Murray SJ, Ross JB, Murray AH. Life threatening dermatitis artefacta. Cutis 1987;39:387-8.
[Google Scholar]
|
| 70. |
Vrij A, Mann S. Non verbal and verbal characteristics of lying. In: Halligan P, Bass C, Oakley D, editors. Malingering and Illness Deception. Oxford: Oxford University Press; 2003. p. 351-4.
[Google Scholar]
|
| 71. |
King CM, Chalmers RJ. Another aspect of contrived disease: "Dermatitis simulata". Cutis 1984;34:463-4.
[Google Scholar]
|
| 72. |
MacSween RM, Millard LG. A green man. Arch Dermatol2000;136:115, 118.
[Google Scholar]
|
| 73. |
McSween R, Stevens A, Millard L. Sex, lies and dermatopathology. Br J Dermatol 1996;135:27.
[Google Scholar]
|
| 74. |
Gattu S, Rashid RM, Khachemoune A. Self-induced skin lesions: A review of dermatitis artefacta. Cutis 2009;84:247-51.
[Google Scholar]
|
| 75. |
Koblenzer CS. Dermatitis artefacta. Clinical features and approaches to treatment. Am J Clin Dermatol 2000;1:47-55.
[Google Scholar]
|
| 76. |
Misery L, Alexandre S, Dutray S, Chastaing M, Consoli SG, Audra H, et al. Functional itch disorder or psychogenic pruritus: Suggested diagnosis criteria from the French psychodermatology group. Acta Derm Venereol 2007;87:341-4.
[Google Scholar]
|
| 77. |
Radmanesh M, Shafei S. Underlying psychopathologies of psychogenic pruritic disorders. Dermatol Psychosom2001;2:130-3.
[Google Scholar]
|
| 78. |
Gieler U, Neimeir V. Psychosomatic aspects of pruritus. Dermatol Psychosomat2002;3:6-13.
[Google Scholar]
|
| 79. |
Gupta MA. Somatization disorders in dermatology. Int Rev Psychiatry 2006;18:41-7.
[Google Scholar]
|
| 80. |
Henningsen P, Zipfel S, Herzog W. Management of functional somatic syndromes. Lancet 2007;369:946-55.
[Google Scholar]
|
| 81. |
Saitta P, Keehan P, Yousif J, Way BV, Grekin S, Brancaccio R. An update on the presence of psychiatric comorbidities in acne patients, Part 2: Depression, anxiety, and suicide. Cutis 2011;88:92-7.
[Google Scholar]
|
| 82. |
Shulman LH, DeRogatis L, Spielvogel R, Miller JL, Rose LI. Serum androgens and depression in women with facial hirsutism. J Am Acad Dermatol 1992;27:178-81.
[Google Scholar]
|
| 83. |
Picardi A, Mazzotti E, Pasquini P. Prevalence and correlates of suicidal ideation among patients with skin disease. J Am Acad Dermatol 2006;54:420-6.
[Google Scholar]
|
| 84. |
Adam JE, Weatherhead L. Lamellar ichthyosis in a recluse. Int J Dermatol 1983;22: 427-9.
[Google Scholar]
|
| 85. |
Gupta MA, Gupta AK. Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. Br J Dermatol 1998;139:846-50.
[Google Scholar]
|
| 86. |
86 Hill L, Kennedy P. The role of coping strategies in mediating subjective disability in psoriasis. Psychol Health Med 2002;7:261-9.
[Google Scholar]
|
| 87. |
Gupta MA, Schnork NJ, Gupta AK, Ellis CN. Alcohol intake and treatment responsiveness of psoriasis: A prospective study. J Am Acad Dermatol 1993;28:730-2.
[Google Scholar]
|
| 88. |
Mattoo SK, Handa S, Kaur I, Gupta N, Malhotra R. Psychiatric morbidity in vitiligo: Prevalence and correlates in India. J Eur Acad Dermatol Venereol 2002;16:573-8.
[Google Scholar]
|
| 89. |
Mattoo SK, Handa S, Kaur I, Gupta N, Malhotra R. Psychiatric morbidity in vitiligo and psoriasis: A comparative study from India. J Dermatol 2001;28:424-32.
[Google Scholar]
|
| 90. |
Shenefelt PD. Therapeutic management of psychodermatological disorders. Expert Opin Pharmacother 2008;9:973-85.
[Google Scholar]
|
| 91. |
Fried RG. Nonpharmacologic treatment in psychodermatology. Dermatol Clin 2002;20:177-85.
[Google Scholar]
|
| 92. |
Lee CS, Koo JY. The use of psychotropic medications in dermatology. In: Koo JY, Lee CS, editors, Psychocutaneous medicine. New York: Marcel Dekker; 2003. p. 427-51.
[Google Scholar]
|
| 93. |
National Institute for Health and Clinical Excellence. Depression: Management of Depression in Primary and Secondary Care. Clinical Guideline 23 (Amended). Available from: http://www.nice.org.uk/nicemedia/pdf/CG23quickrefguideamended.pdf. [Last accessed on 2012 Jun 22].
[Google Scholar]
|
| 94. |
Lee CS, Koo J. Psychopharmacologic therapies in dermatology: An Update. Dermatol Clin 2005;23:735-44.
[Google Scholar]
|
| 95. |
Rasmussen SA, Eisen JL. Treatment strategies for chronic and refractory obsessive-compulsive disorder. J Clin Psychiatry 1997;58:9-13.
[Google Scholar]
|
| 96. |
Levenson H, Persons JB, Pope KS. Behavior therapy and cognitive therapy. In: Goldman HH, editor. Review of general psychiatry. 5 th ed. New York: McGraw-Hill; 2000. p. 472.
[Google Scholar]
|
| 97. |
Shenefelt PD. Hypnosis in dermatology. Arch Dermatol 2000;136:393-9.
[Google Scholar]
|
| 98. |
Levin C, Maibach H. Exploration of "alternative" and "natural" drugs in dermatology. Arch Dermatol 2002;138:207-11.
[Google Scholar]
|
| 99. |
Bedi MK, Shenefelt PD. Herbal therapy in dermatology. Arch Dermatol 2002;138:232-42.
[Google Scholar]
|
| 100. |
Linde K, Berner MM, Kriston L. St John′s wort for major depression. Cochrane Database Syst Rev 2008:CD000448.
[Google Scholar]
|
Fulltext Views
19,080
PDF downloads
3,057





